Translate this page into:
High frequency of HPV16 European variant E350G among Mexican women from Sinaloa
For correspondence: Dr Jose Guadalupe Rendon Maldonado, Faculty of Chemical and Biological Sciences, Autonomous University of Sinaloa, Av. de las Americas y Blvd. Universitarios S/N, Ciudad Universitaria, Culiacan, Sinaloa, 80010 Mexico e-mail: jgrendonm@uas.edu.mx
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Human papillomavirus (HPV) infections play a crucial role in the aetiology of cervical cancer (CC), and HPV16 is the primary viral genotype associated with CC. A number of variants of the HPV16 E6 gene are involved in the progression of CC, differing in their prevalence and biological and biochemical properties. This study was designed to determine the frequency of HPV types 16/18 and to identify the presence of HPV16 E6-variants in asymptomatic Mexican women.
Methods:
A total of 189 cervical Pap smears were collected from women attending public health services in three different cities in Sinaloa, Mexico. Viral DNA was identified by amplification of E6 viral gene fragments using polymerase chain reaction (PCR). Identification of variants was done by sequencing a DNA fragment (321bp) of the HPV16 E6 gene.
Results:
More than half of the women tested were HPV-positive (52.38%), with HPV16 being the most frequent genotype (21.16%), followed by HPV18 (8.99%). Sequence analysis of the E6-HPV16 PCR products showed that in all cases, the viruses corresponded to European variants. It was further observed that the E350G intra-variant was the most common (>76%).
Interpretation & conclusions:
This study showed a predominance of European lineage variants of HPV16 among asymptomatic women from Sinaloa, Mexico, predominantly with of the E350G variant. This variant has been shown to be associated with an increased risk of early development of CC. The use of molecular identification of carcinogenic HPV and Pap test screening may be a good strategy for monitoring women to prevent CC.
Keywords
Cervical cancer
European variant
human papillomavirus
molecular diagnostics
Cervical cancer (CC) is the fourth-most common cancer in women worldwide, affecting 500,000 individuals each year, primarily in the developing countries1. Among Mexican women, CC is the leading cause of death from cancer with a mortality rate of 6.09 deaths per 100,000 women, as reported by the Health Ministry of Mexico2. High mortality rates due to CC have been reported in Sinaloa, Mexico, where the mortality rate was 9.50 deaths per 100,000 >25 yr old women3. The major cause of high-grade cervical squamous intraepithelial lesions (HG-SIL) is a persistent infection of the cervix with a high-risk human papillomavirus (HR-HPV) types, predominantly the HPV16 and/or HPV18 genotypes. The presence of HPV16 DNA has been reported in approximately 63-90 per cent of CC cases45, being the most common worldwide. The HPV16 genotype is detected in almost 50 per cent of CC cases, followed by HPV18, HPV45 and HPV3156. It has been reported that the prevalence of HPV infections in healthy women varies with age in different regions of the world6. Most instances of CC occur 15-20 yr after the initial HPV infection78. This period of latency could explain why CC is the most common in young and middle-aged women67910. The sequence variations in the HPV16 E6 gene have been observed to correctly classify HPV16 variants isolated from different continents11. Therefore, most studies of HPV16 variants have focused on the E6 gene, which encodes the major transforming protein that inhibits apoptosis, promotes cellular proliferation and is associated with cancer aggressiveness121314. Worldwide, variants of the HPV16 genome in CC from different geographical areas have been classified into phylogenetic lineages, such as European (E) (A1-A4), Asian (As), Asian-America (AA) (D2 and D3), African-1 and -2 (Af1 and Af2) (B1, B2 and C) and North American (NA1) (D1)14. Some studies have shown that HPV16 variants promote disease progression, ranging from HG-SIL to the development of CC1415. In a previous study based on all 47 sequenced HPV16 genomes, the European variant nt350G was observed to occur frequently in HG-SIL [odds ratio (OR)=3.8, P=0.03], and was present in 36 HPV16 isolates from women with minor cervical abnormalities (OR=4.8, P=0.07)16. However, most strikingly, there was a clear association between the nt350G variant and HPV16 persistence over a period of two years15. However, the distribution and genotyping of HPV16 among asymptomatic healthy women have been poorly studied in Mexico. The objective of this study was therefore, to identify the HPV16 variants present among healthy asymptomatic women with normal cervical cytology in the State of Sinaloa, Mexico.
