Translate this page into:
A fascinating story of the discovery & development of biologicals for use in clinical medicine
For correspondence: Dr Anand N. Malaviya, Department of Rheumatology, ISIC Superspeciality Hospital, Vasant Kunj, New Delhi 110 070, India e-mail: anand.malaviya@yahoo.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A young physician starting a fresh career in medicine in this millennium would hardly stop to think about the genesis of a particular biological drug that he/she will be prescribing for a patient evaluated in the morning outpatient department. For him/her, this is now routine, and the question of ‘Who’, ‘How’ and ‘When’ about these biologicals would be the last thing on their mind. However, for those who came to the medical profession in the 1950s, 1960s and 1970s, these targeted drugs are nothing short of ‘miracles’. It would be a fascinating story for the young doctor to learn about the long journey that the dedicated biomedical scientists of yesteryears took to reach the final destination of producing such wonder drugs. The story is much like an interesting novel, full of twists and turns, heart-breaking failures and glorious successes. The biologicals acting as ‘targeted therapy’ have not only changed the natural history of a large number of incurable/uncontrollable diseases but have also transformed the whole approach towards drug development. From the classical empirical process, there is now a complete shift towards understanding the disease pathobiology focusing on the dysregulated molecule(s), targeting them with greater precision and aiming for better results. Seminal advances in understanding the disease mechanism, development of remarkably effective new technologies, greater knowledge of the human genome and genetic medicine have all made it possible to reach the stage where artificially developed ‘targeted’ drugs are now therapeutically used in routine clinical medicine.
Keywords
Biological drugs
drug discovery
history of medicine
infliximab
monoclonal antibody
tumour necrosis factor-α
Introduction
Most orally administered drugs are organic compounds with a relatively small molecular weight (usually <500 g/mol), except calcineurin inhibitors that have a slightly higher molecular weight (but still <1000 g/mol). These molecules are chemically synthesized in laboratories without using any biological systems. Indeed, orally taken small molecules are easily absorbed by diffusion through the intestinal lining. Although the gut can ingest large molecules through the process of endocytosis, use of this delivery system for orally administered drugs is yet to find its way in clinical medicine. Therefore, drugs with a large molecular weight perforce need to be administered parenterally. Biologicals, a new category of drugs that are not synthesized chemically in the laboratory, need biological systems for their production. These are ‘targeted’ drugs that ‘home’ on and bind to a specific key molecule involved in the pathogenesis of that disease. These drugs have been named ‘biological response modifiers’ or ‘biologicals’ in short. Since their addition in the armamentarium of the clinicians around the end of the 20th century and the beginning of the millennium, these drugs have revolutionized therapy and significantly influenced the outcome of several so-called ‘untreatable diseases’ across all the medical specialities. These drugs are now widely used in routine day-to-day medical practise. Yet, only a few might actually know the underlying fascinating story of scientific discoveries of the past few decades that made it possible to develop these drugs. This review attempts to recreate the successes and travails of a large number of medical scientists whose astute observations and painstaking work over decades culminated in the production of a clinical-grade monoclonal antibody (mAb) that was highly specific against a key molecule in the pathogenesis of rheumatoid arthritis (RA), namely the tumour necrosis factor-α (TNF-α). The rest as they say is history.
Biological drugs
Definition of a biological drug as provided by the National Cancer Institute (NCI, USA) is ‘a substance that is made from a living organism or its products and is used in the prevention, diagnosis, or treatment of cancer and other diseases. Biological drugs include antibodies, interleukins (ILs), and vaccines; also called biologic agent and biological agent’ (https://www.cancer.gov/publications/dictionaries/cancer-terms/def/biological-drug). It may be mentioned that agents used in clinical therapeutics and derived from living beings are not a new phenomenon in medicine. ‘Serum therapy’ or ‘antitoxin therapy’ was first discovered by Shibasaburo Kitasato (1852-1931) and Emil von Behring (1854-1917) using serum from animals (usually sheep or horse) injected with appropriate antigens to produce the desired antibodies. This method of treatment was widely prevalent in the last two centuries1. Indeed, diphtheria, tetanus and rabies antitoxins continue to be used even today. Not only was the method of producing such sera and their purification process tedious and time-consuming, but also the main disadvantage was the frequent appearance of a disease often called ‘serum sickness’, caused by the body's immune response to foreign (animal) proteins. Based on pure nomenclature, even the clotting factors used in bleeding disorders and several growth factors (used in haematology and other disciplines) are biologically derived. Even the older insulin, used widely for decades, was a biologically derived molecule (from the pancreas of pigs).
Monoclonal antibodies (mAbs)
With rapid advances in biotechnology along with complementary DNA (cDNA) cloning of the relevant molecules, substances such as insulin (and several others including erythropoietin) can now be synthesized without involving the biological systems (e.g. cell cultures, genetically modified bacteria, and yeast cells). However, conceptually, if treatment requires highly specific antibodies (derived from a single clone of antibody-producing plasma cells against aberrant molecules in the body leading to pathology), an in-depth understanding of the biological processes involved is essential for producing monoclonal antibodies (mAbs) in large amounts. The mAbs are now widely used in the treatment of a large number of diseases encompassing almost all speciality/super-speciality boundaries in medicine. Nevertheless, modern-day young physicians may not be fully aware of the seminal contributions and painstaking efforts of a dedicated group of passionate clinicians, biologists, biochemists, molecular biologists and pharmacologists, who made it all possible. The story of the development of biologicals is that of a remarkable breed of researchers who, despite several heart-breaking failures, ultimately succeeded in discovering a family of new therapeutic molecules that have not only changed the treatment landscape of a large number of chronic ‘untreatable’ diseases but have also provided new leads for ‘targeted therapy’. These monumental discoveries have changed the way the medicine is practised today. This review highlights the salient historical events during the development of first such therapeutic mAb, an anti-TNF-α, that was given the name ‘infliximab’.
Biotechnology made it possible
The advent of several path-breaking technologies has made it possible to develop new biologicals. While most of these were developed for different objectives and variable research needs, the story of their discovery and the key researchers involved are both interesting and educative.
Tissue culture and the study of culture supernatants
Tissue culture has been central to the study of cell biology, particularly for understanding the cellular function in health and disease. Wilhelm Roux, a student of Rudolf Virchow (a German physician with lifetime contributions in experimental embryology), was the first to successfully grow medullary plate of an embryonic chicken in the laboratory in 18852. This discovery was followed by the ‘hanging drop’ method of cell culture developed by Ross Harrison, an American biologist and anatomist credited to be the first to work successfully with artificial tissue culture in 19073. From 1911 to 1935, the tissue culture technique reached a level of sophistication that made it the pivot for the study of cell physiology and behaviour. During this period, several other dedicated biologists contributed significantly towards making the technique more user-friendly. One of them was Alexis Carrel, a French surgeon and biologist who won the Nobel Prize (1912) and pioneered the culture techniques to perfection4. Carrel worked at the Rockefeller Institute from 1906 to 1927 and teamed up with Montrose Burrows (1911), a US surgeon and pathologist with special interests in cancer research. Together, they developed the long-term aseptic technique of in vitro cell culture4. Burrows is credited with coining the phrase ‘tissue culture’ and was among the first to adapt the technology to the study of tissues from warm-blooded animals4. From the standpoint of rheumatology research, Vaubel at the Rockefeller Institute Hospital was the first to study synovial cells in tissue culture way back in 1933. He is credited with the description of two distinct cell types in the synovial tissue, namely a fibroblast-like synoviocytes (FLS) and a macrophage-like synoviocytes (MLS)5.
