Translate this page into:
Cytopenia in adult brucellosis patients
For correspondence: Dr Safak Kaya, Department of Infectious Diseases & Clinical Microbiology, Gazi Yasargil Training & Research Hospital, Diyarbakir 21100, Turkey e-mail: ksafak76@gmail.com
-
Received: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Brucellosis can lead to haematological abnormalities including cytopenia confusing with haematological malignancies. The aim of this study was to compare the main characteristics of brucellosis patients without cytopenia (Group 1) and with cytopenia (Group 2).
Methods:
This five-year period study which was performed in two referral hospitals in Turkey, included all adult brucellosis patients. Abnormally, low counts of leucocyte or haemoglobin or platelets in a patient were considered as cytopenia. The demographics, clinical, laboratory, treatment and outcome data were analyzed.
Results:
A total of 484 brucellosis patients were enrolled. Among the cases, 162 (33.5%) of them had cytopenia. One hundred and four (21.5%) had anaemia, 88 (18.8%) had thrombocytopenia, 71 (14.6%) had leucopenia and 28 (5.8%) had pancytopenia. The mean age of group 2 was 35.01±16.05 yr and it was 33.31±14.39 yr in group 1. While there was no difference between the groups in terms of duration of treatment, the median length of hospital stay (LOS) was significantly longer in group 2 (9 vs 10 days; P <0.001). The most frequently applied combination therapy consisted of doxycycline plus rifampicin and doxycycline plus streptomycin regimens. No significant difference was observed in terms of duration of treatment, LOS and restoration time of cytopenia between the patients who received either of these combinations.
Interpretation & conclusions:
Our findings suggested that the patients with cytopenia should be investigated for brucellosis, especially if living in, or with a history of travel to, endemic areas, in view of the increase in world travel.
Keywords
Anaemia
brucellosis
leucopenia
pancytopenia
thrombocytopenia
Brucellosis is a zoonotic disease frequently seen throughout the world. It is especially common in the Mediterranean region, the Middle East, the Arabian Peninsula, Central and South America, Asia and Africa. Although it has been brought under control in the majority of developed countries, it is still an important health problem in developing countries, including Turkey123. Vaccination of animals plays an important role in the control of the disease. Transmission to humans is known to occur through the ingestion of contaminated meat and dairy products, infected animal tissue, direct contact of blood or bodily fluids with broken skin or conjunctiva and inhalation of infectious aerosols. Since the disease may involve a number of organs and systems in the body, it manifests with various symptoms. There are no disease-specific clinical, haematological or biochemical characteristics that help distinguish the condition from other infectious diseases. Therefore, its diagnosis may present a challenge4.
Brucellosis leads to a number of non-specific haematological abnormalities. Although mild-to-moderate anaemia and leucopenia are frequently observed, it may also rarely present with pancytopenia, severe thrombocytopenia or severe leucopenia. Therefore, the condition may sometimes be confused with haematological malignancies5. The aims of this study were to evaluate the epidemiological, clinical and laboratory features of brucellosis in patients with cytopenia and the complications associated with the disease, and to compare the antibiotic combinations used, duration of treatment, normalization time of cytopenia, length of hospital stay (LOS) and cure or relapse in brucellosis patients.
Material & Methods
The South-eastern Anatolian region of Turkey is an endemic area for brucellosis3. One of the largest cities is Diyarbakir, and both the Gazi Yasargil Training and Research Hospital and the Dicle University Hospital are referral hospitals for the region. This study included all patients admitted to these two centres in Diyarbakir Province, Turkey, for brucellosis-associated cytopenia between 2009 and 2013. Only patients over the age of 14 yr with brucellosis were enrolled. Patients both with and without cytopenia were enrolled in the study, into separate groups. A standard questionnaire was administered to the participant centres, and data were collected through a digital database. A control group consisting of brucellosis patients without cytopenia was formed among the brucellosis patients concurrently diagnosed or treated at the participating centres. Dicle University Hospital's Review Board in Diyarbakir, Turkey, approved the study. All participants gave prior written informed consent.