Material & Methods
In this cross-sectional study, 189 cervical Pap smears were collected from equal number of women who attended the integral diagnostic service for early detection of CC from September 2013 to March 2014 in hospitals from the three primary cities of Sinaloa, Mexico (IMSS 032 Hospital from Guasave, IMSS 046 Hospital from Culiacan and a Public Hospital from Mazatlan). The study protocol was approved by the institutional Bioethics Committees for Clinical Research, Faculty of Chemical and Biological Sciences, Autonomous University of Sinaloa, Culiacan, Sinaloa, and National Institute of Cancer (INCan), Mexico City, and written informed consent was obtained from all participants.
A probabilistic sample size was obtained consecutively from a population of 2040 women with normal cytology, using a 90 per cent confidence level and 80 per cent of power with an accuracy of five per cent bilaterally, with an expected proportion of 16 per cent testing HPV16 positive8, resulting in a sample size of 138. This study included women aged 16-69 yr who had attended a CC screening clinic, had normal cervical cytology, were not in their menstrual period and had not had intercourse 48 h before sampling. All consecutive women who fulfilled the inclusion criteria and consented to participate in the study were included.
All women with cervical neoplasia, dysplasia or who had a hysterectomy were excluded. Each woman was subjected to a cervical Pap smear, and an aliquot was stored at 4°C for analysis. Molecular HPV identification was performed using the consensus primers GP5+/GP6+ and HPV genotyping using HPV16 and HPV18 specific primers.
Viral genotyping: Cytological specimens were used for the detection of viral DNA by polymerase chain reaction (PCR) and for PCR-sequencing to identify HPV16 E6 variants. DNA extraction was performed using the salting out standard method17. PCR was carried out with 150 ng of total DNA with the previously reported primers GP5+/GP6+11. PCR products were analyzed by agarose gel electrophoresis and visualized with GelRed (Biotium, USA). As positive controls, 100 ng of Caski cell DNA (ATCC CRL-1550), and 100 ng of HeLa cell DNA were used. A reaction using sterile water instead of DNA was used as a negative control. For HPV-genotyping, PCR18 was carried out with 150 ng of total DNA with the specific primers HPV16 F (5´-CAA GCA ACA GTT ACT GCG A-3´) and HPV16 R (5´-CAA CAA GAC ATA CAT CGA CC-3´), and HPV18 F (5´-AAG GAT GCT GCA CCG GCT GA-3´), and HPV-18 R (5´-CAC GCA CAC GCT TGG CAG GT-3´) (Figure). When samples tested negative or the HPV type could not be identified, the primer pair GP5+/GP6+ was used, and the PCR products were sequenced.
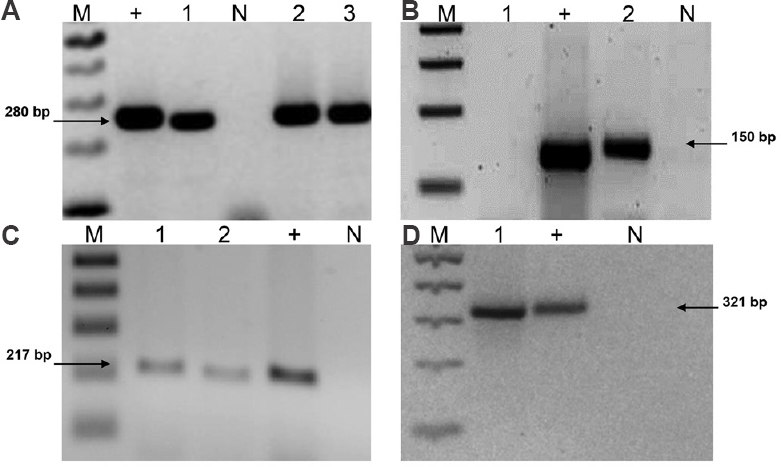
- Agarose gel electrophoresis of PCR reaction products. (A) Representative agarose gel with PCR products of human beta-globin (280bp). (B) 150 bp PCR product using GP5+/GP6+ common primer for HPV. (C) PCR products of HPV-18 using specific primers FHPV-18/RHPV18 (217bp). (D) PCR products of HPV-16 using specific primer FHPV-16/RHPV16 (321bp). M, 100 bp molecular weight marker, (+) positive control: in (A) human DNA, in (B and C) Ca Ski cells DNA, in (D) HeLa cells DNA. N, negative control without DNA. Numbers 1 to 3 correspond to PCR products using DNA from human cervical samples.