Intercellular cross-talk and the concept of cytokines
While the technique for long-term cell cultures was being developed during the early 20th century, it was soon realized that the harvested culture supernatants provided a rich source of molecules secreted by cells. This observation led to a plethora of studies defining their biological properties. Most of these were found to be small protein molecules (~5-20 kDa). In the absence of a defined system of nomenclature, different investigators gave different names, often two different names for the same molecule. In 1974, Cohen6 an American (New Yorker) biochemist and 1986 Nobel Laureate along with his colleagues coined the term ‘cytokine’ to designate products of cell cultures. They argued that many non-leucocyte cells in the body could also produce cytokines. Strictly speaking and depending on the cell types involved, the ‘cytokine umbrella’ encompasses besides cytokines, the chemokines, interferons (INFs), ILs, lymphokines, TNF, and others7. At that time, it was speculated that these molecules must be involved in cell signalling (‘cross-talk’ between cells) and could thus be considered ‘short-range’ hormones (autocrines, paracrines) that influence the functioning and behaviour of the neighbouring cells8. However, to date, the terminology of these molecules remains in flux, and many different names have been popular including migration factors, lymphokines, monokines, ILs, chemokines, autocrines, and paracrines. These are also named after the tissue in which they are found, for example, neurokines, adipokines, and others. Conventionally, hormones and growth factors are not included under the head ‘cytokines’.
Impact of the discovery of cDNA cloning - Obtaining molecules in the purest form
For studying molecules in different tissues in health and disease, tracer antibodies raised in small laboratory animals have conventionally been used. However, there were inherent problems of specificity and batch-to-batch variation for the use of these ‘polyclonal’ antibodies. This problem was soon resolved with the discovery of DNA cloning technology, capable of generating pure molecules. Although it is beyond the scope of this review to discuss biotechnological cloning methods for the production of pure forms of molecules and proteins, suffice to say that without these sophisticated techniques, it would not have been possible to conduct high-class basic research, leading to the production of pharmaceutical-grade biologicals for clinical use. One such technique for the production of specific antibody molecules that uniformly (clonally) carry the same three-dimensional structure (e.g. the same heavy and light chains, as well as the variable and hypervariable regions along with the same glycosylation pattern reacting exactly with the same epitope of the given antigen) was the discovery of the Nobel Prize-winning technique called ‘Hybridoma Technology’. However, before we dwell on the story of hybridomas, there is a lot to discuss about cytokines.
Discovery of IL-1, TNF-α/cachectin and their receptors - Cohen's (Nobel Laureate) and Jean-Michel Dayer's contributions
The history of the discovery of cytokines goes back to the early 20th century when tuberculosis and tuberculin research was gaining strength. The work of Zinsser and Tamiya9 and Arnold Rich in 1926-192710 on ‘permeability factor’ released by tissues sensitized by tuberculin might have been the first clear demonstration of what we call today, the ‘cytokine effect’. From 1957 to 1974, several investigating groups reported on the functional aspects of molecules secreted by ‘stimulated’ (sensitized) cells using different biological systems. Isaacs and Lindenmann11 while working with live influenza virus grown in chicken embryo chorioallantoic membranes observed that cells pre-treated with heat-inactivated influenza virus inhibited the growth of live influenza virus. They conjectured that the phenomenon was mediated by a protein released by cells in the chorioallantoic membrane that was pre-treated with heat-inactivated influenza virus. They named it ‘interferon’ (interference with the growth of the virus)11. Byron Waksman and Margit Matolfsky (1958) showed that tuberculin sensitization of macrophages, instead of causing damage, led to their stimulation (macrophage activation)10, a mechanism earlier utilized by Freund and McDermott12 as an adjuvant for boosting an immune response to weak antigens. In 1966, migration-inhibitory factor that inhibited the migratory property of normal macrophages was discovered1314. Soon in 1968, several groups almost simultaneously discovered a protein secreted by stimulated lymphocytes, which they named ‘lymphotoxin’1516 that was later renamed as ‘TNF-β’17. Dudley Dumonde (1969) is credited with the use of ‘lymphokine, monokine’ terminology1018. He defined them as non-antibody mediators of cellular immunity generated by lymphocyte activation possibly pointing to lymphocytes of the innate immune system. While working in the laboratory of Byron Waksman in 1972, Igal Gery, described a ‘lymphocyte-activating factor’ (LAF)19. Soon after in 1974, Cohen introduced the term ‘cytokine’ as discussed above. Indeed, the saga of cytokines is replete with the names of Cohen and Byron Waksman; the former earned the Nobel Prize, while the latter went onto become a legendary physician-immunologist from New Haven, Connecticut, USA.
Besides the basic scientists including biochemists and molecular biologists, many of those who contributed significantly in this field were clinicians interested in autoimmune diseases. At this point in time, several new departments got established around the world with the designation ‘Rheumatology and Clinical Immunology’ or vice versa. Some of the prominent names include Division of Clinical Immunology and Rheumatology, University of Alabama, Birmingham; Department of Rheumatology and Clinical Immunology, Charité - University Medicine Berlin; UMC Utrecht Rheumatology and Clinical Immunology; Amsterdam Rheumatology and Immunology Canter; Rheumatology and Clinical Immunology, University of Groningen, The Netherlands, and many others. For those engaged in this field, RA was the main disease that needed to be better understood for developing effective treatment modalities. Incidentally, joints are relatively easily accessible for obtaining tissue (pathologic synovial membrane) for deciphering the pathogenesis of synovitis and pannus that erodes the cartilage and bones in joints. Obviously, synovial tissue was the earliest to be grown in tissue culture to understand its physiology and pathology in diseases such as RA. In this regard, the work of Vaubel5 in successfully culturing the synovial tissue in the laboratory has already been mentioned.
Till the late 1960s, the pathogenesis of RA was being debated from gum infection (this theory has seen great revival in recent times with Porphyromonas gingivalis as the possible culprit) to abnormal extracellular matrix (ECM) caused by alterations in enzymes, proenzymes and possible auto-activation, exposing the altered antigens of ECM and thus causing autoimmunity. It needs to be reminded that in 1962, interstitial collagenase (now called metalloproteinase-1 or MMP-1) had already been discovered along with its property of altering tissue structure20. The legacy of ‘abnormal extracellular matrix’ in those days had translated in the name of ‘collagen diseases’ that we call today systemic immunoinflammatory diseases (two categories: autoimmune inflammatory diseases and auto-inflammatory diseases). However, advances in enzymology (1970s-1980s) and their application in RA refuted any direct role of altered enzymes in ECM damage. One had to go back to the ‘cells in rheumatoid synovium’ especially the pannus that was central to the process of joint destruction. However, the burning question at the time was ‘How do cells in the pannus (immune cells, inflammatory cells) cause damage to the ECM?’
