Translate this page into:
What makes non-cirrhotic portal hypertension a common disease in India? Analysis for environmental factors
For correspondence: Dr C.E. Eapen, Department of Hepatology, Christian Medical College, Vellore 632 004, Tamil Nadu, India e-mail: eapen@cmcvellore.ac.in
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
In India, an unexplained enteropathy is present in a majority of non-cirrhotic intrahepatic portal hypertension (NCIPH) patients. Small intestinal bacterial contamination and tropical enteropathy could trigger inflammatory stimuli and activate the endothelium in the portal venous system. Groundwater contaminated with arsenic is an environmental factor of epidemic proportions in large areas of India which has similar consequences. Von Willebrand factor (a sticky protein) expressed by activated endothelium may promote formation of platelet microthrombi and occlusion of intrahepatic portal vein branches leading to NCIPH. Environmental factors linked to suboptimal hygiene and sanitation, which enter through the gastrointestinal (GI) tract, predispose to platelet plugging onto activated endothelium in portal microcirculation. Thus, NCIPH, an example of poverty linked thrombophilia, is a disease mainly affecting the lower socio-economic strata of Indian population. Public health measures to improve sanitation, provide clean drinking water and eliminate arsenic contamination of drinking water are urgently needed. Till such time as these environmental factors are addressed, NCIPH is likely to remain 'an Indian disease'.
Keywords
Endothelial dysfunction
non-cirrhotic portal fibrosis
obliterative portal venopathy
poverty linked thrombophilia
Introduction
A two-part series published in 1967 described a new syndrome of non-cirrhotic portal fibrosis (NCPF) with portal hypertension12. The nomenclature of unexplained portal hypertension without cirrhosis of liver including NCPF, hepatoportal sclerosis, nodular regenerative hyperplasia, idiopathic portal hypertension, incomplete septal cirrhosis and partial nodular transformation of the liver (mostly histology based nomenclature)34 is now regarded as representing aspects of a single clinical entity of non-cirrhotic intrahepatic portal hypertension (NCIPH)56. NCIPH is a vascular disorder of the liver, a consequence of chronic microangiopathy of portal vein branches, leading to intrahepatic portal vein occlusion. In addition to the original description of this disease from India, publication of other seminal research work from India789101112131415 led to the question as to why this disease was so common in India16.
Multifactorial diseases maybe caused by an interplay of multiple acquired and/ or genetic factors. The incidence of NCIPH has been linked to poor sanitation and hygiene, a reflection of living standards in the strata of society affected. As Indian economic development translates into better living standards for its citizens, one can predict that the incidence of NCIPH in India will come down.
An imbalance of low ADAMTS13 (a disintegrin and metalloprotease with thrombospondin type 1 motif, member 13) and high von Willebrand factor (vWF) levels has been documented as example of a mechanistic pathway that would permit poverty-linked environmental triggers to promote obliteration of portal vein radicles in the liver in NCIPH patients1718. ADAMTS13 is an enzyme which cleaves vWF multimers. Uncleaved ultralarge vWF multimers are extremely adhesive and favour platelets to stick onto the activated endothelium. It has been postulated that endothelial activation (vWF is an endothelial protein) leads to platelet plugs in the microcirculation in the liver in NCIPH1718.
This review describes some environmental factors which may explain the predilection of NCIPH for India, and how NCIPH is diagnosed and how NCIPH masquerades (and is often mislabelled) as cryptogenic cirrhosis in India.
Diagnosis of non-cirrhotic intrahepatic portal hypertension (NCIPH)
As the disease process is limited to small intrahepatic portal vein radicles not visualized by currently available imaging techniques, the diagnosis of NCIPH is based on the presence of colour Doppler documenting patent inflow into (portal vein) and outflow out of (hepatic venous outflow tract) the liver, negative aetiological workup for any aetiology of liver disease (e.g. hepatitis B or C virus, iron or copper overload, autoimmune liver disease), liver biopsy documenting absence of bridging fibrosis/cirrhosis and excluding other causes that can closely mimic NCIPH on histology (e.g. schistosomiasis, primary biliary cirrhosis and sarcoidosis)5. History of significant alcohol intake (>20 g/day), risk factors for non-alcoholic fatty liver disease (metabolic syndrome), portal vein thrombosis and hepatic malignancy are exclusion criteria for making a diagnosis of NCIPH.
Role of liver biopsy
Cryptogenic cirrhosis tends to mimic NCIPH and adequate liver biopsy (i.e. containing at least 10 portal tracts with multiple cores) is central to this differentiation. The telltale signs of microangiopathy (portal venule sclerosis/ectasia, sinusoidal dilation, nodular regenerative hyperplasia etc.) are present in a proportion of these patients. For diagnosis of NCIPH, absence of significant fibrosis, i.e. bridging fibrosis/ cirrhosis, is mandatory. Liver biopsy also excludes alternative aetiology (e.g. steatosis, steatohepatitis and significant inflammation) and mimickers of NCIPH (e.g. schistosomiasis and congenital hepatic fibrosis).
Hepatic venous pressure studies
Hepatic venous pressure measurements (balloon or catheter wedge technique19) can help differentiate cirrhosis from NCIPH. As the disease process (and the gradient) in NCIPH is presinusoidal, hepatic venous pressure gradient (HVPG) is expected to be normal in these patients. However, this is true only in one-third of the patients with NCIPH, and the rest tend to have higher than normal HVPG5.
Is NCIPH still present in India?
