Translate this page into:
Epidemiological & clinical profile of influenza A (H1N1) 2009 virus infections during 2015 epidemic in Rajasthan
Reprint requests: Dr Bharti Malhotra, Department of Microbiology, SMS Medical College & Hospital, Jawahar Lal Nehru Marg, Jaipur 302 004, Rajasthan, India e-mail: drbhartimalhotra@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Pandemic influenza A (H1N1) 2009 virus emerged in 2009 and caused pandemic with high morbidity and mortality in India and worldwide. The number of H1N1-positive cases varied in different years in Rajasthan. The objective of the study was to present the epidemiological profile of pandemic influenza A (H1N1) 2009 virus cases in Rajasthan from January to March 2015.
Methods:
A retrospective descriptive, record-based analysis of suspected and confirmed cases of pandemic influenza A (H1N1) 2009 virus infection in Rajasthan, India, from January to March 2015 was performed. Testing was done as per the Centers for Disease Control guidelines at nine laboratories approved by the Government of Rajasthan. Data were analyzed in terms of demographic characteristics, clinical presentation and outcome.
Results:
Among 18,187 tested cases, 6203 (34.10%) were positive. Death occurred in 378 cases, with six per cent case fatality rate. Maximum number of cases (n=2801) and deaths (n=101) were from Jaipur zone. The highest number of cases, 47.60 per cent (2953/6203) and deaths, 52.11 per cent (197/378) were in the age group of 26-50 yr; 52.64 per cent (199/378) of deaths occurred in females. The highest number (63.5%) of deaths was from urban areas. Associated risk factors were observed in 59.44 per cent of the death cases, pregnancy being the predominant predisposing factor. In 61.92 per cent of patients, death occurred within three days of hospitalization.
Interpretation & conclusions:
H1N1 epidemic caused high morbidity and mortality in early 2015, particularly in the younger and middle-aged population and pregnant women in Rajasthan State of India. The study highlights the regular surveillance of influenza like illness, early diagnosis and timely initiation of therapy in suspected cases.
Keywords
Epidemiology
H1N1
influenza
Oseltamivir
pandemic
real-time polymerase chain reaction
Pandemic influenza A (H1N1) 2009 is a novel strain of influenza A virus evolved by genetic reassortment. This virus was first reported in Mexico in April 20091 and rapidly spread to various countries worldwide12. High morbidity (27236 cases) and mortality (981 deaths) have been reported from India3. The World Health Organization (WHO) announced the global pandemic in June 2009 which was declared post-pandemic phase in August 2010. As per the WHO, the pandemic influenza A (H1N1) virus is now considered as seasonal influenza virus4. The mortality and morbidity due to pandemic influenza A (H1N1) 2009 virus continues to remain high in India. A large number of pandemic influenza A (H1N1) 2009 virus cases and deaths have been reported from Rajasthan during H1N1 pandemic in 2009-20105. In 2015, pandemic influenza A (H1N1) 2009 virus epidemic became widespread throughout Rajasthan. In mid-March 2015, the total number of laboratory confirmed cases of pandemic influenza A (H1N1) 2009 virus in India was 29,978, with death of 1793 people6. Rajasthan (6203 cases, 378 deaths) and Gujarat (6150 cases and 387 deaths) were the worst affected States as per the data communicated (personal communication) by the Emergency Medical Relief (EMR), Ministry of Health and Family Welfare, Government of India (MOHFW-GOI). As there are limited data on profile of pandemic influenza A virus infections in Rajasthan, this study was planned to analyse the epidemiology and clinical profile of pandemic influenza A (H1N1) 2009 cases during an epidemic in Rajasthan from January to March 2015.
Material & Methods
This study was a retrospective descriptive, record-based analysis of suspected and confirmed cases of pandemic influenza A (H1N1) 2009 infection which occurred in Rajasthan during January to March 2015. The study was carried out at the Advanced Research Laboratory, SMS Medical College, Jaipur, Rajasthan, India. The study was approved by the Institutional ethics committee.
