Translate this page into:
Oral health consequences of smokeless tobacco use
For correspondence: Dr Saman Warnakulasuriya, WHO Collaborating Centre for Oral Cancer & King's College London, London, UK e-mail: s.warne@kcl.ac.uk
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Smokeless tobacco (SLT) use has many oral effects including oral cancer, leukoplakia and erythroplakia, oral submucous fibrosis (if mixed with areca nut), loss of periodontal support (recession) and staining of teeth and composite restorations. This review was aimed to provide information to identify oral lesions that occur due to the use of smokeless tobacco so that effective interventions can be undertaken to reduce morbidity and mortality from the use of SLT.
Keywords
Chewing tobacco
leukoplakia
oral cancer
smokeless tobacco
submucous fibrosis
Introduction
Tobacco is derived from two main species Nicotiana tabacum and Nicotiana rustica. The most important ingredient from the leaves of these plants is nicotine - a volatile alkaloid. Nicotine is one of the most addictive and stimulant drugs. Nicotine affects all organs, but predominantly, it binds to a central nervous system receptor and increases brain dopamine levels making it an addictive agent. Although nicotine is an addictive, most of the severe health effects of smokeless tobacco use come from other chemicals1. The Centers for Disease Control and Prevention analyzed 40 top-selling brands of moist snuff to measure nicotine, moisture, pH, un-ionized nicotine and tobacco-specific nitrosamines (TSNAs), including 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol. The study findings indicated that moist snuff brands in the US varied widely in the content of rapidly absorbed, addictive un-ionized nicotine (500-fold range) and of carcinogenic TSNAs (18-fold range)2. Smokeless tobacco (SLT) products in the Indian market are likely to have much more nitrosamine content. This was confirmed in a study on the Indian products: the highest levels of TSNAs were found in certain brands of khaini, zarda and other SLT products. Concentrations of N-nitrosonornicotine (NNN) and 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) in these products ranged from 1.74-76.9 to 0.08-28.4 μg/g, respectively3. The packaging, moisture content and pH of the product influence the content and rapid absorption of chemicals through the oral mucosa. Smokeless tobacco may also contain harmful metals such as arsenic. A recent study indicates that the concentration of arsenic was significantly higher in scalp hair and blood samples of tobacco chewing patients than those of controls4.
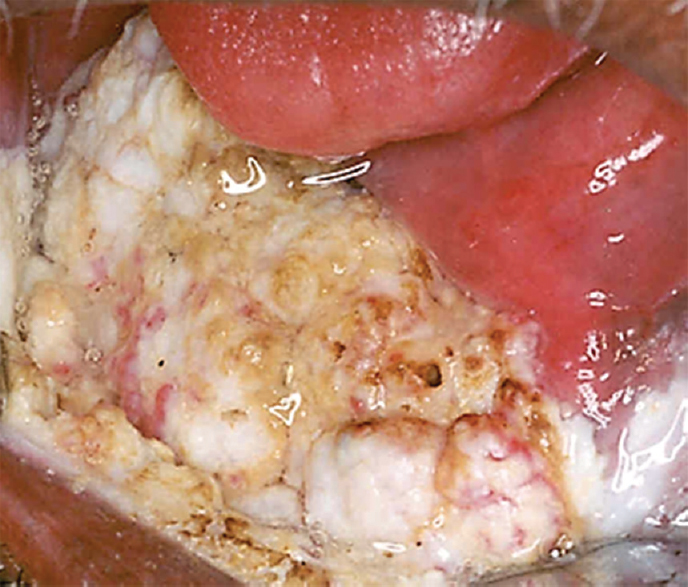
In addition to chewing tobacco leaves, other forms of smokeless tobacco are used in India and other countries. The terminology used for these SLT products and the ingredients in tobacco mixtures used to make these products are shown in Table. Gutka is the most abundantly consumed SLT form in India. Gutka has now been banned all over India5, but a more vigorous implementation is necessary. Betel quid used in South Asia often contains smokeless tobacco6.