In 1974, Dayer et al2122 from the Faculty of Medicine, University of Geneva, Switzerland, joined the famous Arthritis Unit at Massachusetts General Hospital headed by Krane. Here, Dayer and colleagues studied the synovial cultures from patients with RA and discovered that synovial fibroblasts were able to produce large amounts of collagenase and prostaglandin E2 (PGE2). They demonstrated that physical contact of synovial fibroblasts with mononuclear cells was essential for the accelerated production of collagenase and PGE2, a process that becomes autonomous (start to behave like tumour cell) with the passage of time. They succeeded in purifying a small 15 kDa molecule that acted as the sensitizer/stimulator for the synovial fibroblasts to produce large amounts of collagenase and PGE2. The molecule was termed ‘mononuclear cell factor’ or MCF2122. Based on the detailed chromatographic studies, MCF was re-christened as IL-1 at the Second International Lymphokine Workshop held in 1979 in Ermatingen, Switzerland23. Again, while analyzing the respective function of mononuclear cell subpopulations, Nardella et al24 demonstrated that T-lymphocyte-stimulated monocyte-macrophages (MΦ) produced MCF, thus establishing the sequential pathways from TL → MΦ → synovial fibroblast activation, where direct physical contact of the mononuclear cells was essential. This paradigm for the joint disease in RA still holds true even after >40 yr2526. The contribution of humoral immune response (B-cell involvement) was later added to the schema when self-associating IgG isotype rheumatoid factor was shown to directly stimulate MΦ that activate synovial fibroblasts without the requirement for T-cells2427. Seckinger et al28 also discovered the first IL-1 receptor antagonist (IL-1Ra) and subsequently described how a natural cytokine antagonist blocked the binding of another cytokine from the same family. Thus, the principle of the competitive binding assay of the IL-1 inhibitor to IL-1 at the receptor level was developed. The observation was crucial for researchers at Synergen, a biotechnology company at Boulder, Colorado, USA, who purified and cloned IL-1Ra in 199010. Cloning of cDNA of IFN-α and IFN-β in 1980 and of cDNA of T lymphocytes (TNF-β) and TNF-α and IL-1 was achieved in 1984, followed by that of IL-1Ra in 1990. These were remarkable discoveries, and since then, the recombinant molecules and specific mAbs have revolutionized the field of signal transduction and the dissection of the hierarchy of different cytokines depending on the type of disease and therapeutic approaches. A key observation of Dayer et al was related to the behaviour of synovial fibroblasts in RA2122. As already mentioned, he showed that normal synoviocytes exposed to MCF show striking morphological changes, become elongated with modified spatial structure and start producing large amounts of collagenase (MMP-1) and PEG2. Such modified cells are called synovial fibroblasts. More importantly, Croft and colleagues29 demonstrated that after a period of continuous exposure to MCF, this subpopulation of synovial fibroblasts switches to an autonomous pattern of cell growth with evidence for the expression of different genes and a variable pattern of response to different cytokines. One wonders that with such elegant work of Dayer, (Fig. 1) was it simply bad luck that later studies involving inhibition of MCF (later renamed IL-1) could not find a discernible effect in controlling rheumatoid disease? However, that is a different story (discussed below).

- Dr Jean-Michael Dayer (Photograph personally provided for use in this article).
Coining of the term TNF - work of Lloyd Old's and Anthony Cerami's teams including Jean-Michel Dayer and Bruce Beutler (Nobel Laureate)
There has been some confusion among biologists regarding the discovery and coining of the term TNF. In hindsight, the reason for this confusion is easy to understand. Historically, it was Carswell et al30 at the Memorial Sloan-Kettering Cancer Center, New York, who published their seminal work in the prestigious ‘Proceedings of the National Academy of Science USA’ in 1975. Using the model of sarcoma Meth A and other transplanted tumours caused by endotoxins, they demonstrated that mice primed with substances inducing non-specific hyperplasia of the reticuloendothelial system (e.g. BCG, Zymosan, Corynebacteria) release a substance that caused haemorrhagic necrosis mimicking the effect of endotoxin itself. They gave it a name, ‘tumour necrosis factor’ or simply TNF, not the best of names yet; this is the name being used until today. Being an experimental finding in mice, it failed to receive the desired attention of the researchers. Exactly 10 years later, Beutler et al31 at the Rockefeller University, New York (just across the street from Lloyd Old's laboratory at the Memorial Sloan-Kettering), published the first demonstration of the important role of TNF in the pathogenesis of disease. The significance of the work done by Beutler and his colleagues on TNF was elegantly emphasised by Jan Vilček in 2008.32 Having something to do with disease pathogenesis, the discovery of TNF caught the imagination of basic researchers and clinicians alike around the world. There are two important points about the paper by Beutler et al31: (i) the first author Bruce Beutler together with Jules A. Hoffmann went on to share the 2011 Nobel Prize in Physiology or Medicine for ‘their discoveries concerning the activation of innate immunity’, (ii) the paper appeared exactly 10 yr after the report from Lloyd Old's Laboratory that had described and used the term ‘TNF’. In all fairness to Beutler and colleagues, they had simultaneously used the term cachectin and TNF in this 1985 paper. Cerami must be credited for building a team of brilliant biologists and immunologists that had besides Beutler, others including the famous Swiss scientist Jean-Michel Dayer (his work already described above). This group published a series of papers describing a lipoprotein lipase-suppressing hormone secreted by endotoxin-induced RAW 264.7 cells that they named ‘cachectin’. Nevertheless, they also mentioned the name TNF for the same molecule333435 (Figs 2 and 3).

- Dr Anthony (Toni) Cerami (Photograph personally provided for use in this article).

- Dr Bruce Beutler (Courtesy: Brian Coates for UT Southwestern medical Center).
Most endeavours of great value require some inspiration, a lot of perspiration and a little bit of luck. Cerami's main work was on ‘Neglected Tropical Diseases’ for which he frequently travelled to Africa making Kenya as his base station. There he became interested in the dramatic wasting in cattle suffering from African sleeping sickness caused by protozoa, Trypanosoma brucei spread by Tsetse flies. He established that the blood of these cattle carried a molecule that caused wasting. Further work on this molecule led to the discovery of ‘cachectin’. It was then argued that if a neutralizing antibody to cachectin is administered, the cachexia (and the other ill effects of cachectin) could be reversed. However, most devastatingly, in his experiments in Kenya, the administration of antibodies against cachectin to cattle suffering from ‘sleeping sickness’ caused their death. The failed experiment was a great deal of disappointment for team-Cerami36. The failure of cachectin/TNF antibody in the treatment of sepsis became one of the main stumbling blocks for several investigators in later years including Ravinder Nath Maini and Marc Feldmann when they wanted a small amount of mAb against TNF for human trials in another disease namely RA. Most Biotechnology Companies did not agree to initiate clinical trials in humans. In later studies on the use of anti-TNF in sepsis in mice, it became clear that the issue had to do with the timing of administration of antibodies; given before the onset of sepsis, it completely prevented the clinical features but not in an established infection31. However, by then, the reputation of mAb as therapeutic agents had taken a hit.
Purification and cDNA cloning of TNF: Meeting of 25 scientists at the Memorial Sloan-Kettering Cancer Center, New York, December 1984 - Lloyd Old and Jan Vilček to the fore
Vilček37 had just completed medical graduation in 1958 in Bratislava (in the Old Czechoslovakia) when he attended talks by Alick Isaacs, the co-discoverer of INF, and Albert Sabin, best known for the development of live polio vaccine. He got highly motivated and started working in the field of INFs. While still in Bratislava, he published a brilliant paper on INF in the next three years38. In 1964, he migrated from communist Czechoslovakia to the United States and joined the New York University (NYU) School of Medicine as Assistant Professor to fulfil his zest for advanced basic research in biological systems. In 1982, his team had already done advanced research in INFs describing the two types, IFN-α and IFN-β (now known as type-I INFs). During the production of these INFs by mononuclear cells by the prevailing laborious cell culture methods of that time, his team observed an additional molecule that they called ‘immune INF’ (or INF-γ now known as type-II INF). On further analysis, there were two different molecules; one produced by the lymphocytes and the other by monocytes. In 1984, his team named the former as ‘lymphokine’ (was also known as TNF-β) and the latter as ‘monocyte-derived cytotoxin’ that subsequently turned out to be the classical TNF now called TNF-α39. This was a unique effort involving nine scientists from three different laboratories across USA (Department of Microbiology, NYU School of Medicine; Developmental Hematopoiesis Laboratory, Sloan-Kettering Institute for Cancer Research, New York; and the department of Protein Biochemistry, Genentech, Inc., South San Francisco, California, USA). In December 1984, Lloyd Old and colleagues at the Memorial Sloan-Kettering Cancer Center organized a small workshop that was attended by scientists interested in TNF and lymphokines. It included several authors of the above-mentioned paper including Bharat Bhushan Aggarwal of the Protein Biochemistry Department of the Genentech Corp, California, USA. It was during this workshop that Bharat announced the seminal work on the first complete amino acid sequence of human TNF, the partial sequence of human lymphotoxin protein and cDNA sequences, the chromosomal location of the TNF and lymphotoxin structural genes by his colleague scientists at the Genentech4041. Since that historical workshop, Vilček developed an active ongoing collaboration with Genentech, including one with Bharat Aggarwal and David Goeddel, who provided samples of the pure form of recombinant human TNF. This greatly facilitated studies on understanding the biological function and mechanism of action of TNF in Vilček's Laboratory. Till then, the only thing known about TNF-α was their cytotoxic action on some tumours and cachexia in chronically infected animals35. For deciphering the biological actions of TNF, it was essential to study different cells to find out which ones had on their surface specific high-affinity binding receptors. Two easily available human cell lines in Vilček's laboratory were (i) the HeLa cell, an immortal cell line from a patient with cervical cancer who had died in 1951 (HeLa cell line is one of the most common and the oldest human cell line available in tissue culture and is used widely in laboratories around the world), (ii) FS-4 strain of human diploid fibroblasts cell-line that was grown in Vilček's Laboratory42. These cells showed high-affinity receptors for TNF. Further experiments in Vikcek's laboratory showed that INF-γ synergizes the cytotoxic action of TNF by increased expression of TNF receptors43. In the case of human diploid FS-4 fibroblasts, an exposure of even nano mol strength of TNF caused a stunning change in the cell morphology, which could be noticed even under a light microscope. The fibroblasts became elongated with a change in their spatial orientation. A student at Vilček's Laboratory, Vito Palombella, demonstrated similar morphological changes even in normal human fibroblasts exposed to TNF44. Lin and Vilček also showed that like other growth factors, TNF led to an increased expression of c-Fos and c-Myc mRNA in human fibroblasts45. Their subsequent work showed that TNF induced a large number of genes in different human cells and was also a strong inducer of a molecule that later came to be known as IL-6, a strong inducer of inflammation including acute-phase reactants46 (Figs 4 and 5).