The diagnosis of brucellosis was based on positive agglutination titres (1:160 or higher) in the standard tube agglutination (STA) test and/or isolation of brucellae from blood or sterile body fluids in patients with signs and symptoms consistent with brucellosis. When the STA was negative, the test was repeated with Coombs serum to detect anti-Brucella-blocking antibodies (>1:160 in one serum sample or fourfold increase in two separate samples taken at least two weeks apart)4. Cases fulfilling the above-mentioned criteria were included, and cases having cytopenia of infectious aetiology other than brucellosis or non-infectious aetiology were excluded. According to the duration of symptoms, brucellosis was classified as acute (less than eight weeks), sub-acute (8-52 wk) and chronic (>52 wk). Blood haemoglobin values <12 g/dl for females and <13 g/dl for males, leucocyte count <4×109/l and platelet count <150×109/l were considered as anaemia, leucopenia and thrombocytopenia, respectively. Abnormally, low leucocyte and platelet counts and haemoglobin level together is accepted as pancytopenia6. Patients with more than five times the upper limit of normal for aminotransferases were placed in clinical hepatitis category. Reappearance of symptoms within six months of discontinuation of antibiotic treatment was considered as relapse.
For microbiological and serological analyses, the blood samples were inoculated into BacT/ALERT FA plus aerobic bottles (bioMérieux, France) and were analyzed in the BacT/ALERT 3D (bioMérieux, France) automated blood culture system. The other clinical samples including the cerebrospinal fluid, synovial fluid, abscess discharges and other bodily fluids were inoculated onto sheep blood agar and chocolate agar. Brucella abortus strain 99 was used for the agglutination test, which was produced in Pendik Animal Diseases Research Institute (Istanbul, Turkey). The Rose Bengal test (RBT; slide agglutination method), STA and Coombs agglutination test were used for the serological analyses4.
All patients were evaluated on admission, daily during their hospitalization and six months after discharge, by the same physicians at the participating centres. For each patient, complete blood count, routine biochemistry parameters, serum C-reactive protein (CRP) levels (nephelometric method) and erythrocyte sedimentation rate (ESR) were measured at admission, and these were repeated when needed. In addition, double sets of blood cultures were drawn for each patient on admission. Response to treatment was monitored using clinical and laboratory data. Antibiotic combinations were continued until the resolution of all foci of brucellosis. Antibiotic treatment was modified if therapeutic failure or adverse drug effects were observed.
The following data were collected from the participating centres and entered into a digital database for each patient: (i) Demographic and epidemiological data: age and gender; (ii) Clinical and laboratory data: duration of disease, symptoms and signs, comorbid conditions, foci of brucellosis, routine and microbiological and serological diagnostic test results for brucellosis, restoration time of the cytopenia to the normal range in the cytopenic group; (iii) Treatment data: drug combinations used, duration of treatment for each drug combination; and (iv) Outcome data: recovery, relapse or death (if any) and LOS in hospital.
All the patients diagnosed as brucellosis were enrolled for the study and were classified into two groups: those without cytopenia (Group 1) and those with cytopenia (Group 2).
Statistical analysis: Statistical analysis was performed using the SPSS for Windows v.16.5 (SPSS Inc., Chicago, IL, USA) software package. Descriptive statistics were presented as frequency and percentage for categorical variables or as mean±standard deviation (SD) and median [interquartile range (IQR)] for continuous variables according to the results of normality tests, as appropriate. Normality testing was done by the one-sample Kolmogorov–Smirnov test. For group comparisons, the Chi-square and Fisher's exact tests were used to compare the categorical variables, and numerical data were analyzed using Student's t test for the parametric data and the Mann–Whitney U-test for the variables of the non-parametric data.
Results
A total of 484 consecutive brucellosis patients over a period of five years were enrolled in the study. Among these patients, 233 (48.1%) were male and 251 (51.9%) were female (Table I). Their mean age±SD was 33.88±14.96 yr (data not shown), and 16.7 per cent patients were over the age of 50 yr. Among the patients, 162 (33.5%) were cytopenic and 70 (43.2%) of these were male while 92 (56.8%) were female Table I. The mean age of cytopenic patients was 35.01±16.05 yr and 33.31±14.39 yr in patients without cytopenia (data not shown). No significant difference was observed in terms of gender between cytopenic and non-cytopenic patients groups (Table I). Of the 484 patients, 285 (60.9%) were identified as having the acute form, 105 (21.7%) the sub-acute form and 84 (17.4%) the chronic form of the disease. No significant difference was found regarding the number of patients with acute brucellosis between the groups.