Initial detailed reports from India described and established NCPF as a disease entity12. Multiple reports corroborate the fact that NCIPH remains prevalent in India20212223. Table I presents some of the recent studies from India reporting the prevalence of NCIPH15202425262728. The prevalence greatly varies depending on the group of patients studied and modalities used for diagnosis.
| Year | Study | Nature of study | Patient population (n) | Prevalence of NCIPH (%) | Basis of diagnosis of NCIPH |
|---|---|---|---|---|---|
| 1991 | Bhargava et al24 | Prospective | Portal hypertensive bleed (404) | 20.5 | Liver biopsy |
| 2001 | Dhiman et al15 | Retrospective | Portal hypertension (>2000) | 15 | Liver biopsy only in a proportion |
| 2008 | Poddar et al25 | Retrospective | Paediatric portal hypertension (517) | 2 | Liver biopsy |
| 2009 | Simon et al26 | Retrospective | Paediatric portal hypertension (171) | 3.5 | Liver biopsy |
| 2009 | Madhu et al27 | Retrospective | Adult cryptogenic portal hypertension (62) | 48 | Liver biopsy |
| 2012 | Nayak et al28 | Retrospective | Adult liver transplant (372) | 2.4 | Liver biopsy |
| 2013 | Goel et al20 | Prospective | Adult portal hypertension (583) | 2.7 | Liver biopsy |
Several new patients with NCIPH have been diagnosed and reported29 from a tertiary centre, catering predominantly to middle/ lower socio-economic class patients from southern and eastern parts of India every year (Figure).
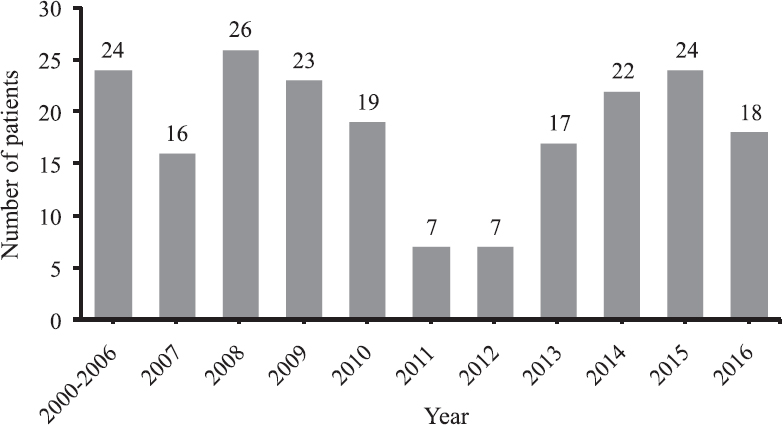
- Number of new non-cirrhotic intrahepatic portal hypertension (NCIPH) patients (liver biopsy proven) diagnosed in a single tertiary centre in southern India from 2000 to 2016 (unpublished data).
Are we underdiagnosing NCIPH?
NCIPH mimics cryptogenic cirrhosis in every aspect, and as mentioned previously, diagnosis of NCIPH requires extensive evaluation. Diagnosis of NCIPH is confirmed only with liver biopsy30, and often, the diagnosis is made with explant biopsy after transplant for presumed cryptogenic cirrhosis531. Sampling the liver for biopsy is often difficult to achieve in a patient with, often severe, thrombocytopenia. In a prospective study spanning one year from our tertiary centre, although cryptogenic chronic liver disease was the most common aetiologic label noted in 203 of 583 (35%) portal hypertensive patients, only 39 (19%) patients were subjected to liver biopsy evaluation20.
Most centres in India have limited access to transjugular liver biopsy and hepatic venous pressure measurement. In addition, pathogenesis of NCIPH remains poorly understood and consequently has limited treatment options available. As oesophageal and gastric variceal bleeds are now almost exclusively managed by endotherapy, shunt surgeries are rarely performed for portal hypertension. As a consequence, peroperative liver biopsy (common method of liver sampling for histology previously for NCIPH) is hardly ever done now in India122027.
Madhu et al27, in a retrospective analysis of liver biopsy in patients with previously labelled as cryptogenic cirrhosis, noted that 48 per cent had NCIPH. Another prospective study20 noted 41 per cent prevalence of NCIPH in patients undergoing liver biopsy for cryptogenic cirrhosis. Although there may be a selection bias, yet it is more than likely that NCIPH forms a significant subset of Indian portal hypertensive patients who are currently labelled as cryptogenic cirrhosis. It has been estimated that in India, 10-30 per cent patients with portal hypertensive bleeds may have underlying NCIPH32.
Role of potential environmental factors in NCIPH patients
Poverty
‘Poverty-linked thrombophilia’ is probably secondary to environmental factors, especially related to gut inflammation5. In a prospective study it was noted that most patients with NCIPH belonged to low and middle socio-economic status20. Limited access to clean drinking water, inadequate sewage facilities and continued close existence with animals contribute to a state of mild gut inflammation (environmental enteropathy) in India33. This chronic low-grade gut inflammation creates a pro-thrombotic milieu in portal circulation and can drive NCIPH5.
Enteropathy
Microangiopathy restricted to intrahepatic small portal vein radicles suggests the active involvement of gut in the pathogenesis of NCIPH. An animal model of NCIPH has been created by repeatedly injecting Escherichia coli into portal circulation34. Often silent gut disorders (celiac disease and ulcerative colitis) accompany NCIPH35. The presence of these disorders was also associated with worse outcome. Higher plasma titres of IgA anti-cardiolipin antibodies36 and deposition of IgA2-complement complexes in the kidneys of NCIPH patients who developed nephrotic syndrome after splenorenal shunt37 also suggest the dominant role of gut in pathogenesis of NCIPH.