- Dr Jan Vilček (Photo credit: Peter Hurley, provided by Dr Jan Vilček personally for use in this article).

- Dr Bharat Bhushan Aggarwal (Photograph personally provided for use in this article).
Nature's experiment: Multiple myeloma-The natural monoclonal antibodies (mAbs)
The story of the discovery of biologicals for clinical use cannot be complete without mentioning the legendary clinical immunologist-physician Henry Kunkel (of ‘Kunkel-girls’ fame, ‘guru’ of a whole generation of American clinical immunologists and autoimmune experts in 1970s-1980s) of Rockefeller Institute, New York. In 1951, he had made a unique observation that malignant plasma cells harvested from the bone marrow of patients with multiple myeloma not only had their antibody-making machinery intact but that also all cells produced identical antibody molecules in every parameter tested47. Serum electrophoresis of these patients showed a ‘monoclonal (M)-spike’. Thus, myeloma was recognized as one of the ‘monoclonal gammopathies’, and myeloma cell lines became the main source of studies on antibodies. This was made even simpler by a serendipitous discovery by Michael Potter (a molecular biologist at the NCI, Bethesda) who in 1962 reported that injecting mineral oil in the peritoneal cavity of a particular strain of mice (BALB/c) induced the growth of myeloma cells. His laboratory thus became a source of several lines of myeloma cells for researchers around the world. The propagation of these cells was made easier by establishing an in vitro culture technique by Kengo Horibata and AW Harris (under the supervision of Melvin Cohn at the famous Salk Institute, San Diego)48. These cells continuously produced antibodies in a clonal pattern using different heavy chains and light chains specific for each clone. However, the exact specificity of these antibodies could not be established. Indeed, determining their specificity out of a billion possible antigens and their epitopes would have been like finding a needle in a haystack. The principal question in the mind of most researchers of the time was, ‘Could one re-direct the clonal antibody producing machinery of these immortal myeloma cell lines to make antibody to a single specified epitope’? That way one could solve all the difficulties of purifying polyclonal antibodies produced in either horses or small laboratory animals and make them relatively specific for directed research on cells and molecules.
Path-breaking discoveries by Sinkovics, Askonas, Klinman and Niels Jerne on the generation of monoclonal antibodies (mAbs)
In 1970s, most investigators in the field of antibodies and antibody-producing cells (later called B cells) had recognized the prime need for producing large amounts of antibodies with known specificity to a particular antigen, unlike myeloma cell lines where specificity of the antibodies remained unknown. Some of the prominent names engaged in this research included Joseph Sinkovics, Brigitte Ita Askonas and Norman Klinman.
Sinkovics, a Hungarian immunologist based at the M.D. Anderson Hospital and Tumor Institute in Texas, reported in 1970 successful natural fusion of a splenic plasma cell with the mouse lymphoma cells49. Although the secreted antibodies were highly specific and functional, their work failed to catch the imagination of others in the field of cell fusion. The credit for using the term ‘hybridoma’ goes to Sinkovics50 who generated a hybrid cell that was capable of producing mAb and had imbibed the quality of immortality of a malignant cell.
Brigitte Ita Askonas was an Austrian by birth51. However, with the increasing Nazi influence and after a short stay in Paris, she migrated to Montreal, Canada, to work as a researcher at the McGill University and obtained her degree in Biochemistry. After a stint at the Basel Institute of Immunology, Switzerland, she moved to Cambridge University, UK, where she worked for her PhD. Finally, she moved to the National Institute of Medical Research, Mill Hill, London, in 1952 and worked in the chemistry division till 1989. She was interested in the study of antibody synthesis in vivo. While working with myeloma cells and through the background knowledge of Kunkel's work in the 1950s and her own vast experience in biochemistry, she was the first to elucidate biochemical steps involved in the synthesis of immunoglobulin molecules within the antibody-producing plasma cells (progeny of B-cells). She was also the first to demonstrate that a single antibody-producing cell clonally produced a single (monoclonal) type of antibody, the work for which she was elected a Fellow of the Royal Society in 1973. While at Mill Hill, she made several other seminal discoveries related to antibody heterogeneity. Historically, she was the first scientist to have produced a mAb in the laboratory. For this work, she used the genetically identical irradiated mice to produce the mAbs52. However, for reasons not obvious, her work failed to receive the due recognition. One possible reason could have been that these antibody-producing clones were fragile, not surviving for an adequate length of time to be used for bulk production of mAbs (Fig. 6).

- Dr Brigitte Ita Askonas (Courtesy: Sir Marc Feldmann, and reproduced with permission from Eur J Immunol).
Norman Klinman, an American immunologist, based at the University of Pennsylvania with joint attachment to the Wistar Institute, published a technique in 1969, which he called ‘monofocal antibodies’53. He used irradiated mice that were injected with fresh cells with antibody-producing capacity, some of which ‘homed’ in the spleen. This spleen was cut in small cubes and placed in tissue culture that contained a specific antigen. The hypothesis was that the spleen fragment that contained a specific antibody-producing cell would produce antibodies specific to that antigen and these could then be harvested from the culture supernatants and used for experiments5354.
AlthoughNiels Jerne (First Director of the Basel Institute of Immunology) was not directly involved in the development of therapeutic mAbs (biological disease-modifying drugs or bDMARDs), his ‘Natural Selection Theory’ of antibody specificity had put him among the best minds in the field of immunology. He shared the 1984 Nobel Prize with Köhler and Milstein for their work on the important contribution of theory and practice in shaping our understanding of the body's immune system (Figs 7 and 8). Jerne's haemolytic plaque technique (in soft agar plates) was an elegant method of studying single mAb-producing cells and their biology. The technique was widely used to study the monoclonality and specificity of the produced antibodies [The first author (ANM) while working at the New England Medical Centre, Boston, in 1968, used the Jerne-plaque technique extensively for his work on ‘Lifecycle of antibody-producing cells’55].
![Dr Niels K. Jerne [The photograph kindly provided by Prof. Thomas Söderqvist; it is also published in the biography of Jerne: Science as Autobiography (Yale University Press, 2003)].](/content/175/2018/148/3/img/IJMR-148-263-g007.png)
- Dr Niels K. Jerne [The photograph kindly provided by Prof. Thomas Söderqvist; it is also published in the biography of Jerne: Science as Autobiography (Yale University Press, 2003)].