Sequence analysis: HPV16 variants were characterized by full-length sequence analysis11 of a 321 bp fragment of the E6 gene in only 31 samples (Figure D). PCR products were purified using 75 per cent isopropanol Centri-Sep Spin Columns (Applied Biosystems, USA) and sequenced using a 310 ABI PRISM Genetic Analyser (Applied Biosystems, USA). All sequences were compared to known sequences for HPV types, available at the NCBI site (http://www.ncbi.nlm.nih.gov).
Statistical analysis: Nominal variables were reported as the number and percentages of cases. OR with 95 per cent confidence intervals (CIs) were used to estimate significance (χ 2 Mantel-Haenszel with P<0.05).
Results
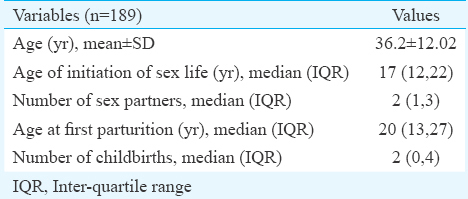
Characteristics of 189 women included in this study are shown in Table I. Most women were young, had started being sexually active at approximately 17 yr of age, and had an average of two childbirths. Their average number of sex partners was two, ranged between 1 and 3. The results from cervical Pap smears showed that all women had normal cytology, but 102 (53.97%) exhibited low-to-moderate inflammation with hyperaemia of stromal tissue, hyperplasia of basal cells, or leucocyte infiltration, despite all samples testing negative for cervical dysplasia. The PCR results showed that 99 of 189 samples (52.38%) were HPV positive, of these 40 (21.16%) were HPV16 positive and 17/189 (8.99%) tested positive for genotype 18; 10 (5.29%) were co-infected with both genotypes. Thirty one of 189 (16.40%) samples tested positive for other viral genotypes. Table II shows the association among risk factors, such as chronological age, age of the initiation of sexual activity, age at first childbirth, number of childbirths and number of sexual partners with HPV-infections and the presence of HPV16. With respect to HPV infection, only two factors showed a significant relationship. The age of women at their first childbirth being between the ages of 15 and 17 yr old (OR=3.1, CI 95%=1.19-8.24, P=0.03) and having three or more sex partners (OR=3.4, CI 95%=1.40-7.87, P=0.01) were associated with the high risk for testing HPV positive.
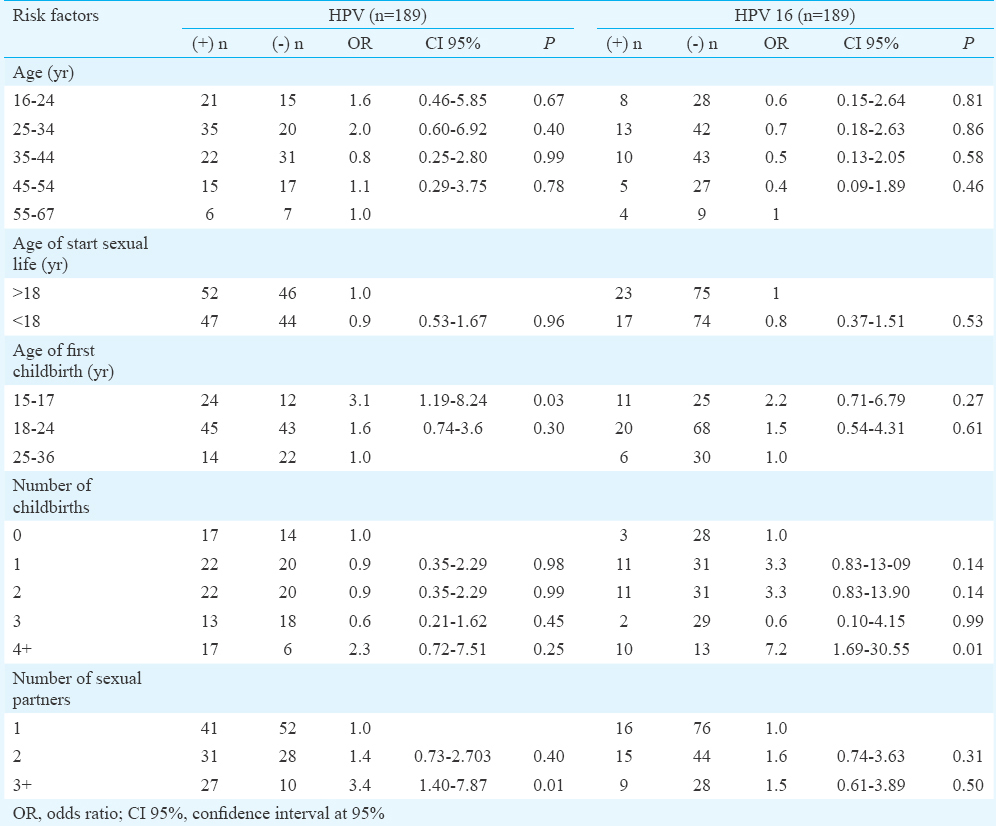
Concerning HPV16 infection, only one factor, the number of childbirths, was associated with a significantly increased risk of testing HPV16 positive (OR=7.2, CI 95%=1.69-30.55, P=0.01). There were limited results with respect to observations of HPV18 infections and HPV16/18 co-infections, precluded statistical analyses. Seventeen women were HPV18 positive, with two peaks observed in the number of positive cases, in 16-34 and 45-54 yr old women. There were 10 women with HPV16/18 co-infections, following a similar trend to that of HPV18 