Epidemiological data: The case definitions followed were as follows: (i) Suspected case defined as a case with signs and symptoms as per category B and C7; and (ii) Confirmed case defined as a probable case that was tested positive for pandemic influenza A (H1N1) 2009 by real-time reverse transcription polymerase chain reaction (RT-PCR).
All patients with categories B and C were given treatment and samples were sent for testing, and treatment was discontinued if found negative. The complete information about all suspected and confirmed cases and deaths at the H1N1 visiting screening centres, swine flu outpatient departments and swine flu isolation wards and hospitals from Rajasthan was collected. The data were compiled at the State Surveillance Unit using proforma prepared by the State government.
Rajasthan is divided into seven zones, among which six zones have one government medical college each and these medical colleges get samples from their respective zones. Testing of pandemic influenza A (H1N1) 2009 virus was carried out at the Microbiology laboratory of six government medical colleges, namely, SMS Medical College (Jaipur), RNT Medical College (Udaipur), SP Medical College (Bikaner), Dr. S.N. Medical College (Jodhpur), JLN Medical College (Ajmer), Government Medical College (Kota) and three private laboratories (A-Lal lab, Delhi; B-Lal lab, Jaipur; SRL, Gurgaon) approved by the Government of Rajasthan. The quality control (QC) measures of the laboratories were monitored by the National Centre for Disease Control (NCDC), New Delhi, for all laboratories. The QC measures by the NCDC included training of the laboratory staff, checking the design of the laboratory in terms of biosafety and for molecular diagnosis, sending samples for proficiency testing and after clearing proficiency, certifying the laboratories for pandemic influenza A (H1N1) 2009 testing.
Sample collection and RT-PCR: Throat or nasal swab samples of suspected cases with influenza-like illness (ILI) were collected in Viral Transport Medium and sent to laboratories maintaining cold-chain. RNA was extracted by QIAamp Viral RNA Mini Kit (Qiagen, Germany). RNA of each isolate was tested by separate primer/probe sets for InfA, Universal Swine (swFluA), Swine H1 (swH1) and RNaseP (Applied Biosystems, USA) as per the CDC real-time RT-PCR protocol (ABI Step One Plus RT-PCR instrument - Applied Biosystems, USA)8.
The epidemiological profiles of all pandemic influenza A (H1N1) 2009 virus cases were analyzed in terms of demographic characteristics, clinical presentation and outcome. Statistical analysis on stratified data was performed using Chi-square test. Case fatality rate (CFR) was calculated for pandemic influenza A (H1N1) 2009 positive cases leading to death.
Results
A total of 18,187 patients suspected to have pandemic influenza A (H1N1) 2009 virus infection were tested in this period of whom 34.10 per cent (6203) were found positive. Death occurred in 378 cases with CFR of six per cent in positive cases. The zone-wise distribution of H1N1 cases is shown in Table I. The highest, 45.16 per cent of positive cases and 26.72 per cent of deaths were from Jaipur region, followed by Kota region for positive cases (861, 13.88%) and Ajmer for deaths (92, 24.33%). Highest CFR was observed in Ajmer (15.28%), followed by Udaipur (8.58%) and Bikaner (7.73%). CFR in Jaipur (3.61%) and Kota was lower (2.79%) (Table I).
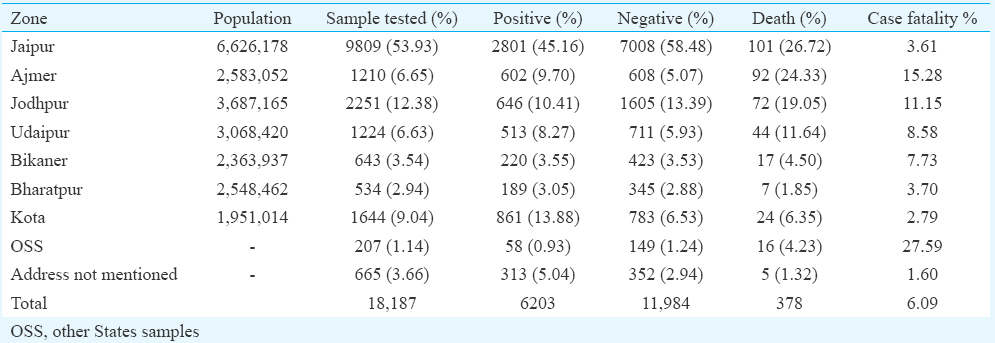
Weekly distribution of pandemic influenza A (H1N1) 2009 positive cases and deaths in Rajasthan from week 1 to 11 (December 29, 2014 to March 15, 2015) is shown in Fig. 1. As per weekly trends in positivity, only six cases were observed in the first week, but there was a sudden increase in the sixth week and cases peaked in eighth week while deaths peaked in the seventh week after which decline in number of cases and deaths was seen.