- César Milstein and Georges JF Köhler (Kindly provided by Ms Celia Milstein for use in this article).
César Milstein and Georges J. F. Köhler: Hybridoma technology and production of monoclonal antibodies (mAbs) - The 1984 Nobel Prize
Much of the story described in this section has been comprehensively narrated by Lara Marks56, a summary of which is recounted here. César Milstein, an Argentinian biochemist (1927-2002), had graduated from the University of Buenos Aires and obtained his PhD in 1956. Funded by the British Council, he moved to the United Kingdom in 1958, became a naturalized British citizen and joined the Biochemistry Department of Darwin College, University of Cambridge. He also had a short-term appointment with the Medical Research Council (MRC). From the late 1960s, his research revolved around the fascinating subject of antibody diversity and the mechanism of its generation. The ‘germline’ versus ‘somatic-mutation’ theory was indeed the moot question under great debate by the immunologists of the day. Those were also the days when the first author of this paper (ANM), undertook a ‘primer’ course in immunology in Boston and was thus privy to hot debates on ‘germline versus somatic-mutation’, the two theories being the major basis of antibody diversity57. Based on simple common sense, the famed American molecular biologist, Joshua Lederberg in 1959 argued in favour of somatic mutations as the basis of antibody diversity because otherwise Nature cannot be wasting innumerable genes only to produce a diverse range of antibodies. Soon after, Brenner (Harvard) and Milstein (Cambridge) published the now-famous ‘Brenner-Milstein model’ for the generation of antibody diversity58. For further details, one might refer to the landmark paper on the life history of César Milstein published by Neuberger59.
In the early 1970s, Dick Cotton a postdoctoral fellow investigator from Australia with interest in immunogenetics joined Milstein's Laboratory, and together, they perfected the technique of cell fusion using a variety of myeloma cell lines. The technique involved the use of inactivated Sendai virus that he obtained from Abraham Karpas working in the laboratory next door, who used it to promote cellular fusion. In 1973, Milstein presented their work on myeloma cell fusion at the Basel Institute of Immunology (Niels Jerne was the Director of the Institute). In the audience was a young German biologist, Georges Köhler, who was completing his PhD from the University of Freiburg. Excited by Milstein's work, Köhler joined his research team in Cambridge in April 1974 as a postdoctoral scientist to carry forwards the research on antibody diversity. For proving the hyper-mutation theory, they needed immortalized antibody-producing cell lines. By this time, Milstein had already obtained Potter's mouse myeloma cell line (MOPC21) that Horibata and Harris had used to establish long-term tissue culture during the early 1970s56. Working with Brownlee, Milstein was able to establish the myeloma cell line, but the problem was that these were making antibodies against unknown antigens as discussed earlier.
By the time Köhler joined Milstein's Laboratory, the hybridoma technology had already been established in several laboratories around the world. However, these two were struggling to discover a hybrid cell that must have three basic properties: (i) induction of immortality for synthesis of an antibody molecule, (ii) it must have the properties of producing a single antibody molecule, i.e. a specific mAb, and (iii) it should be able to grow in tissue culture for indefinite periods. Using the techniques of isolating single antibody-forming cells from sheep red cell immunized mice spleen fragments (Klinman technique described above) and the already established cell-fusion technique with Sendai virus perfected in their laboratory by Dick Cotton and Abraham Karpas (with skilled technical assistance provided by Shirley Howe), Köhler and Milstein succeeded in producing ‘hybridomas’ that could make mAbs against certain antigens of sheep red cells. With such positive results in their hand (proven by using the Jerne haemolytic plaque technique), these two biologists suddenly realized that they had successfully discovered a tool that everybody else had been striving to make for many years. In critical scientific terms, they had developed an immortal antibody-producing cell line that was capable of producing an endless supply of identical antibodies with known specificity. The method would soon become popular under the name ‘hybridoma technology’. The antibodies thus produced were named ‘mAbs’ signifying that they were derived from a single hybrid cell. Köhler and Milstein60 published their epoch-making discovery in 1975 for which they were awarded the Nobel Prize in 1984, which they shared with Niels Jerne who had laid down the theoretical framework years before their discovery. Although these hybridomas could be propagated indefinitely in large amounts, there was a small problem due to the dwindling supply of Sendai virus in Milstein's Laboratory. Further, the Sendai virus inactivation and its use for cell fusion were tedious. As luck would have it, Giovanni Galfré, a postdoctoral student who had recently joined Milstein, resolved the issue by using polyethylene glycol (PEG), a chemical that had been used successfully in other cell-cell fusion experiments. Galfré's introduction of PEG significantly enhanced the hybridoma technology for generating immortal mAbs on an unprecedented scale. The discovery of mAbs heralded a major advance over the conventional polyclonal antibodies.
Saga of monoclonal antibody (mAb) patent - A jarring note in a flawless melody
In 1975, Milstein presented his work on hybridoma technology at an internal meeting of the MRC, UK, the laboratory where this discovery was made. Tony Vickers, a scientist by training, was working as an official in the Administration Department of MRC47. Realizing the immense commercial value of the discovery, he alerted the National Research Development Corporation (NRDC), the body responsible for patenting MRC inventions. To the great disappointment and surprise of the MRC administration, the reply from NRDC (dated 7th October 1976 later tracked down, the details of which can be accessed47; the subject heading of the NRDC reply letter was ‘Continuous Culture of Fused Cells’) was rather disheartening. It read and we quote47 ‘It is certainly difficult for us to identify any immediate practical application which could be pursued as a commercial venture,……and it is not immediately obvious what patentable features are at present in the Nature paper’. In hindsight, this misjudgement about hybridoma technology might have caused a loss of billions of dollars to British economy!
In those early days, investigators took ethics in science extremely seriously and any thoughts about the commercial exploitation of a discovery would have been considered ‘sinful’. Indeed, there was free exchange of thoughts/ideas and research methods among scientists across the world with little worry about intellectual property or methodological copyrights. In such a scientific atmosphere of free exchange of ideas and material, Milstein in September 1976 received a request from Hilary Koprowski, a scientist working at the Wistar Institute, Philadelphia (founded in 1892 and now a NCI-designated Cancer Centre affiliated to NYU since 1972), for parting with some of his hybridoma cell lines. In the spirit of ‘free exchange in science’, Milstein immediately dispatched a hybridoma cell line to Koprowski; and the rest, as they say, is history47. Koprowski (1913-2013) was a Polish scientist who pioneered the development of oral polio and modern rabies vaccines. In the history of the discovery of mAbs, it is mentioned that Hilary Koprowski, Carlo Croce and Walter Gerhard were granted two patents (October 1979 and April 1980) for making mAbs against tumours and influenza virus. This was the first time ever that the scientists were granted any patents for producing mAbs. Almost simultaneously, Koprowski also co-founded Centocor, one of the first biotechnology companies for commercial production of mAbs for diagnostics and therapeutics [‘Remicade’ (infliximab), the first biological used in the treatment of RA is a Centocor product]. It was a pity that Köhler and Milstein's contributions were not acknowledged. It may be mentioned that 1970s were the days of political and economic anxiety for Britain. The failure to patent such an important discovery raised a political storm in the country that ultimately reached the then Prime Minister Margaret Thatcher's (a chemist by training) desk. To say the least, she was furious;a great opportunity was missed by Britain47.