infections, albeit with a much lower number of cases. When age of the initiation of sexual activity was considered, there was a greater number of HPV18 infections and HPV16/18 co-infections in women older than 18 yr old. When reviewing the age at first childbirth, the highest incidence of HPV18 infections and HPV16/18 co-infections were observed in individuals between 18 and 24 yr old. In addition, women with <3 childbirths showed the highest occurrence of HPV18 infections and HPV16/18 co-infections.
Sequencing the E6 gene to identify HPV16 variants in 31 samples demonstrated that 100 per cent were of the European variant. Of these, 23 (74.2%) had a base pair substitution at the E350G position, with this change being the most prevalent. In total, 12 variations were observed in a 321 bp fragment of the E6 region. A similar distribution of the viral variants was observed in all samples.
Discussion
In this study, 52.4 per cent women with normal cytology were tested HPV positive. This differed from a previous study performed in two towns in southern Mexico that reported an HPV prevalence of 43.6 per cent18. However, studies in India showed HPV prevalence rates over 60 per cent in asymptomatic populations, with a more commonly reported prevalence of HPV infection between 10 and 12 per cent1920. In our study, HPV16 genotype was present in 21.16 per cent of the women. This result was similar to previous reports of this genotype in asymptomatic populations elsewhere in the world and consistent with other studies conducted in Mexico1321. The frequency was lower than that reported in Mexican patients with CC in whom the frequency of HPV16 was 50.9 per cent14.
In this study, 8.99 per cent women were tested positive for HPV18, and 5.29 per cent were co-infected with both the HPV16 and HPV18 genotypes. These data were in contrast with that reported in Puebla, Mexico, where 40 per cent of patients with a normal Pap smear had more than one viral genotype21. In other countries, the reported rates of co-infection with HPV16 and HPV18 were 15.3 per cent in Spain10, 17.9 per cent in Denmark9 and 18.2 per cent in the Netherlands8. It has been reported that there is a significant relationship between the presence of HPV16 and the development of HG-SIL. In addition, HPV18 is associated with low-grade lesions (LG-SIL)22. It is now believed that infection with HPV is necessary to cause, but is not sufficient for, the development of CC1213. Therefore, co-infection with other genotypes may pose a greater risk for the development of CC. Considering that we failed to determine the HPV genotypes in 16.40 per cent of HPV-positive women, further studies focused on identifying more HPV genotypes, and co-infections are necessary.