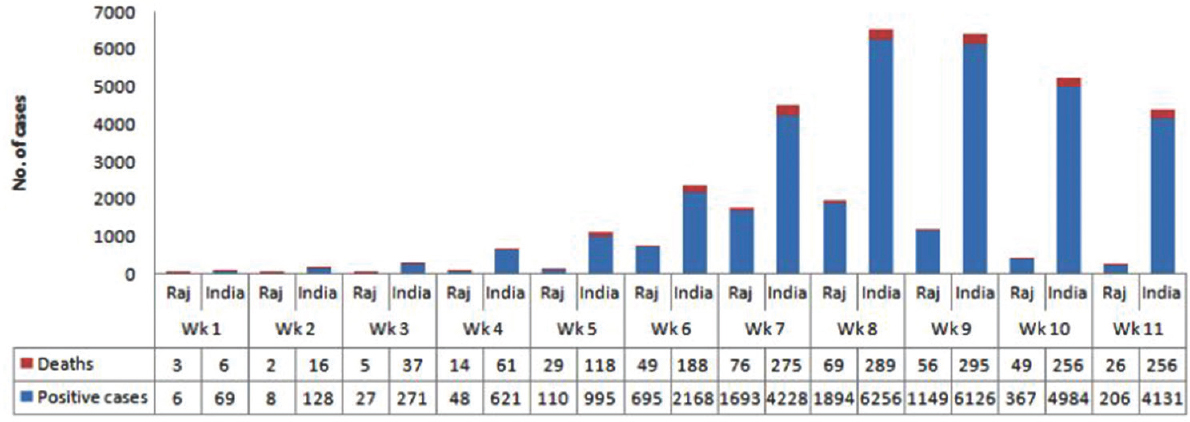
- Weekly trends of pandemic influenza A (H1N1) 2009 cases and deaths from January to March 2015 in Rajasthan State and India6.
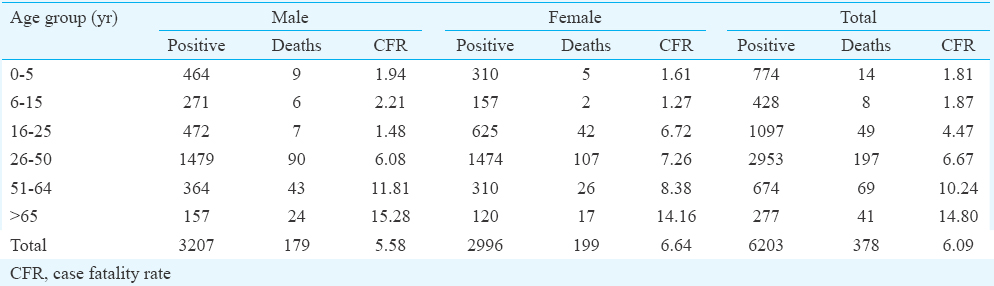
The age and sex distribution of pandemic influenza A (H1N1) 2009 virus positive and death cases are shown in Table II. A total of 6203 cases were positive; of these, 3207 (51.70%) were males; and 2953 (47.60%) cases were in 26-50 yr age group. Pandemic influenza A (H1N1) 2009 virus infection rate was higher in people from urban areas (5659, 91.23%) than from rural areas (544, 8.77%). Stratified analysis revealed that deaths were more in urban areas among females (35.98%) and in 16-65 yr age group (Table III).