Monoclonal antibody (mAb) against TNF-α, ‘infliximab’
Vilček's contributions to the development of mAbs against TNF-α, infliximab - the first mAb ever to be therapeutically used in human have been immense37. Much of this and the story of Centocor Laboratories in Malvern, Pennsylvania, and the role of Kapowski at Centocor, has been described above. Michael Wall, the founder of Centocor and its future Director, was well known to Vilček through an earlier collaboration with a small life science company working on IFN-β (old name lymphotoxin). These gentlemen were seeking intellectual support from the academia for developmental plans of their new company. That was the year 1983. Discussions led to the idea of generating different mAbs through scientific collaboration to be exploited by the company commercially (possibly in developing enzyme-linked immunoassay utilizing mAbs). It is of note that Vilček had also mentioned their possible therapeutic use in human37. Thus, came about a convenient financial arrangement where Vilček's Laboratory would produce the monoclonals and Centocor would exploit them commercially and in return, give a grant to Vilček's Laboratory for a postdoctoral position and also pay royalties to NYU. As luck would have it, Junming (Jimmy) Lee an expert in mAb technology joined on a Centocor grant. He produced the first mAb against human IFN-γ in Vilček's Laboratory. By the late 1980s, Centocor wanted to diversify into therapeutic use of mAbs. With the background work of Cerami and colleagues from mid-1980s on the role of TNF in bacterial sepsis, and the combined efforts of Vilček's laboratory and several scientists from Centocor led to the production of a human-mouse chimeric mAb (called cA2) against human TNF in early 1990s. However, it failed to produce any clinically positive effects in patients with septicaemia and, therefore, did not get FDA approval. The work had to be diverted to other mAb development that would be therapeutically useful. In 1993 two scientists from the Kennedy Institute of Rheumatology, London, (RN Maini & M Feldmann) approached Centocor to part with some of their cA2 mAb against human TNF. The rest was again history. Centocor became a billion-dollar company and the work of Maini and Feldmann opened a whole new era of targeted drugs37. Ever since the success of anti-TNF biological therapy, developing drugs without known mechanism (found empirically to be effective, e.g. low-dose methotrexate for the treatment of RA) of action has been abandoned. Targeted therapies are being developed for only those diseases where the cellular-molecular mechanisms of pathogenesis are known.
First use of ‘infliximab’ in clinical medicine - Maini and Feldmann show the way
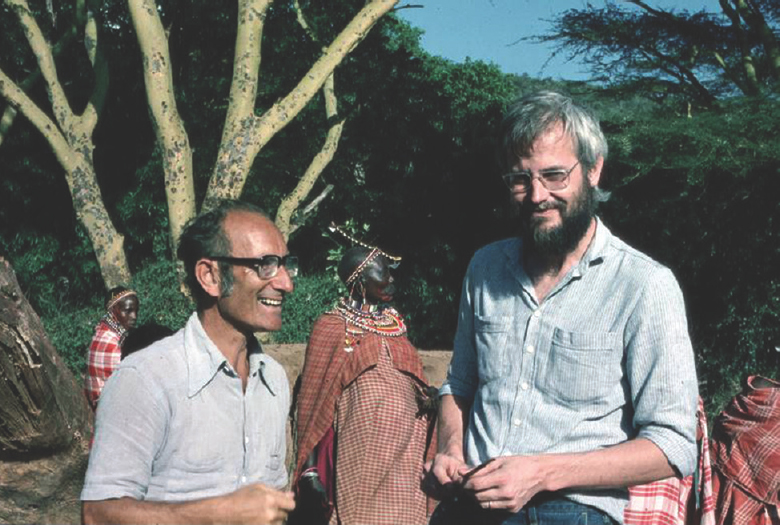
In the late 1960s and early 1970s, Maini et al61 and Feldmann and Basten62 working at the Kennedy Institute of Rheumatology, Imperial College, London, had noted remarkable biological activities in the supernatant of immune cells grown in tissue culture. The technologies of the time were not advanced enough for an in-depth analysis of molecules from these supernatants. By the mid-1970, the technology of cDNA cloning reflecting the mRNA for any naturally produced molecule became available and this simplified the study of cytokines in tissues in health and disease. Maini being a rheumatologist and a keen student of immunology teamed up with Feldmann for an in-depth study of the synovial tissue and of cytokines in RA. Since joint replacement surgeries, occasional biopsies and frequent joint aspirations are routine in a department of Rheumatology; this made their task easier for they could obtain samples of pathological synovial tissues easily. By this time, the synovial tissue culture techniques had already been established since the seminal work of Vabuel5. With some local modifications, it became possible for Buchan et al6364 and Feldmann et al65 to study the role of cytokines generated by cells of the synovium from RA patients by mRNA expression. They observed a spectrum of inflammatory cytokines including TNF, IFN-γ, IL-1, lymphotoxin, IL-6, and granulocyte-macrophage colony-stimulating (GM-CSF) factor in the culture supernatants. Interestingly, the synovial cells had the ability of continuous production of cytokines, which is much in contrast to the transient appearance of most cytokines in a normal physiological process. This phenomenon was termed ‘dysregulation of cytokine production’ (transient physiological vs. continuous pathological production). Unlike previous studies on synovial tissue cytokines (Dayer, 1976 - mentioned in details earlier10), released by FLS, Maini and Feldmann used enzymatically treated synovial cells which could survive for up to a week in culture. This novel technique permitted them to study cytokine dysregulation and overproduction in more details. By this time (late 1980s and early 1990s), several laboratories had generated mAbs against most of the known cytokines. For example, Michael Shepard generated a mAb against TNF at Genentech Laboratories USA, which he generously provided to Maini and Feldmann for their research. Using this neutralizing antibody against TNF, the latter group of investigators observed a most unusual phenomenon, i.e. blocking of TNF inhibited the synthesis of several other important proinflammatory cytokines in cell culture. This led to the pivotal concept that TNF was at the ‘apex’ of a cascade of inflammatory cytokines in the pathogenesis of RA. These findings were published in a seminal paper in 1989 whose first author was Fionnuala Brennan66, a postdoctoral fellow working in the team. The implications of this finding were stunning; targeting a single cytokine leads to complete suppression of the inflammatory cascadein the synovial tissue from RA. Using the hamster anti-mouse-TNF (provided by Bob Schreiber), Richard Williams, a PhD student provided the proof of concept in the mouse that administration of anti-mouse TNF antibody ameliorated collagen-induced arthritis,67. The next obvious step was to initiate clinical trials using anti-human TNF antibodies in RA patients (Fig. 9).

- Sir Ravinder Nath Maini and Sir Marc Feldmann (Courtesy: Sir Marc Feldmann and reproduced with permission from The Lasker Foundation).
Despite scientific evidence of protection with anti-TNF antibodies against endotoxin shock in mice31, Cerami's36 unsuccessful experiments with cattle sleeping sickness in Africa had made most biotech companies wary to provide their anti-human TNF monoclonals for clinical trial in humans. That was the main stumbling block faced by Maini and Feldmann in their quest for testing the efficacy of anti-TNF mAb in RA. Fortunately, Centocor Company in Philadelphia in collaboration with Vilček's group at NYU got interested in producing mAbs for ELISA test kits and for treating human disease. They hired James N. Woody, an ex-student of Maini and Feldmann as the Chief Scientific Officer at the Centocor and this facilitated the availability of anti-human anti-TNF mAbs for a small clinical trial on 10 patients with RA. The trial conducted in May 1992 onwards produced dramatic results. Patients showed marked clinical improvement as well as decrease in inflammation, i.e. the acute phase reactants, which normalized rapidly. This grand success of Centocor's anti-TNF mAb, given the name ‘infliximab’ was publicly announced by Marc Feldmann in September 1992 in a small group meeting organized by David Naor in Arad, Israel, and the results were published68. Several clinical trials followed in quick succession proving high efficacy of infliximab in the treatment of RA69707172. A remarkable aspect of the clinical benefits was that the drug stopped the appearance of new erosions and some of the existing erosions started to heal. Such an effect had never been seen with any previous drug used for treating RA.