Although the identification of HPV16 variants in our study was done by assaying the E6 gene sequence, our results showed that all HPV16-positive samples were of the European variant, which was consistent with previously described results in America23. A study from Brazil observed that 29.4 per cent of women with normal cytology were HPV positive, with HPV16 being the most commonly observed genotype (14%), followed by HPV-52 and HPV-4524. In these studies, the observed HPV16 variants were classified predominantly as European (87.5%), but Asian, African and American variants were also reported24. In our study, HPV16 was also the primary viral genotype detected, followed by HPV18.
While European HPV16 variants have been reported in both women with normal cytology and in women with CC, non-European HPV16 variants appear to be associated with a 2- to 9-fold increased risk of CC, as reported in biopsies of Mexican women with CC14. The Asian-American HPV16 D2 variant has been shown to be associated with a high-risk of developing of CC in Mexican women younger than 50 yr old23. Here, we only observed the European HPV16 variant. However, the E350G (or L83V) intra-variant primarily found in our study was not associated with the development of CC in all European populations91025. The higher association of AA and E350G variants and cancer risk may be linked to a better ability to evade the host immune system and/or an increased oncogenic potential associated with intrinsic biological properties of viral proteins1315. In addition, functional studies demonstrated that the E350G E6 variant has biological advantages over the E-P (European-Prototype)242526.
In other study conducted in Latin America in samples of healthy women, a 92 per cent of HPV16 European variant, followed by 4, and four per cent distribution of the AA and Af variants were reported, respectively27. Moreover, similar distribution frequencies of HPV variants in women without cancer have been reported (87, 11 and 2% of infections with the E, AA and Af variants, respectively)26. It should be noted that in studies with CC biopsies performed in Mexico, non-European variants, such as AA and Af, were found in greater proportion (approximately 45%)23. Data showed an association between aggressiveness and the speed of onset of CC with the presence of the AA variant.
In contrast with the data reported in Mexico2327, in this work, all HPV16 samples having the E6 gene sequenced were of the European variant prototype. This could be explained by the fact that, in our study, samples of healthy women were used instead of CC biopsies. These variants are less aggressive than the AA and Af intratypic variants of HPV16 reported in Mexico (23.2% AA vs. 23.8% European)23262728.
One of the limitations of our study was that 53.97 per cent of the women had an inflammatory process and the presence of other pathogens responsible for sexually transmitted infections or immunosuppressed status not clinically confirmed, and we did not analyze other HPV-coinfections that could be present in these women.
In conclusion, a predominance of HPV16 European lineage variants was observed in asymptomatic women from in Sinaloa, Mexico. This variant is known to be associated with a higher risk of developing CC. Molecular diagnoses of HPV may be included in addition to cervical Pap smears as a measure to establish the prognosis of the development of CC in Mexican women.
Acknowledgment
The authors acknowledge all volunteering women participants and thank Dr Omar Fragosa Sosa for allowing us the use of the facilities for sampling and cervical Pap smear analyses.
Financial support & sponsorship: This work was supported by Institutional Funds (PROFAPI2010/110, and 2014/170) and FOMIX CONACyT-Sinaloa (2005-CO1-05).
Conflicts of Interest: None.
References
- 2018. World Health Organization. Cervical Cancer. Available from: http://www.who.int/cancer/prevention/diagnosis-screening/cervical-cancer/en/
- National epidemiological surveillance system. Unique information system. Ministry of Health, Mexico. Cases by State of dysplasia and neoplasm. 2018. Epidemiol Bull. 26:56. Available from: https://www.gob.mx/cms/uploads/attachment/file/386065/sem34.pdf
- [Google Scholar]
- 2018. Direction of Prevention and Health Promotion, Department of Prevention and Control Diseases, Ministry of Health, Sinaloa. II:32. Available from: http://saludsinaloa.gob.mx/saludsinaloa.gob.mx/sitio/epidemiologia-prevencioncontrol.html
- Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518-27.
- [Google Scholar]
- Global burden of human papillomavirus and related diseases. Vaccine. 2012;30(Suppl 5):F12-23.
- [Google Scholar]
- Age distribution of human papillomavirus infection and cervical neoplasia reflects caveats of cervical screening policies. Int J Cancer. 2010;126:297-301.