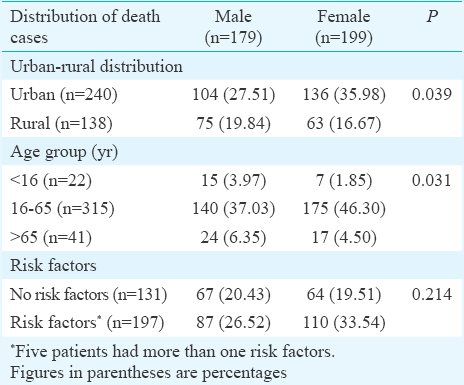
Fever, sore throat, running nose, cough, shortness of breath, diarrhoea, vomiting, headache and body ache were the common clinical symptoms. On carrying out death audit of 323 death cases, 131 (40.56%) had no risk factors and 192 (59.44%) had associated risk factors. Pregnancy was the most common associated risk factor (49, 15.17%), followed by heart disease (36, 11.15%), diabetes mellitus type 2 (34, 10.53%), respiratory diseases (27, 8.36%), cancer (16, 4.95%), obesity (7, 2.17%), thyroid diseases (7, 2.17%), kidney diseases (5, 1.55%), liver diseases (4, 1.24%) and other diseases (12, 3.72%). Of the 49 pregnant women, 47 (95.91%) were admitted to the Intensive Care Unit (ICU) and all were on ventilator. Pregnancy was the most predominant risk factor associated with pandemic influenza A (H1N1) 2009 virus-associated mortality. One hundred and six death cases (33%) were admitted after 4-5 days of onset of symptoms, 200 (62%) expired within three days of hospitalization (Fig. 2). Two hundred ninety of 323 death cases (89.78%) were admitted to the ICUs, of whom 275 (94.83%) were on ventilator.
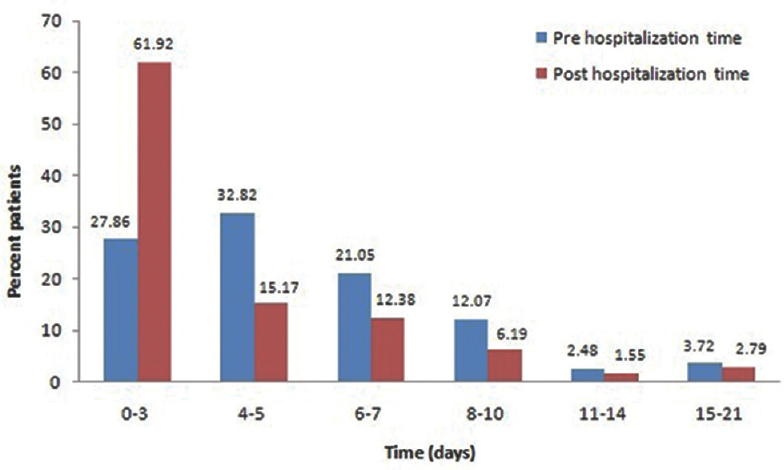
- Details of pre- and post-hospitalization time in pandemic influenza A (H1N1) 2009 death cases (n=323).
Discussion
There was sudden increase in number of pandemic influenza A (H1N1) 2009 virus-positive cases in India in January 2015 and the infection became widespread. Fever and cough were the most common clinical symptoms seen in our study as has been reported earlier also910, followed by sore throat, running nose, headache, body ache, vomiting, breathlessness, weakness, diarrhoea, etc. In children, commonly reported symptoms were fever, cough and running nose as reported previously111213.
The percentage of positive cases (34.11%) in the present study was higher than that reported in earlier studies, 22 per cent in India14, 23.3 per cent in Mexico15, 21.8 and 24.6 per cent in Rajasthan during 2012-20131617 and 32.93 per cent in Gujarat18. Death occurred in 378 cases and the CFR was six per cent in our study. No particular clinical or biochemical predictor was observed for mortality. Patients not responding on oxygen mask and non-invasive ventilation, having arterial PO2 less than 90 were put on invasive ventilator, and mortality was high in such patients19.