Tropical sprue was initially reported in residents of India, as well as visitors to India as a cause of malabsorption38. The epidemiology of tropical sprue in India has changed over the past several decades. Epidemics of tropical sprue are no longer reported in India. Sporadic cases of tropical sprue still constitute the main cause of malabsorption in many centres in India39404142. Tropical enteropathy (subclinical malabsorption) is common in India. Xylose malabsorption was documented in 50 per cent of the apparently healthy population in southern India43. Despite elaborate investigations and researching putative causes44, the definitive cause of tropical sprue has never been identified. It has been postulated that tropical enteropathy may be an adaptive response to recurrent intestinal infections45.
It is possible that with improving sanitation, the causative environmental factor(s) may have got attenuated. However, the sporadic cases of tropical sprue suggests that the environmental causative factors are still present in India. Small intestinal bacterial overgrowth occurs in patients with tropical sprue46. Low-grade small intestinal bacterial growth is common in patients with non-alcoholic fatty liver disease in India47. Celiac disease is now increasingly recognized in India. Its prevalence varies with the wheat-consuming habits of the population48. The association of (asymptomatic) celiac disease and NCIPH has been reported354950.
Systematic studies looking for enteropathy in NCIPH patients unearthed an unexplained enteropathy, significantly higher in NCIPH patients compared to patients with hepatitis B or C causing portal hypertension (disease controls) as well as in healthy controls50. Further research is needed to explore this as yet unexplained enteropathy in NCIPH patients. Of the different types of gut disorders discussed above, it is likely that some disorders - tropical sprue, tropical enteropathy, small bowel bacterial overgrowth – affect individuals in lower socio-economic strata of society who are more exposed to the consequences of suboptimal sanitation51.
Arsenicosis
The link between therapeutic arsenic use (Fowler's solution - arsenic trioxide - used to treat psoriasis) and non-cirrhotic portal hypertension was initially reported from Europe52. Chronic arsenicosis is a multisystem disorder and skin is most commonly involved (melanosis and keratosis); other organs involved include peripheral nerves, liver, lungs, etc. NCIPH is the typical hepatic manifestation5354. In long-standing cases, cancer (of skin, lungs, liver, kidney and urinary bladder) can develop5556. In affected locations, children in addition to adults are affected2357.
In 1970s, Datta et al10 reported the link between chronic arsenicosis and NCIPH in India. These patients had consumed arsenic from three sources: consumption of groundwater contaminated with arsenic; use of arsenic mixed with opium (illegal recreational drug) and Ayurvedic medicines (bhasams prepared by repeated oxidation of ores) containing arsenic.
Ground water contamination by arsenic
The entire Ganga River basin covering large areas of land in India, Bangladesh, Nepal and Tibet, has high levels of arsenic in groundwater, water used for irrigation and in food materials. The arsenic levels here are in excess of World Health Organization standards for drinking water and United Nations Food and Agricultural Organization's standard for irrigation water (100 μg/l)58. Arsenic contamination of groundwater and water used for drinking continues to be documented on a significant scale in Bihar59, Uttar Pradesh60 and West Bengal61. In Kolkata Municipal Corporation, the southern parts of the Corporation face a higher degree of groundwater arsenic contamination62.
The population affected by arsenic in India in 2018 was estimated to be 1.48 crores62. The States maximally affected are West Bengal (1.04 crore affected persons), Bihar (16.88 lakh affected) and Assam (14.48 lakh affected). In West Bengal, the ground water contamination by arsenic is recognized in 83 blocks in eight districts (Bardhaman, Malda, Hooghly, Howrah, Murshidabad, Nadia, North 24 Parganas and South 24 Parganas)62. Subclinical arsenicosis (higher level of arsenic in hair, nail or urine samples, with no overt clinical manifestations) was seen in >90 per cent of adults and children studied, residing in the affected localities55. Typical skin lesions of arsenicosis (hyperpigmentation and keratosis) were seen in 10 per cent of adults and six per cent of children from these localities (Uttar Pradesh, Bihar and West Bengal) who were examined596061. Individuals residing in these localities and consuming arsenic-laden drinking water continue to be diagnosed with NCIPH63.
Prevention of arsenic poisoning in India
The technology needed to remove arsenic from groundwater is expensive. Attempts to treat NCIPH with arsenic chelating agents have shown limited success64. The urgent need is to educate the public about the arsenic contamination of groundwater. Adequate infrastructure is needed to treat and provide arsenic free drinking water. The water supply needs to be continuously monitored for arsenic contamination. Rainwater harvesting (thus avoiding use of contaminated groundwater) is another suggested option. Cost-effective arsenic mitigation programmes which can be sustained with public participation for implementation are urgently needed5865.
Use of arsenic mixed in recreational drugs and Ayurvedic/alternative medicines
A survey from Chandigarh showed highly prevalent use of substances including that of opioids66. Dependence rates on opioids, cannabinoids and sedative hypnotics were 1.5 per cent. The association between use of arsenic containing Ayurvedic medicines, arsenicosis and NCIPH has been reported in India67. In patients who develop drug-induced liver injury due to these drugs, the presence of arsenic or mercury is found to be associated with a higher risk of death68.
Animal models of liver damage in arsenicosis
Chronic ingestion of arsenic (over 15 months duration of arsenic exposure) leads to hepatic fibrosis in mice. Oxidative stress in the liver has been demonstrated in murine model of arsenicosis causing hepatic fibrosis69. The lack of progression to portal hypertension in mice exposed to arsenic for prolonged periods suggests that arsenic exposure alone is not sufficient to produce NCIPH in mice70.