There is greater prevalence of using smokeless tobacco than smoking tobacco in the Indian subcontinent. Use differs by age, gender and social class. Unlike other regions, in South East Asia Region, SLT use among adults is higher than smoking. Among women tobacco users, SLT is the predominant form of tobacco used6.
Chewing tobacco and other smokeless tobacco products are known to be deleterious to oral health. The oral health effects of smokeless tobacco used in North America has been reviewed earlier7. This review is focused on harmful effects of SLT products available in the Indian subcontinent. The effects can be divided into two broad categories: those affecting the dental hard tissues, which include teeth, their supporting periodontium, and the soft tissues, which make up the oral mucosa that lines the oral cavity.
Oral health consequences of SLT use
The main categories of smokeless or chewing tobacco-induced oral mucosal soft-tissue lesions reported are: oral squamous cell carcinoma (SCC) and verrucous carcinoma; oral potentially malignant disorders (OPMDs) (leukoplakia, erythroplakia and erythroleukoplakia); and tobacco pouch lesion [tobacco and lime users’ lesion, oral submucous fibrosis (OSF) when mixed with areca nut].
Oral cancer
The evaluation of carcinogenic risks of smokeless tobacco by the International Agency on Research for Cancer (IARC) has confirmed that SLT is carcinogenic to human and the main target organ being the oral cavity where the products are applied locally89. The IARC evaluation is based on a large number of epidemiological studies (both case-control and cohort studies) and various experimental studies both in vivo and in vitro. A meta-analysis of published studies10 reported an adjusted relative risk of 6.19 [confidence interval (CI) 4.16-9.21] from 10 studies for chewing betel quid with tobacco. The population attributable risk of SLT for the development of oral cancer is estimated at 66 per cent to tobacco chewers10. Cancers of the oral cavity arise in the lining epithelium of the oral cavity and the two main histological types reported are SCCs and verrucous carcinomas.
Squamous cell carcinoma
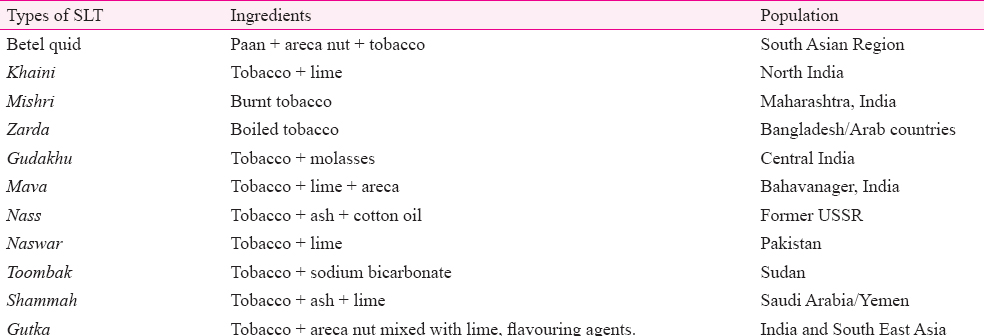
Tumours appear as red granular areas, or tend to be exophytic- ulcerative-infiltrative (Fig. 1). Ulcerative lesions have a distinct rolled border (margins). Induration at the margins and base of the tumour is a pathognomonic sign of oral SCC. Buccal involvement is reported to be as high as 80 per cent of the cancers that arise at the site of placement of the tobacco-containing quid, mostly in the lower buccal sulcus or posterior buccal mucosa. Lateral margins of tongue and floor of mouth are also high-risk sites due to pooling to tobacco fluid in this horse-shaped area in the mouth. In late stages, limitation of mouth opening, rigidity of tongue and metastasis to lymph nodes are common. Buccal carcinoma with extraoral fungation is not uncommon.

- Oral squamous cell carcinoma in a patient addicted to gutka. Tumour arising from retromolar region has spread to the buccal sulcus. The figure demonstrates features of an exophytic growth with ulceration and necrosis.