Conclusions
While in the past, most scientific discoveries of note were serendipitous, quite often with a ‘Eureka moment’ in the life of a scientist, there has been a major paradigm shift in recent years. For example, a window of the laboratory of Alexander Fleming's in St Mary's Hospital Medical School, Imperial College London, was left open overnight. Next morning, Fleming saw a small clean halo on a bacterial culture plate. At the centre of the halo was Penicillium notatus, a fungus producing penicillin. That is how the antibiotics were discovered, and Fleming was awarded Nobel Prize in 1945 for the discovery (shared with Chain and Walter). Since those early days, there has occurred a major paradigm shift from ‘empirical’ to ‘mechanistic’ approach where the disease mechanism is studied for abnormalities/dysregulations, zeroing in on the most rational target to be hit for normalizing the dysregulation. Over time, step-by-step, one-after-the-other, newer technologies, newer molecular paths in physiology, newer regulatory circuits, newer possibilities of modulating cellular and molecular functions, were discovered. Using this background knowledge and steps involved in the pathological (disease) process, the treatment targets are identified, and drugs targeting those molecules developed. In such a scenario, it becomes difficult to pinpoint a single individual's effort for the development of a drug with profound effects, never seen before. With sound reasoning and proven scientific basis, clinician(s) who use the drug for the first time are often remembered as the discoverer(s) of that drug. The story of the development of infliximab is a typical example of such a drug discovery. Decades of work in different areas of biology, biochemistry and biotechnology carried out by scores of dedicated scientists made it possible to develop a medical-grade mAb against TNF-α. The rheumatologist-immunologist team at the Imperial College, Kennedy Institute, London, led by Mani and Feldmann, would always be remembered, not only for their path-breaking discovery that TNF-α was at the centre of a cascade of inflammatory cytokines in the pathogenesis of RA, but also to be the first to actually use it clinically and demonstrate its high efficacy never seen earlier with any treatment.
The therapeutic success of infliximab opened the door for clinical use of mAbs in medicine and provided a major boost to the Pharma companies for developing additional targeted therapies for a variety of diseases. The public announcement of the high efficacy of infliximab in patients with RA caught the imagination of a large number of biotechnology companies. They could now divert their attention from the disastrous pursuit of infection and septic shock towards diseases where dysregulated cytokine network had been demonstrated such as RA, spondyloarthritis, and other similar systemic immunoinflammatory diseases including inflammatory bowel disease, psoriatic arthritis and juvenile idiopathic arthritis. Without that public announcement, this epoch-making discovery could have gone unnoticed, hidden in the pages of some of the academic journals.
Among the 10 best-selling drugs of 2015, at least six were mAbs73. Most of the present generation of physicians may not be aware that the discoverer of mAb for therapeutic use was a team of rheumatologist-immunologist-clinicians at the Imperial College, Kennedy Institute of Rheumatology, London, headed by Sir Ravinder Nath Maini and his long-time colleague, Sir Marc Feldmann. For his outstanding contribution to science and medicine, Maini has been honoured with several high awards that include the Crafoord Prize (2000), Albert Lasker Award for Clinical Medical Research (2003), Dr Paul Janssen Award for Biomedical Research (2008), Gairdner Foundation International Award (2014), while Prof. Marc Feldmann has been honoured with Crafoord Prize (2000), Albert Lasker Award for Clinical Medical Research (2003), EPO European Inventor of the Year Award (2007), Dr Paul Janssen Award for Biomedical Research (2008), Ernst Schering Prize (2010) and Gairdner Foundation International Award (2014). Finally, for their historic work during 1980s-1990s culminating in the identification of TNFα as a key cytokine in the process of RA, Ravinder Maini and colleague Marc Feldmann were knighted in 2003 and 2010, respectively. We salute this duo for their outstanding contributions leading to mitigation of sufferings of thousands of hapless patients.
Acknowledgment
This review article would not have been possible without the inspiring treatise of Dr Lara Marks, D. Phil (Oxon), FRSB, Managing editor: www.whatisbiotechnology.org; that makes the basis of our paper. The authors acknowledge her help and cooperation in making it possible to write this historical review. The authors would like to express their sincere thanks to Drs Cerami, Dayer, Vilček, Bharat Aggarwal, Thomas Söderqvist, Sir Marc Feldmann and The Lasker Foundation, for providing their photographs for inclusion in this review article. Special thanks are due to Ms Celia Milstein for the photographs of César Milstein and Georges Köhler. This work was inspired by the inquisitiveness of our students and colleagues specially Dr Shubha Bhalla and Dr Shallu Verma, Fellows in rheumatology; Rheumatology Nurse specialists Ms Roopa Rawat, Sadhana Baghel, Ravita Thakaran, Christy Massy, colleague Rheumatologists Drs Sanjiv Kapoor and Shriram Garg; and physiatrists in the department including Dr Qamar Zaheer and Vivekanand. The authors thank them for encouraging to write the review.
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- Emil von Behring: Infectious disease, immunology, serum therapy: Project MUSE, (review) Bull History Med. 2006;80:778-80.
- [Google Scholar]
- Cell culture: History, development and prospects. Int J Curr Res Acad Rev. 2014;2:188-200.
- [Google Scholar]
- Ross Granville Harrison 1870-1959 – A biographical memoir by biographical memoir. Washington D.C.: National Academy of Sciences; 1961.
- [Google Scholar]
- An amended history of tissue culture: Concerning Harrison, Burrows, Mall, and Carrel. J Med Biogr 2016 Jan 01 967772016685033. doi:10.1177/0967772016685033
- [Google Scholar]
- The form and function of synovial cells in tissue cultures: I. Morphology of the cells under varying conditions. J Exp Med. 1933;58:63-83.
- [Google Scholar]
- Cytokine: More than a new word, a new concept proposed by Stanley Cohen thirty years ago. Cytokine. 2004;28:242-7.
- [Google Scholar]
- Commentary. Similarities of T cell function in cell-mediated immunity and antibody production. Cell Immunol. 1974;12:150-9.
- [Google Scholar]
- Peptide signalling in human placenta and membranes: Autocrine, paracrine, and endocrine mechanisms. Endocr Rev. 1996;17:156-86.
- [Google Scholar]
- Studies on the antigenic substance of the bacterial cell. J Exp Med. 1925;42:311-21.
- [Google Scholar]
- From supernatants to cytokines: A personal view on the early history of IL-1, IL-1Ra, TNF and its inhibitor in rheumatology. Arthritis Res Ther. 2018;20:101.
- [Google Scholar]
- Virus interference. I. The interferon. Proc R Soc Lond B Biol Sci. 1957;147:258-67.
- [Google Scholar]
- Sensitization to horse serum by means of adjuvant. Proc Soc Expl Biol Med. 1942;49:548-53.
- [Google Scholar]
- Mechanism of a reaction in vitro associated with delayed-type hypersensitivity. Science. 1966;153:80-2.
- [Google Scholar]
- Delayed hypersensitivity in vitro: Its mediation by cell-free substances formed by lymphoid cell-antigen interaction. Proc Natl Acad Sci U S A. 1966;56:72-7.
- [Google Scholar]
- Lymphocyte in vitro cytotoxicity: Lymphotoxins of several mammalian species. Nature. 1968;219:1076-7.
- [Google Scholar]
- Lymphotoxin and TNF: How it all began-a tribute to the travelers. Cytokine Growth Factor Rev. 2014;25:83-9.
- [Google Scholar]
- Historical perspectives on tumor necrosis factor and its superfamily: 25 years later, a golden journey. Blood. 2012;119:651-65.
- [Google Scholar]
- The definition of lymphocyte activating factor: Giving a helping hand to serendipity. Front Immunol. 2014;5:610.
- [Google Scholar]
- Collagenolytic activity in amphibian tissues: A tissue culture assay. Proc Natl Acad Sci U S A. 1962;48:1014-22.
- [Google Scholar]
- Collagenase production by rheumatoid synovial cells: Stimulation by a human lymphocyte factor. Science. 1977;195:181-3.