Hypovitaminosis B12
Vitamin B12 deficiency is common in general population of India71. Low serum vitamin B12 may be due to subclinical malabsorption (like tropical enteropathy), genetic variations or low intake (vegetarianism)40717273. Low serum vitamin B12 level in patients with unexplained portal hypertension is a marker of NCIPH74. Low serum vitamin B12 predicts lack of advanced hepatic fibrosis in patients with intrahepatic portal hypertension75. Whether vitamin B12 deficiency (and consequent hyperhomocysteinemia) has a pathogenic role in causing portal venous obliteration in NCIPH is unclear at present. In a study from West Bengal, the degree of arsenic contamination of drinking water correlated with low serum vitamin B12 levels in the population consuming this water76. Whether B12 deficiency predisposes to NCIPH in areas with endemic arsenicosis in India needs further study.
Table II summarizes the findings of various case-control and observational studies regarding the prevalence of potential environmental factors in patients with NCIPH in India.
| Environmental factor | Study and year | Type of the study | Patients studied | Parameter studied | Findings (%) | P |
|---|---|---|---|---|---|---|
| Arsenicosis | Mazumder et al, 199854* | Observational | 156 (with arsenicosis) | Spectrum of liver disease | 41 (26) had NCIPH | - |
| Datta et al, 197910# | Case-control | Cases: 9 Controls: 7 | Liver arsenic content | Cases: 0.9±0.40 ppm Controls: 0.18±0.17 ppm | <0.01 | |
| Goel et al, 201663 | Case-control | Cases: 27 Controls: 25 | Arsenicosis (dermatological) | Cases: 3 (11) Controls: 0 | 0.2 | |
| Enteropathy | Maiwall et al, 2014 (Unexplained enteropathy)50 | Case-control | Cases: 12 Controls: 59 | Celiac serology and duodenal biopsy | Cases: 11 (92) Controls: 6 (10) | <0.001 |
| Maiwall et al, 2014 (Celiac disease)50 | Case-control | Cases: 14 Controls: 59 | Celiac serology and duodenal biopsy | Cases: 2 (14) Controls: 0 | 0.04 | |
| Hypo- vitaminosis B12 | Goel et al, 201374 | Case-control | Cases: 42 Controls: 38 | Low vitamin B12 levels (<250 pg/ml) | Cases: 14 (33) Controls: 1 (3) | <0.001 |
*Of the 156 patients with skin arsenicosis, 33 per cent had portal hypertension and 41 patients had liver biopsy findings suggesting NCIPH54; #Nine liver biopsy specimens of patients with NCIPH had higher liver arsenic content as compared to seven cirrhosis controls, nine still born infants and 18 normal liver controls
Mechanistic pathway
Platelet sequestration occurs in spleen and liver in healthy individuals as well as in syndromes of splenomegaly7778. Platelet sequestration onto endothelium is one mechanism of thrombocytopenia in patients with portal hypertension. Marked, at times symptomatic, thrombocytopenia is a characteristic feature of NCIPH. Platelet sequestration onto the activated endothelium in portal vein branches in the liver is postulated as a pathogenic mechanism of NCIPH5.
Plasma vWF levels are raised (reflecting endothelial activation) in NCIPH patients. Release of pro-inflammatory cytokines in response to the chronic inflammatory stimulus from the intestine can activate the endothelium to release vWF into portal circulation7980. It is likely that chronic low-grade inflammatory stimuli released from the gut trigger vWF expression on portal venous endothelium, with potential to promote platelet sequestration and occlusion of portal vein radicles causing NCIPH. ADAMTS13 is a vWF-cleaving protease synthesized almost exclusively by hepatic stellate cells. In advancing cirrhosis, as liver synthetic functions decrease, the plasma levels of ADAMTS13 also decrease. In a study of 142 hepatitis C-infected patients, mean plasma ADAMTS13 levels were 87, 79, 63 and 31 per cent in chronic hepatitis, cirrhosis in Child's A, B and C classes, respectively. Severe ADAMTS13 deficiency was seen in five patients in Child's C cirrhosis81. In contrast, two studies of NCIPH patients from Birmingham, UK17 and at Vellore, India18 have documentedsevere ADAMTS13 deficiency in 10 to 28 per cent despite most patients having well-preserved liver functions. This suggests that ADAMTS13 deficiency may be a primary event and involved in pathogenesis of NCIPH; in contrast to being a secondary phenomenon due to reduced liver synthetic function in advanced cirrhosis because of hepatitis C. The association of ADAMTS13 deficiency in NCIPH patients is being increasingly recognized82.
Genetic predisposition to NCIPH
Prevalence of familial NCIPH
There have been isolated reports of NCIPH occurring in childhood and families suggesting a possible role of genetic predisposition83848586878889. In a retrospective analysis of prospectively collected database of 174 NCIPH patients (age at presentation: 32±12 yr) at our centre, only three patients had another 1st degree family member having a chronic liver disease29. In a large Western study on natural history of NCIPH, none of the 69 patients reportedly had a family history of liver disease90. Thus, familial NCIPH appears to be uncommon.
Genetic alterations in NCIPH
Multiple studies have attempted to explore the role of genetic influence in pathogenesis of NCIPH. Whole exome sequencing in familial NCIPH revealed potential pathogenic mutations needing further studies9192. Studies have attempted to analyze possible genetic influences such as immunogenetic (major histocompatibility complex), thrombophilic and metabolic (especially drug susceptibility) in pathogenesis of NCIPH939495969798. Except for in isolated families affected by NCIPH, there are not enough data at present to suggest a monogenic cause in majority of these patients.
Genetic predisposition to microangiopathy
NCIPH may be considered as a localized form of thrombotic microangiopathy affecting the small portal vein radicles as there is evidence of low ADAMTS1351718, and alternative complement system activation99100, being involved in its pathogenesis. In addition, low ADAMTS13 is associated with enhanced complement activation, especially in alternative pathway101. Both mutations in ADAMTS13 and the complement regulators are known to predispose to thrombotic microangiopathy102103104105.