The CFR was found to be 12.6 and 21 per cent in 2012 and 2013 in Western Rajasthan1617, 1.8 per cent from south India20 and 17.9 per cent in hospitalized patients at Jaipur19. In the present study, positivity was higher in urban population (91.23%) than rural population (8.77%) as reported earlier21. Mortality was also higher (63.5%) in urban areas, particularly in women in our study as reported earlier from Gujarat (64.2%)18 and Rajasthan (64.22%)22.
Positivity and mortality were predominantly seen in 16-65 yr age group in the present study as has been earlier reported from India and other countries1617232425. People in this age group are mostly working and thus liable to get exposed to pandemic influenza A (H1N1) 2009 infection while those above 65 yr may have had greater immunity due to previous exposure to similar viruses2627.
In the present study, positivity started increasing from the first week of January, reached at the highest in the eighth week of 2015, with a decline subsequently. The relationship of influenza virus with low temperature has been reported from other States of India16282930.
Of the 323 deaths in the present study, 59.44 per cent had associated risk factors. A study from the USA reported co-morbidities in 73 per cent of fatal cases; asthma, diabetes, heart, lung, neurologic diseases and pregnancy28; in addition, metabolic diseases, immunosuppressive conditions and neuromuscular disorders were reported from California25. Heart and respiratory diseases along with anaemia, obesity and cancer were the common co-morbidities reported in Indian studies2023. High mortality was found in pregnant women in our study as reported earlier322.
There were some limitations in the present study. Detailed death audit was not done to find the causes of death; only data obtained in proforma were analyzed. Analysis was not done for respiratory parameters of responders and non-responders. The reason as to why some districts in Rajasthan had lower positivity and low CFR, besides regional geographical conditions was not taken into account, which might have a significant impact on prevalence and morbidity. As per the guidelines, category B should not be tested, but the same was not followed in this study due to the emergency situation; hence, there was limitation in comparison of CFR data over the period. There is also a need to carry out subtyping of influenza A and correlate clinical and epidemiological profile of circulating subtypes of non-pandemic influenza A.
In conclusion, our study showed high mortality and morbidity due to pandemic influenza A (H1N1) 2009 virus infections in Rajasthan, particularly in the younger and middle-aged population. Pregnancy, anaemia, heart and lung diseases were the common predisposing factors. Regular surveillance, early diagnosis and timely initiation of oseltamivir therapy in suspected cases would be helpful to reduce mortality and morbidity under such emergency situation.
Acknowledgment
Authors acknowledge the support of members of the Swine flu task force formed by the State Government of Rajasthan in 2015, the chairman of the task force, Dr Ashok Panagariya (Emeritus Professor), along with Shri J.C. Mohanty, Principal Secretary, Department of Medical Education, Shri Mukesh Sharma, Principal Secretary, Department of Health, Dr S.P. Singh, Joint Secretary, Department of Medical Education, Government of Rajasthan, Dr U.S. Agarwal, Principal and Controller, SMS Medical College, Jaipur, and various experts. Authors thank the National Centre for Disease Control (NCDC) for QC testing of the laboratory and for providing training to the laboratory staff for H1N1 testing, and acknowledge all the nine research laboratories for testing of samples and providing data for this manuscript.
Conflicts of Interest: None.
References
- Centers for Disease Control and Prevention (CDC). Update: Novel Influenza A (H1N1) Virus Infection: Mexico, March-May, 2009. MMWR Morb Mortal Wkly Rep. 2009;58:585-9.
- [Google Scholar]
- Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;360:2605-15.
- [Google Scholar]
- Clinical profile & outcome of H1N1 infected pregnant women in a tertiary care teaching hospital of Northern India. Indian J Med Res. 2014;139:454-8.
- [Google Scholar]
- Pandemic (H1N1) 2009 Briefing Note 23. WHO Recommendations for the Post-Pandemic Period. Available from: http://www.who.int/csr/disease/swineflu/notes/briefing_20100810/en/
- Modeling of H1N1 outbreak in Rajasthan: methods and approaches. Indian J Community Med. 2011;36:36-8.