Verrucous carcinoma
Verrucous carcinoma (VC) comprised up to 16 per cent of oral cancers in an Indian study11 with a predilection for commissural, buccal or gingival sites. VC is a slow-growing tumour spreading laterally, is more indolent than conventional SCC. It is a diffuse, exophytic lesion usually covered by leukoplakic (keratotic) patches (Fig. 2). Characteristically, the lesion shows multiple rugae-like folds and deep clefts between them. This tumour has a high potential for local recurrence but not for nodal metastasis12. VC could sometimes appear as multifocal tumours due to field cancerization of the oral cavity by chronic SLT use.
- Verrucous carcinoma in oral cavity of a patient in a tobacco chewer. This is an advanced tumour with a typical verrucoid appearance.
Oral potentially malignant disorders (OPMD)
Placing tobacco in the oral cavity, namely in the buccal mucosa, gingival sulcus, inner aspect of lower lip, floor of the mouth initially leads to keratotic or hyperkeratotic changes. These changes are localized to the site where tobacco is placed (Fig. 3). Initially, there is a greyish white area which develops at the site of tobacco placement with a wrinkling of the mucosa which is termed as ‘tobacco pouch keratosis’13. Pindborg14 reported some morphological variations in smokeless tobacco-associated lesions in the form of discrete elevated keratinized striae, particularly when involving non-keratinized mucosal sites. These striae gave the appearance to the lesion described as ‘pumice pattern’. A typically wrinkled appearance at the site of placement of the moist snuff and chewing tobacco was described by Axéll et al15. Later with prolonged use this area of mucosa changes to more defined conditions referred to as leukoplakia or erythroplakia.

- Lower labial sulcus of a patient showing tobacco pouch keratosis in places where the quid has been retained for long periods.
Leukoplakia and erythroplakia
Leukoplakias are usually diagnosed after the fourth decade of life. These are more common in males and are six times more common among SLT users, than among non-tobacco users16. Sites of involvement among SLT users are buccal mucosa and lower buccal groves that are commonly affected due to the placement of tobacco quid at these locations.
There are two main clinical types of leukoplakia encountered in clinical practice; homogeneous and non-homogeneous leukoplakia16. The distinction is based on surface colour and morphological (thickness and texture) characteristics. Homogeneous leukoplakiasare uniformly flat and thin (Fig. 4). Non-homogeneous varieties comprise three clinical types: (i) Speckled: mixed, white and red (also termed erythroleukoplakia) (Fig. 5) but retaining predominantly white in colour; (ii) Nodular: small polypoid outgrowths, rounded red or white excrescences; and (iii) Verrucous or exophytic: wrinkled or corrugated surface appearance.

- Oral homogeneous leukoplakia affecting the commisure in a tobacco chewer.

- Erythroleukoplakia with candidal infection. This is mixed red and white lesion and has a worse prognosis than homogeneous leukoplakia.
In general, most leukoplakias are asymptomatic. A red component in the leukoplakia (erythroleukoplakia) indicates possible colonization by candida organisms and an increased risk for dysplasia and/or malignancy (Fig. 5). When widespread or multiple patches of leukoplakia are noted the term proliferative verrucous leukoplakia is used (Fig. 6). This is a distinct entity that carries a higher risk for malignant transformation and is fortunately rare. A provisional diagnosis of leukoplakia is made after excluding other conditions that clinically appear white in colour17.

- Proliferative verrucous leukoplakia. Thick white plaques are noted affecting several sites, gingiva, alveolar mucosa, the sulcus and spreading to lower lip.
Erythroplakia clinically appears as a red patch with a velvety or a granular surface and present with well circumscribed clinical margins. Again the diagnosis is made after excluding other conditions that clinically appear red in colour.