A rare non-synonymous variant in ADAMTS13 gene (CUB domain, rs2301612) was detected in a single patient with NCIPH (absent in 20 healthy controls) in a study at our centre, which was associated with ADAMTS13 protein trapping inside the hepatic stellate cells and also decrease in functional activity106. East Asians have been shown to harbour polymorphisms that lead to decrease in ADAMTS13 activity, which can make the population vulnerable to develop thrombotic microangiopathy in the presence of a second insult107.
There is evidence to suggest complement activation (primary or secondary), especially alternative complement pathway may play a role in pathogenesis of NCIPH100. Thrombotic microangiopathy is known to be associated with mutations in alternative complement pathway108. These mutations render the alternative complement system hyperactive with loss of natural suppression. In a recent case-control study on 21 patients with NCIPH (compared with healthy controls), we found no significant association with a single nucleotide polymorphism at rs6677604 (polymorphism associated with decrease in complement factor H and known to predispose to thrombotic microangiopathy)109.
Is the epidemiology of NCIPH changing in India?
Decline in incidence of NCIPH has been reported from some centres in India110111. However, multiple reports in the past decade corroborate the fact that NCIPH remains prevalent in India2023252728112. NCIPH mimics cryptogenic cirrhosis113. As discussed earlier, NCIPH is currently underdiagnosed in India.
Causes of NCIPH in different parts of the world
The factors triggering NCIPH are diverse114. In the West, haematological and malignant thrombophilic disorders are often associated with NCIPH90115. Association of NCIPH with certain drugs (most commonly azathioprine and some anti-retroviral drugs) have often been reported96116117118. Such association have not been reported from India, but widespread use of herbal products needs to be considered118. In India, gut derived environmental factors are probably the predominant triggers of NCIPH at present.
Future directions
The available evidence showed that deleterious environmental factors, entering the portal venous system through the gut, could promote endothelial-platelet interaction leading to occlusion of intrahepatic portal vein radicles in NCIPH. While it is likely that all socio-economic categories in India are exposed to these environmental factors, the impact may be more prominent in the lower socio-economic categories. Urgent public health measures to improve hygiene and sanitation are needed to reduce incidence of NCIPH. Governmental initiatives such as Swatch Bharat Mission or Clean India Mission119, National Mission for Clean Ganga120, Task Force to reduce Arsenicosis121 as well as community-led initiatives122 in this regard are likely to contribute to reduction of NCIPH in India, in the days to come.
Financial support & sponsorship: Authors acknowledge funds received from the Science and Engineering Research Board, Government of India (EMR/2015/000570) and Fluid research funds, Christian Medical College, Vellore, India, towards conduct of these studies into non-cirrhotic portal hypertension.
Conflicts of Interest: None.
References
- Non-cirrhotic portal fibrosis with portal hypertension: A new syndrome. I. Clinical and function studies and results of operations. Indian J Med Res. 1967;55:336-50.
- [Google Scholar]
- Non-cirrhotic portal fibrosis with portal hypertension: A new syndrome. II. Histopathological studies. Indian J Med Res. 1967;55:351-9.
- [Google Scholar]
- Histopathology of the liver in non-cirrhotic portal hypertension of unknown aetiology. Histopathology. 1996;28:195-204.
- [Google Scholar]
- Partial nodular transformation of the liver with portal hypertension. Am J Med. 1966;40:195-203.
- [Google Scholar]
- Idiopathic non-cirrhotic intrahepatic portal hypertension (NCIPH)-newer insights into pathogenesis and emerging newer treatment options. J Clin Exp Hepatol. 2014;4:247-56.
- [Google Scholar]
- Noncirrhotic intrahepatic portal hypertension: Towards a unifying definition and etiology. Indian J Gastroenterol. 2014;33:308-9.
- [Google Scholar]
- Obliterative portal venopathy of the liver. Associated with so-called idiopathic portal hypertension or tropical splenomegaly. Arch Pathol. 1969;87:359-69.
- [Google Scholar]
- Ultrastructure of the liver in non-cirrhotic portal fibrosis with portal hypertension. Gut. 1970;11:905-10.
- [Google Scholar]
- Chronic oral arsenic intoxication as a possible aetiological factor in idiopathic portal hypertension (non-cirrhotic portal fibrosis) in India. Gut. 1979;20:378-84.
- [Google Scholar]
- Measurement and correlation of wedged hepatic, intrahepatic, intrasplenic and intravariceal pressures in patients with cirrhosis of liver and non-cirrhotic portal fibrosis. Gut. 1987;28:260-6.
- [Google Scholar]
- Effect of shunt surgery on spleen size, portal pressure and oesophageal varices in patients with non-cirrhotic portal hypertension. J Gastroenterol Hepatol. 1997;12:582-4.
- [Google Scholar]
- Study of portal hypertension in children with special reference to sclerotherapy. Trop Gastroenterol. 1997;18:119-21.
- [Google Scholar]
- Non-cirrhotic portal fibrosis (idiopathic portal hypertension): Experience with 151 patients and a review of the literature. J Gastroenterol Hepatol. 2002;17:6-16.
- [Google Scholar]
- Non-cirrhotic portal hypertension: Why is it so common in India? J Gastroenterol Hepatol. 2002;17:1-5.
- [Google Scholar]
- Idiopathic noncirrhotic intrahepatic portal hypertension is associated with sustained ADAMTS13 deficiency. Dig Dis Sci. 2011;56:2456-65.
- [Google Scholar]
- ADAMTS13 deficiency, despite well-compensated liver functions in patients with noncirrhotic portal hypertension. Indian J Gastroenterol. 2014;33:355-63.