- [Google Scholar]
- Emergency Medical Relief (EMR), Ministry of Health and Family Welfare, Government of India. Available from: http://mohfw.nic.in/index3.php?lang=1&level=0&deptid=115
- Guidelines on Categorization of Influenza A H1N1 Cases during Screening for Home Isolation, Testing Treatment, and Hospitalization. Available from: http://www.mohfw.nic.in/WriteReadData/l892s/804456402Categorisation.pdf
- CDC Protocol of Real Time RTPCR for Influenza A (H1N1). Available from: http://www.who.int/csr/resources/publications/swineflu/CDCRealtimeRTPCR_SwineH1Assay-2009_20090430.pdf
- Clinico-epidemiological profile of influenza A H1N1 cases admitted at a tertiary care institute of Western India. Int J Med Sci Public Health. 2014;3:1258-61.
- [Google Scholar]
- An epidemiological study of confirmed H1N1 admitted cases in an infectious disease hospital, Pune. J Krishna Inst Med Sci Univ. 2012;1:81-90.
- [Google Scholar]
- Clinical presentations of pandemic 2009 influenza A (H1N1) virus infection in hospitalized Thai children. J Med Assoc Thai. 2011;94:S107-12.
- [Google Scholar]
- Pandemic influenza A(H1N1) 2009 outbreak in a residential school at Panchgani, Maharashtra, India. Indian J Med Res. 2010;132:67-71.
- [Google Scholar]
- Emergence of pandemic 2009 influenza A H1N1, India. Indian J Med Res. 2012;135:534-7.
- [Google Scholar]
- Characterizing the epidemiology of the 2009 influenza A/H1N1 pandemic in Mexico. PLoS Med. 2011;8:e1000436.
- [Google Scholar]
- Epidemiological profile of H1N1 cases in Western Rajasthan from January 2012 to December 2012. Indian J Public Health Res Dev. 2015;6:118-22.
- [Google Scholar]
- Epidemiological profile of influenza A H1N1 cases in Western Rajasthan in year 2013. Paripex Indian J Res. 2013;2:264-6.
- [Google Scholar]
- Epidemiological characteristics including seasonal trend of hospital based swine flu cases in Jamnagar region, Gujarat, India. J Res Med Dent Sci. 2015;3:39-42.
- [Google Scholar]
- Profiling the mortality due to influenza A (H1N1) pdm09 at a tertiary care hospital in Jaipur during the current season - January & February 2015. J Assoc Physicians India. 2015;63:36-9.
- [Google Scholar]
- Case series study of the clinical profile of H1N1 swine flu influenza. J Assoc Physicians India. 2011;59:14-6. 18
- [Google Scholar]
- An outbreak of pandemic influenza A (H1N1) in Kolkata, West Bengal, India, 2010. Indian J Med Res. 2012;135:529-33.
- [Google Scholar]
- Demographic correlates of swine flu cases attending a tertiary care hospital in Rajasthan. Indian J Prev Soc Med. 2012;43:224-8.
- [Google Scholar]
- Epidemiological characteristics of H1N1 positive deaths: a study from tertiary care hospital in Western India. Int J Med Sci Public Health. 2013;2:305-8.
- [Google Scholar]
- Pandemic influenza A (H1N1) 2009 and mortality in the United Kingdom: Risk factors for death, April 2009 to March 2010. Euro Surveill. 2010;15 pii: 19571
- [Google Scholar]
- Factors associated with death or hospitalization due to pandemic 2009 influenza A(H1N1) infection in California. JAMA. 2009;302:1896-902.
- [Google Scholar]
- H1N1 revisited after six years: then and now. J Assoc Physicians India. 2015;63:41-3.
- [Google Scholar]
- Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: a modelling study. Lancet Infect Dis. 2012;12:687-95.
- [Google Scholar]
- Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N Engl J Med. 2009;361:1935-44.
- [Google Scholar]
- Differences in influenza seasonality by latitude, Northern India. Emerg Infect Dis. 2014;20:1723-6.
- [Google Scholar]
- Dynamics of influenza seasonality at sub-regional levels in India and implications for vaccination timing. PLoS One. 2015;10:e0124122.
- [Google Scholar]