Oral submucous fibrosis
OSF is a chronic, insidious disease that affects the submucosa of the oral cavity resulting in progressive limitation of mouth opening which is a hallmark feature of this disease18. The disease is solely69 caused by areca nut and the literature erroneously refers to smokeless tobacco as the causative agent. However, as gutka products contain both SLT and areca nut19, the disease is common among gutka chewers. Due to an increase in the prevalence of gutka use among young people in India, the OSF was considered as an epidemic20. A systematic review21 of studies reported ORs 2.98 (CI 1.5-3.9); 2.33 (CI 1.9-4.5); 5.08 (CI 3.7-6.4); 3.56 (CI 1.3-4.7); 33 (CI 2.2-46.6); 1.65 (CI 1.2-2.3); 3.33 (CI 2.5-5.3) and 9.25 (CI 3.1-15.5) for between gutka use and prevalence of OSF. Fig. 7 illustrates some of the clinical aspects of OSF. Malignant changes at the site of OPMD may take a couple of years to manifest. Before oral SCC develops, a biopsy taken from the white or red patch may show varying degrees of dysplasia. Some OPMDs may show reversal and may not undergo malignant change22.
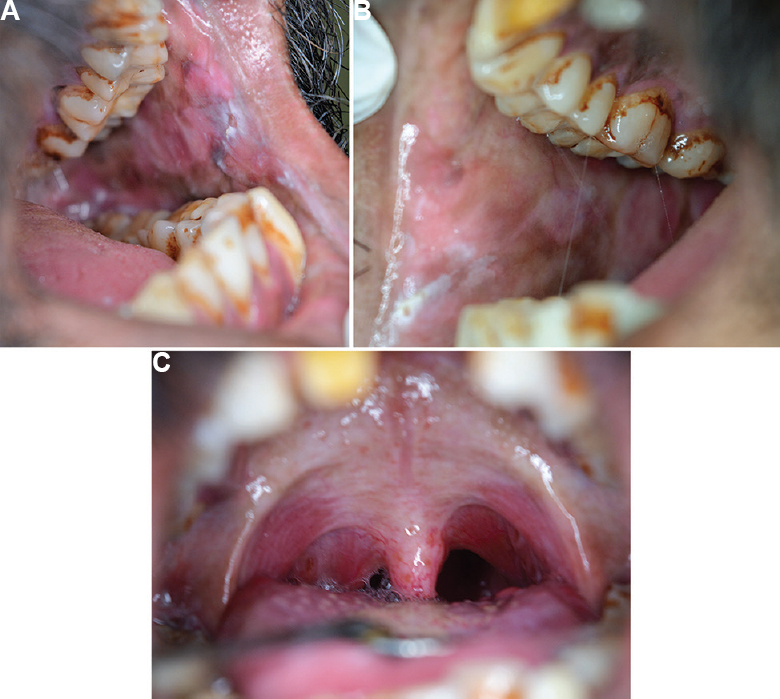
- Oral submucous fibrosis, (A) left buccal mucosa, (B) right buccal mucosa, (C) palate. The buccal mucosae show loss of elasticity and fibrous banding. The palatal arch shows fibrosis.
Effect of smokeless tobacco on teeth
Chewing tobacco and use of SLT products cause considerable staining of teeth among users (Fig. 8). Discolouration of the teeth is a common complication of tobacco chewing. The stains bind and penetrate the enamel, dentin, root surfaces causing a brown to black discolouration. Artificial dentures, prosthesis are also discoloured by prolonged tobacco chewing. The coarse abrasives in tobacco products when constantly chewed cause abrasion or tooth wear. Chewing tobacco also increases the incidence of dental caries and thereby causes tooth loss23. Epidemiology suggests tobacco users have 67 per cent tooth loss compared to non-users23. The high content of sweetening and flavouring agents in tobacco products is responsible for tooth decay.

- Tooth staining. These extrinsic stains are due to long term betel quid with tobacco use.