- [Google Scholar]
- Measurement of hepatic venous pressure gradient revisited: Catheter wedge vs. balloon wedge techniques. Indian J Radiol Imaging. 2011;21:291-3.
- [Google Scholar]
- A study of aetiology of portal hypertension in adults (including the elderly) at a tertiary centre in Southern India. Indian J Med Res. 2013;137:922-7.
- [Google Scholar]
- Noncirrhotic portal fibrosis in pediatric population. J Pediatr Gastroenterol Nutr. 2017;64:748-53.
- [Google Scholar]
- Management of hypersplenism in non-cirrhotic portal hypertension: A surgical series. Hepatobiliary Pancreat Dis Int. 2012;11:165-71.
- [Google Scholar]
- Non-cirrhotic portal fibrosis among children admitted in a tertiary care hospital of Kolkata: A search for possible aetiologies. J Indian Med Assoc. 2011;109:889-91.
- [Google Scholar]
- Efficacy of endoscopic sclerotherapy on long-term management of oesophageal varices: A comparative study of results in patients with cirrhosis of the liver, non-cirrhotic portal fibrosis (NCPF) and extrahepatic portal venous obstruction (EHO) J Gastroenterol Hepatol. 1991;6:471-5.
- [Google Scholar]
- Etiological spectrum of esophageal varices due to portal hypertension in Indian children: Is it different from the west? J Gastroenterol Hepatol. 2008;23:1354-7.
- [Google Scholar]
- Aetiology of paediatric portal hypertension - experience of a tertiary care centre in South India. Trop Doct. 2009;39:42-4.
- [Google Scholar]
- Idiopathic non-cirrhotic intrahepatic portal hypertension: Common cause of cryptogenic intrahepatic portal hypertension in a Southern Indian tertiary hospital. Indian J Gastroenterol. 2009;28:83-7.
- [Google Scholar]
- Etiologic types of end-stage chronic liver disease in adults: Analysis of prevalence and their temporal changes from a study on native liver explants. Eur J Gastroenterol Hepatol. 2012;24:1199-208.
- [Google Scholar]
- Prognosticating after variceal bleed in cryptogenic cirrhosis: Non cirrhotic portal hypertension can be a confounder. J Hepatol. 2016;64:S251-2.
- [Google Scholar]
- Slow cirrhosis – Or no cirrhosis? A lesion causing benign intrahepatic portal hypertension. J Pathol. 1982;137:253-72.
- [Google Scholar]
- Non-cirrhotic portal fibrosis related end stage liver disease in adults: Evaluation from a study on living donor liver transplant recipients. Hepatol Int. 2011;5:882-9.
- [Google Scholar]
- Assessment of environmental enteropathy in the MAL-ED cohort study: Theoretical and analytic framework. Clin Infect Dis. 2014;59(Suppl 4):S239-47.
- [Google Scholar]
- A rabbit model of non-cirrhotic portal hypertension by repeated injections of E. coli through indwelling cannulation of the gastrosplenic vein. Hepatobiliary Pancreat Dis Int. 2004;3:417-22.
- [Google Scholar]
- Non-cirrhotic intrahepatic portal hypertension: Associated gut diseases and prognostic factors. Dig Dis Sci. 2011;56:227-35.
- [Google Scholar]
- Nodular regenerative hyperplasia of the liver and coeliac disease: Potential role of IgA anticardiolipin antibody. Gut. 2004;53:1032-4.
- [Google Scholar]
- Increased incidence of glomerulonephritis following spleno-renal shunt surgery in non-cirrhotic portal fibrosis. Kidney Int. 1997;52:482-5.
- [Google Scholar]
- Spectrum of malabsorption in India – Tropical sprue is still the leader. J Assoc Physicians India. 2011;59:420-2.
- [Google Scholar]
- Tropical sprue in 2014: The new face of an old disease. Curr Gastroenterol Rep. 2014;16:391.
- [Google Scholar]
- Spectrum of chronic small bowel diarrhea with malabsorption in Indian subcontinent: Is the trend really changing? Intest Res. 2016;14:75-82.
- [Google Scholar]
- Chronic enterocyte infection with coronavirus. One possible cause of the syndrome of tropical sprue? Dig Dis Sci. 1982;27:1039-43.
- [Google Scholar]
- Tropical enteropathy: An adaptation of the small intestine to accelerated cell loss in “contaminated” environments. In: Robinson JWL, Dowling RH, Riecken EO, eds. Mechanisms of intestinal adaptation. Lancaster: MTP Press; 1982. p. :609-10.
- [Google Scholar]
- Tropical sprue is associated with contamination of small bowel with aerobic bacteria and reversible prolongation of orocecal transit time. J Gastroenterol Hepatol. 2003;18:540-7.
- [Google Scholar]
- Low-grade small intestinal bacterial overgrowth is common in patients with non-alcoholic steatohepatitis on quantitative jejunal aspirate culture. Indian J Gastroenterol. 2017;36:390-9.
- [Google Scholar]
- Prevalence of adult celiac disease in India: Regional variations and associations. Am J Gastroenterol. 2016;111:115-23.
- [Google Scholar]
- Association of celiac disease with non-cirrhotic portal fibrosis. J Gastroenterol Hepatol. 2006;21:332-4.
- [Google Scholar]
- Investigation into celiac disease in Indian patients with portal hypertension. Indian J Gastroenterol. 2014;33:517-23.
- [Google Scholar]
- Household sanitation is associated with lower risk of bacterial and protozoal enteric infections, but not viral infections and diarrhoea, in a cohort study in a low-income urban neighbourhood in Vellore, India. Trop Med Int Health. 2017;22:1119-29.