- [Google Scholar]
- Prostaglandin production by rheumatoid synovial cells: Stimulation by a factor from human mononuclear cells. J Exp Med. 1977;145:1399-404.
- [Google Scholar]
- Revised nomenclature for antigen nonspecific T cell proliferation and helper factors (letter to the Editor) J Immunol. 1979;123:2928-9.
- [Google Scholar]
- Self-associating IgG rheumatoid factors stimulate monocytes to release prostaglandins and mononuclear cell factor that stimulates collagenase and prostaglandin production by synovial cells. Rheumatol Int. 1983;3:183-6.
- [Google Scholar]
- Collagenase and prostaglandin in connective tissue destruction: Cell-cell and humoral interactions. Bull Schweiz Akad Med Wiss. 1979;35:329-43.
- [Google Scholar]
- Participation of monocyte-macrophages and lymphocytes in the production of a factor that stimulates collagenase and prostaglandin release by rheumatoid synovial cells. J Clin Invest. 1979;64:1386-92.
- [Google Scholar]
- IFN-gamma and 1,25(OH)2D3 induce on THP-1 cells distinct patterns of cell surface antigen expression, cytokine production, and responsiveness to contact with activated T cells. J Immunol. 1992;149:2040-6.
- [Google Scholar]
- A urine inhibitor of interleukin 1 activity that blocks ligand binding. J Immunol. 1987;139:1546-9.
- [Google Scholar]
- Rheumatoid synovial fibroblasts differentiate into distinct subsets in the presence of cytokines and cartilage. Arthritis Res Ther. 2016;18:270.
- [Google Scholar]
- An endotoxin-induced serum factor that causes necrosis of tumors. Proc Natl Acad Sci U S A. 1975;72:3666-70.
- [Google Scholar]
- Passive immunization against cachectin/tumor necrosis factor protects mice from lethal effect of endotoxin. Science. 1985;229:869-71.
- [Google Scholar]
- First demonstration of the role of TNF in the pathogenesis of disease. J Immunol. 2008;181:5-6.
- [Google Scholar]
- Purification of cachectin, a lipoprotein lipase-suppressing hormone secreted by endotoxin-induced RAW 264.7 cells. J Exp Med. 1985;161:984-95.
- [Google Scholar]
- Cachectin/tumor necrosis factor stimulates collagenase and prostaglandin E2 production by human synovial cells and dermal fibroblasts. J Exp Med. 1985;162:2163-8.
- [Google Scholar]
- Identity of tumour necrosis factor and the macrophage-secreted factor cachectin. Nature. 1985;316:552-4.
- [Google Scholar]
- The value of failure: The discovery of TNF and its natural inhibitor erythropoietin. J Intern Med. 2011;269:8-15.
- [Google Scholar]
- An interferon-like substance released from tickborne encephalitis virus-infected chick embryo fibroblast cells. Nature. 1960;187:73-4.
- [Google Scholar]
- Interrelationships of human interferon-gamma with lymphotoxin and monocyte cytotoxin. J Exp Med. 1984;159:828-43.
- [Google Scholar]
- Human tumor necrosis factor. Production, purification, and characterization. J Biol Chem. 1985;260:2345-54.
- [Google Scholar]
- Human lymphotoxin and tumor necrosis factor genes: Structure, homology and chromosomal localization. Nucleic Acids Res. 1985;13:6361-73.
- [Google Scholar]
- Stabilization of interferon messenger RNA activity by treatment of cells with metabolic inhibitors and lowering of the incubation temperature. Proc Natl Acad Sci U S A. 1973;70:3909-13.
- [Google Scholar]
- Tumor necrosis factor: Specific binding and internalization in sensitive and resistant cells. Proc Natl Acad Sci U S A. 1985;82:7626-30.
- [Google Scholar]
- Fibroblast growth enhancing activity of tumor necrosis factor and its relationship to other polypeptide growth factors. J Exp Med. 1986;163:632-43.
- [Google Scholar]
- Tumor necrosis factor and interleukin-1 cause a rapid and transient stimulation of c-fos and c-myc mRNA levels in human fibroblasts. J Biol Chem. 1987;262:11908-11.
- [Google Scholar]
- Isolation and characterization of eight tumor necrosis factor-induced gene sequences from human fibroblasts. Mol Cell Biol. 1990;10:1982-8.
- [Google Scholar]
- A Healthcare Revolution in the Making: The Story of César Milstein and Monoclonal Antibodies. 2013. Available from: http://www.whatisbiotechnology.org/index.php/collections
- [Google Scholar]
- Discovery of the hybridoma principle in 1968-69 immortalization of the specific antibody-producing cell by fusion with a lymphoma cell. J Med. 1985;16:509-24.
- [Google Scholar]
- Selection of a single antibody-forming cell clone and its propagation in syngeneic mice. Proc Natl Acad Sci U S A. 1970;67:1398-403.
- [Google Scholar]
- Antibody with homogeneous antigen binding produced by splenic foci in organ culture. Immunochemistry. 1969;6:757-9.
- [Google Scholar]
- General methods for the study of cells and serum during the immune response: The response to dinitrophenyl in mice. Clin Exp Immunol. 1969;4:473-87.
- [Google Scholar]
- The life-cycle of the antibody-forming cells. I. The generation time of S hemolytic plaque-forming cells during the primary and secondary response. J Exp Med. 1968;128:895-924.
- [Google Scholar]
- 2013. Making monoclonal antibodies The hunt for a single antibody. Available from: http://www.whatisbiotechnology.org/index.php/exhibitions/milstein/monoclonals/The-making-ofmonoclonal-antibodies
- César Milstein and investigations into the generation of antibody diversity. Panorama Inmunol. 2003;22:306-12.
- [Google Scholar]
- Continuous cultures of fused cells secreting antibody of predefined specificity. Nature. 1975;256:495-7.
- [Google Scholar]
- Specific collaboration between T and B lymphocytes across a cell impermeable membrane in vitro. Nat New Biol. 1972;237:13-5.
- [Google Scholar]
- Detection of activated T cell products in the rheumatoid joint using cDNA probes to interleukin-2 (IL-2) IL-2 receptor and IFN-gamma. Clin Exp Immunol. 1988;71:295-301.
- [Google Scholar]
- Interleukin-1 and tumour necrosis factor mRNA expression in rheumatoid arthritis: Prolonged production of IL-1 alpha. Clin Exp Immunol. 1988;73:449-55.
- [Google Scholar]
- Inhibitory effect of TNF alpha antibodies on synovial cell interleukin-1 production in rheumatoid arthritis. Lancet. 1989;2:244-7.
- [Google Scholar]
- Expression of granulocyte-macrophage colony-stimulating factor in rheumatoid arthritis: Regulation by tumor necrosis factor-alpha. Eur J Immunol. 1991;21:2575-9.
- [Google Scholar]
- Treatment of rheumatoid arthritis with chimeric monoclonal antibodies to tumor necrosis factor alpha. Arthritis Rheum. 1993;36:1681-90.
- [Google Scholar]
- Repeated therapy with monoclonal antibody to tumour necrosis factor alpha (cA2) in patients with rheumatoid arthritis. Lancet. 1994;344:1125-7.
- [Google Scholar]
- Randomised double-blind comparison of chimeric monoclonal antibody to tumour necrosis factor alpha (cA2) versus placebo in rheumatoid arthritis. Lancet. 1994;344:1105-10.
- [Google Scholar]
- Therapeutic efficacy of multiple intravenous infusions of anti-tumor necrosis factor alpha monoclonal antibody combined with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis Rheum. 1998;41:1552-63.
- [Google Scholar]
- Infliximab and methotrexate in the treatment of rheumatoid arthritis. Anti-tumor necrosis factor trial in rheumatoid arthritis with concomitant therapy study group. N Engl J Med. 2000;343:1594-602.
- [Google Scholar]