Effects of SLT on gingiva and periodontal tissues
Among smokeless tobacco users, there is an increased gingival recession with exposure of tooth root surface, periodontal pocket formation, plaque and calculus accumulation which leads to periodontitis. The gingival recession is more prominent in the anterior teeth region. A systematic review21 of three studies among tobacco chewers reported ORs 1.64 (CI 1.2-2.1); 2.20 (CI 1.1-4.9) and 3.56 (CI 1.9-5.50) for periodontal inflammation including gingivitis, gingival recession and periodontal pocketing among tobacco chewers.
Conclusion
Smokeless tobacco predisposes to increased risk of oral cancer and OPMD development in an individual. In addition, it exerts a number of adverse effects on the teeth and adjoining structures. All healthcare providers should assess the patients’ tobacco usage habits and actively employ tobacco prevention, cessation and treatment programmes.
Conflicts of Interest: None.
Financial support & sponsorship: None.
References
- National Cancer Institute and Centers for Disease Control and Prevention. Smokeless Tobacco and Public Health: A Global Perspective. NIH Publication No. 14-7983 2014
- [Google Scholar]
- Surveillance of moist snuff: Total nicotine, moisture, pH, un-ionized nicotine, and tobacco-specific nitrosamines. Nicotine Tob Res. 2008;10:1645-52.
- [Google Scholar]
- Tobacco-specific nitrosamines in smokeless tobacco products marketed in India. Int J Cancer. 2005;116:16-9.
- [Google Scholar]
- Correlation of arsenic levels in smokeless tobacco products and biological samples of oral cancer patients and control consumers. Biol Trace Elem Res. 2015;168:287-95.
- [Google Scholar]
- Resource Centre for Tobacco Free India. Available from: www.rctfi.org/, accessed on May 2, 2013
- International Agency for Research on Cancer. IARC monographs on the evaluation of carcinogenic risks to humans. In: Betel-quid and areca nut chewing and some areca-nut derived nitrosamines. Vol 85. Lyon, France: IARC; 2004.
- [Google Scholar]
- International Agency for Research on Cancer. IARC monographs on the evaluation of carcinogenic risks to humans. In: Smokeless tobacco and some tobacco specific N-nitrosamines. Vol 89. Lyon, France: IARC; 2007.
- [Google Scholar]
- International Agency for Research on Cancer. IARC monographs on the evaluation of carcinogenic risks to humans. In: Personal habits and indoor combustions. Vol 100E. Lyon, France: IARC; 2012.
- [Google Scholar]
- Betel quid chewing and the risk of oral and oropharyngeal cancers: a meta-analysis with implications for cancer control. Int J Cancer. 2014;135:1433-43.
- [Google Scholar]
- Verrucous carcinoma of the oral cavity: A clinico-pathologic appraisal of 133 cases in Indians. Oral Maxillofac Surg. 2010;14:211-8.
- [Google Scholar]
- Verrucous carcinoma of the oral cavity: A clinical and pathological study of 101 cases. Oral Oncol. 2009;45:47-51.
- [Google Scholar]
- Oral mucosal lesions associated with tobacco and betel-chewing habits: A napalese experience. Dent J Malays. 1997;18:23-5.
- [Google Scholar]
- Oral cancer and precancer. Bristol: John Wright; 1980.
- Oral mucosal findings associated with chewing tobacco in Sweden - A clinical and histological study. J Dent Assoc S Afr. 1992;47:194-6.
- [Google Scholar]
- Definition of leukoplakia and related lesions: An aid to studies on oral precancer. Oral Surg Oral Med Oral Pathol. 1978;46:518-39.
- [Google Scholar]
- Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med. 2007;36:575-80.
- [Google Scholar]
- Oral submucous fibrosis: A review of the current management and possible directions for novel therapies. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122:232-41.
- [Google Scholar]
- Oral mucosal disorders associated with habitual gutka usage: A review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:857-64.
- [Google Scholar]
- Malignant transformation of oral leukoplakia: a systematic review of observational studies. J Oral Pathol Med. 2016;45:155-66.
- [Google Scholar]
- Oral health risks of tobacco use and effects of cessation. Int Dent J. 2010;60:7-30.
- [Google Scholar]