- [Google Scholar]
- Hepatic manifestations in chronic arsenic toxicity. Indian J Gastroenterol. 1999;18:152-5.
- [Google Scholar]
- Chronic arsenic toxicity in West Bengal – The worst calamity in the world. J Indian Med Assoc. 1998;96:4-7, 18.
- [Google Scholar]
- Chronic arsenic toxicity: Studies in West Bengal, India. Kaohsiung J Med Sci. 2011;27:360-70.
- [Google Scholar]
- Chronic arsenic toxicity in Bangladesh and West Bengal, India – A review and commentary. J Toxicol Clin Toxicol. 2001;39:683-700.
- [Google Scholar]
- Effect of drinking arsenic contaminated water in children. Indian Pediatr. 2007;44:925-7.
- [Google Scholar]
- Groundwater arsenic contamination in the Ganga river basin: A future health danger. Int J Environ Res Public Health. 2018;15 pii: E180
- [Google Scholar]
- Arsenic groundwater contamination and its health effects in Patna district (capital of Bihar) in the Middle Ganga plain, India. Chemosphere. 2016;152:520-9.
- [Google Scholar]
- Arsenic groundwater contamination and its health effects in the state of Uttar Pradesh (UP) in upper and middle Ganga plain, India: A severe danger. Sci Total Environ. 2006;370:310-22.
- [Google Scholar]
- Arsenic in groundwater of the Kolkata municipal corporation (KMC), India: Critical review and modes of mitigation. Chemosphere. 2017;180:437-47.
- [Google Scholar]
- The Hindu.1.04 Cr hit by argenic contamination in Bengal. Available from: http://www.thehindu.com/news/cities/kolkata/104-cr-hit-by-arsenic-contamination-in-bengal/article17530242.ece
- Arsenicosis, possibly from contaminated groundwater, associated with noncirrhotic intrahepatic portal hypertension. Indian J Gastroenterol. 2016;35:207-15.
- [Google Scholar]
- Randomized placebo-controlled trial of 2,3-dimercapto-1-propanesulfonate (DMPS) in therapy of chronic arsenicosis due to drinking arsenic-contaminated water. J Toxicol Clin Toxicol. 2001;39:665-74.
- [Google Scholar]
- Study on arsenic level in public water supply of Delhi using hydride generator accessory coupled with atomic absorption spectrophotometer. Indian J Clin Biochem. 2006;21:70-6.
- [Google Scholar]
- Pattern and prevalence of substance use and dependence in the union territory of Chandigarh: Results of a rapid assessment survey. Indian J Psychiatry. 2017;59:284-92.
- [Google Scholar]
- Clinical outcomes, histopathological patterns, and chemical analysis of ayurveda and herbal medicine associated with severe liver injury-A single-center experience from Southern India. Indian J Gastroenterol. 2018;37:9-17.
- [Google Scholar]
- Hepatic damage caused by chronic arsenic toxicity in experimental animals. J Toxicol Clin Toxicol. 2000;38:395-405.
- [Google Scholar]
- Hepatic fibrogenesis using chronic arsenic ingestion: Studies in a murine model. Indian J Exp Biol. 1999;37:147-51.
- [Google Scholar]
- Deficiencies of serum ferritin and Vitamin B12, but not folate, are common in adolescent girls residing in a slum in Delhi. Int J Vitam Nutr Res. 2015;85:14-22.
- [Google Scholar]
- GWAS identifies population-specific new regulatory variants in FUT6 associated with plasma B12 concentrations in Indians. Hum Mol Genet. 2017;26:2551-64.
- [Google Scholar]
- Status of Vitamin B12 and folate among the urban adult population in South India. Ann Nutr Metab. 2016;68:94-102.
- [Google Scholar]
- Use of serum Vitamin B12 level as a marker to differentiate idiopathic noncirrhotic intrahepatic portal hypertension from cryptogenic cirrhosis. Dig Dis Sci. 2013;58:179-87.
- [Google Scholar]
- Vitamin B12 deficiency in patients with unexplained portal hypertension indicates absence of severe liver fibrosis. J Clin Gastroenterol. 2019;53:e126-7.
- [Google Scholar]
- Plasma-aminothiols status and inverse correlation of total homocysteine with B-vitamins in arsenic exposed population of West Bengal, India. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2016;51:962-73.
- [Google Scholar]
- Kinetics, distribution and sites of destruction of 111indium-labelled human platelets. Br J Haematol. 1980;44:269-80.
- [Google Scholar]
- Organ distribution and fate of human platelets: Studies of asplenic and splenomegalic patients. Am J Hematol. 1986;23:231-8.
- [Google Scholar]
- Serum cytokine elevations in celiac disease: Association with disease presentation. Hum Immunol. 2010;71:50-7.
- [Google Scholar]
- Effects of inflammatory cytokines on the release and cleavage of the endothelial cell-derived ultralarge von willebrand factor multimers under flow. Blood. 2004;104:100-6.
- [Google Scholar]
- Comprehensive analysis of ADAMTS13 in patients with liver cirrhosis. Thromb Haemost. 2008;99:1019-29.
- [Google Scholar]
- Orthotopic liver transplantation (OLTx) in non-cirrhotic portal hypertension secondary to ADAMTS13 deficiency. Prz Gastroenterol. 2016;11:56-8.
- [Google Scholar]
- Hepatoportal sclerosis in childhood: Some presenting with cholestatic features (a re-evaluation of 12 children) Pediatr Dev Pathol. 2012;15:107-13.
- [Google Scholar]
- Familial occurrence of nodular regenerative hyperplasia of the liver. Am J Gastroenterol. 2013;108:150-1.
- [Google Scholar]
- Familial aggregation in noncirrhotic portal fibrosis: A report of four families. Am J Gastroenterol. 1987;82:1130-3.