- [Google Scholar]
- Human papillomavirus genotype attribution in invasive cervical cancer: A retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11:1048-56.
- [Google Scholar]
- Cervical human papillomavirus prevalence in 5 continents: Meta-analysis of 1 million women with normal cytological findings. J Infect Dis. 2010;202:1789-99.
- [Google Scholar]
- Differences in human papillomavirus type distribution in high-grade cervical intraepithelial neoplasia and invasive cervical cancer in Europe. Int J Cancer. 2013;132:854-67.
- [Google Scholar]
- Human papillomavirus genotype distribution in cervical cancer cases in Spain. Implications for prevention. Gynecol Oncol. 2012;124:512-7.
- [Google Scholar]
- Human papillomavirus type 16 variant lineages in United States populations characterized by nucleotide sequence analysis of the E6, L2, and L1 coding segments. J Virol. 1995;69:7743-53.
- [Google Scholar]
- Papillomaviruses and cancer: From basic studies to clinical application. Nat Rev Cancer. 2002;2:342-50.
- [Google Scholar]
- HPV-related carcinogenesis: Basic concepts, viral types and variants. Arch Med Res. 2009;40:428-34.
- [Google Scholar]
- Different association of human papillomavirus 16 variants with early and late presentation of cervical cancer. PLoS One. 2016;11:e0169315.
- [Google Scholar]
- The immortalizing and transforming ability of two common human papillomavirus 16 E6 variants with different prevalences in cervical cancer treatment. Oncogene. 2010;29:3435-45.
- [Google Scholar]
- Human papillomavirus genotype as a predictor of persistence and development of high-grade lesions in women with minor cervical abnormalities. Int J Cancer. 1996;69:364-8.
- [Google Scholar]
- Universal and rapid salt-extraction of high quality genomic DNA for PCR-based techniques. Nucleic Acids Res. 1997;25:4692-3.
- [Google Scholar]
- Geographical variation in human papillomavirus prevalence in Mexican women with normal cytology. Int J Infect Dis. 2010;14:e1082-7.
- [Google Scholar]
- Application of a multiplex PCR to cervical cells collected by a paper smear for the simultaneous detection of all mucosal human papillomaviruses (HPVs) and typing of high-risk HPV types 16 and 18. J Med Microbiol. 2010;59:1303-10.
- [Google Scholar]
- Prevalence and distribution of high risk human papillomavirus (HPV) types 16 and 18 in carcinoma of cervix, saliva of patients with oral squamous cell carcinoma and in the general population in Karnataka, India. Asian Pac J Cancer Prev. 2011;12:645-8.
- [Google Scholar]
- Prevalence of human papillomavirus genotypes in women from a rural region of Puebla, Mexico. Int J Infect Dis. 2009;13:690-5.
- [Google Scholar]
- HPV genotyping and site of viral integration in cervical cancers in Indian women. PLoS One. 2012;7:e41012.
- [Google Scholar]
- Asian-American variants of human papillomavirus 16 and risk for cervical cancer: A case-control study. J Natl Cancer Inst. 2001;93:1325-30.
- [Google Scholar]
- Prevalence of human papillomavirus infection and phylogenetic analysis of HPV-16 E6 variants among infected women from Northern Brazil. Infect Agent Cancer. 2014;9:25.
- [Google Scholar]
- [Distribución de variantes del virus del papiloma humano 16 (VPH 16) en mujeres con y sin neoplasia intraepitelial cervical grado 3 y cáncer cervical] Rev Colomb Cancerol. 2012;16:205-16.
- [Google Scholar]
- E6 molecular variants of human papillomavirus (HPV) type 16: An updated and unified criterion for clustering and nomenclature. Virology. 2011;410:201-15.
- [Google Scholar]
- [Infección por virus del papiloma humano en una muestra de mujeres jóvenes con citología normal] Rev Colomb Cancerol. 2004;8:3-4.
- [Google Scholar]
- Impact of human papillomavirus coinfections on the risk of high-grade squamous intraepithelial lesion and cervical cancer. Gynecol Oncol. 2014;134:534-9.
- [Google Scholar]