- [Google Scholar]
- Familial occurrence of nodular regenerative hyperplasia of the liver: A report on three families. Gut. 1999;45:289-94.
- [Google Scholar]
- An autosomal dominant form of non-cirrhotic portal hypertension. J Hepatol. 2015;63:525-7.
- [Google Scholar]
- Obliterative portal venopathy: A study of 48 children. J Pediatr. 2014;165:190-300.
- [Google Scholar]
- Idiopathic noncirrhotic portal hypertension is associated with poor survival: Results of a long-term cohort study. Aliment Pharmacol Ther. 2012;35:1424-33.
- [Google Scholar]
- Recurrent recessive mutation in deoxyguanosine kinase causes idiopathic noncirrhotic portal hypertension. Hepatology. 2016;63:1977-86.
- [Google Scholar]
- A de novo mutation in KCNN3 associated with autosomal dominant idiopathic non-cirrhotic portal hypertension. J Hepatol. 2016;64:974-7.
- [Google Scholar]
- Genetic determinants of idiopathic noncirrhotic portal hypertension in HIV-infected patients. Clin Infect Dis. 2013;56:1117-22.
- [Google Scholar]
- Nodular regenerative liver hyperplasia as a complication of azathioprine-containing immunosuppressive treatment for Crohn's disease. Immunopharmacol Immunotoxicol. 2011;33:398-402.
- [Google Scholar]
- Analysis of inherited thrombophilic mutations and natural anticoagulant deficiency in patients with idiopathic portal hypertension. J Thromb Thrombolysis. 2009;28:57-62.
- [Google Scholar]
- Nodular regenerative hyperplasia, portal vein thrombosis, and avascular hip necrosis due to hyperhomocysteinaemia. Gut. 2005;54:1021-3.
- [Google Scholar]
- Idiopathic portal hypertension in a systemic sclerosis patient heterozygous for factor V Leiden mutation. Rheumatol Int. 2003;23:44-6.
- [Google Scholar]
- Possible HLA influence in governing susceptibility to non-cirrhotic portal fibrosis. Tissue Antigens. 1987;30:184-7.
- [Google Scholar]
- Profiles of serum complement in patients with hepatobiliary diseases. Digestion. 1978;18:371-83.
- [Google Scholar]
- Immunological profile of patients with non-cirrhotic portal fibrosis. J Gastroenterol Hepatol. 1990;5:425-31.
- [Google Scholar]
- Interaction between multimeric von Willebrand factor and complement: A fresh look to the pathophysiology of microvascular thrombosis. J Immunol. 2017;199:1021-40.
- [Google Scholar]
- Mutations in a member of the ADAMTS gene family cause thrombotic thrombocytopenic purpura. Nature. 2001;413:488-94.
- [Google Scholar]
- Defining the genetics of thrombotic microangiopathies. Transfus Apher Sci. 2016;54:212-9.
- [Google Scholar]
- The role of ADAMTS-13 activity and complement mutational analysis in differentiating acute thrombotic microangiopathies. J Thromb Haemost. 2016;14:175-85.
- [Google Scholar]
- ADAMTS13 missense variants associated with defective activity and secretion of ADAMTS13 in a patient with non-cirrhotic portal hypertension. Indian J Gastroenterol. 2017;36:380-9.
- [Google Scholar]
- Crystal structure and enzymatic activity of an ADAMTS-13 mutant with the East Asian-specific P475S polymorphism. J Thromb Haemost. 2013;11:1399-406.
- [Google Scholar]
- Complement factor H mutation in familial thrombotic thrombocytopenic purpura with ADAMTS13 deficiency and renal involvement. J Am Soc Nephrol. 2005;16:1177-83.
- [Google Scholar]
- Analysis of single nucleotide polymorphism at rs6677604 in patients with non-cirrhotic intrahepatic portal hypertension. J Clin Exp Hepatol. 2015;5:S54.
- [Google Scholar]
- Noncirrhotic portal fibrosis/idiopathic portal hypertension: APASL recommendations for diagnosis and treatment. Hepatol Int. 2007;1:398-413.
- [Google Scholar]
- Non-cirrhotic portal fibrosis (NCPF) is a vanishing disease in India. Trop Gastroenterol. 2003;24:45-6.
- [Google Scholar]
- Idiopathic noncirrhotic intrahepatic portal hypertension is an ongoing problem in India. Hepatology. 2011;54:2274.
- [Google Scholar]
- Non-cirrhotic portal hypertension - diagnosis and management. J Hepatol. 2014;60:421-41.
- [Google Scholar]
- Idiopathic non-cirrhotic intrahepatic portal hypertension in the west: A re-evaluation in 28 patients. Gut. 2002;51:275-80.
- [Google Scholar]
- Prevalence of significant liver disease in human immunodeficiency virus-infected patients exposed to didanosine: A cross sectional study. World J Hepatol. 2016;8:1623-8.
- [Google Scholar]
- Hepatoportal sclerosis related to the use of herbals and nutritional supplements. Causality or coincidence? Ann Hepatol. 2016;15:932-8.
- [Google Scholar]
- Swatch Bharat Mission or Clean India Mission, Ministry of Drinking water and sanitation, Government of India. Available from: http://www.sbm.gov.in/sbm/
- Available from: http://www.nmcg.nic.in/
- Report of the task force on formulating action plan for removal of arsenic contamination in West Bengal. Available from: http://www.planningcommission.nic.in/aboutus/committee/wrkgrp11/tf11_arsenics.pdf
- How the public is getting India's Adyar river clean. Available from: http://www.worldrowing.com/news/how-the-publicgetting-india-adyar-river-clean