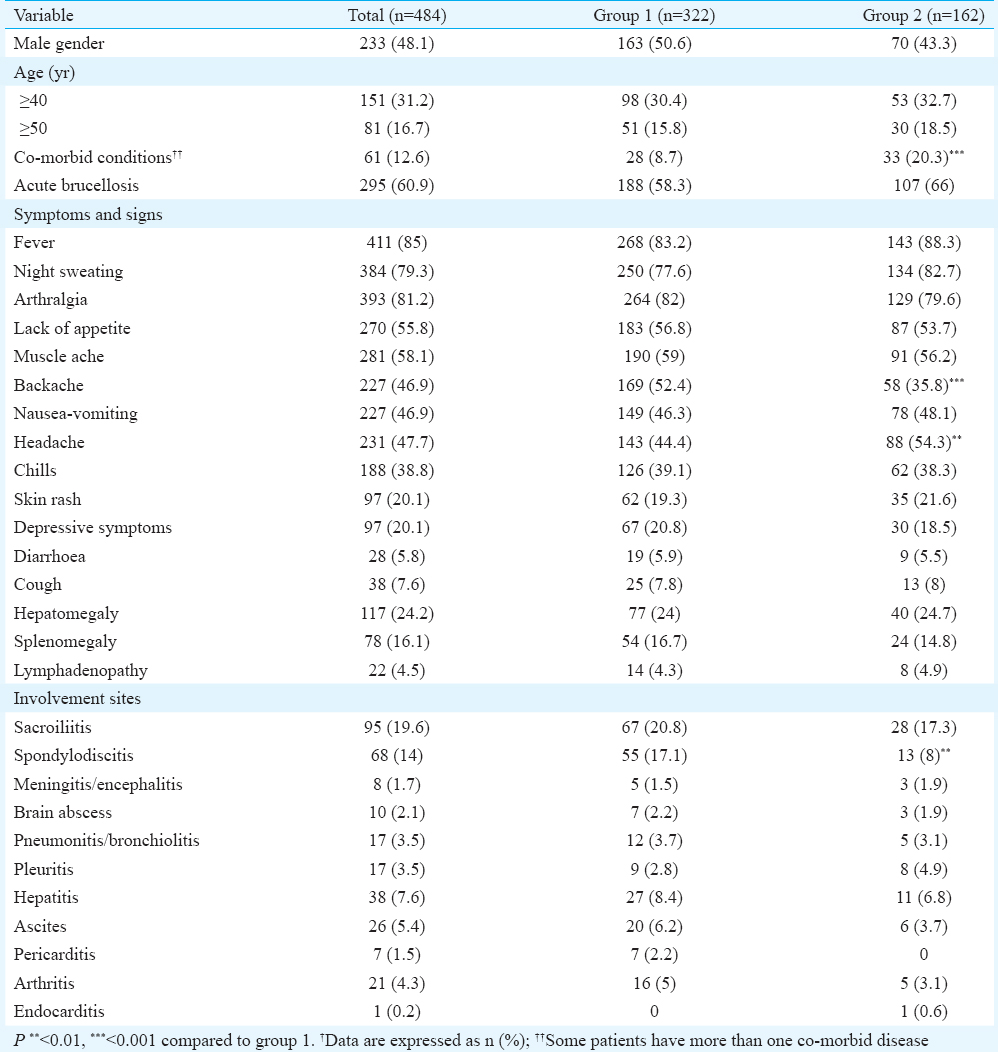
A total of 61 (12.6%) of the 484 patients had at least one co-morbid condition, namely diabetes mellitus in 15 patients (3.1%), hypertension in five patients (1.03%), coronary artery disease in five patients (1.03%), congestive heart failure in one patient (0.2%), solid organ tumours in three patients (0.61%) and hypercholesterolaemia in one patient (0.2%). When the groups were compared in terms of the presence of at least one comorbidity, the cytopenic patient group outnumbered the other (33 vs 28; P<0.001).
For the clinical findings among the patients (n=484), 411 (85%) had fever, 393 (81.2%) had arthralgia and 384 (79.3%) had night sweats. All the symptoms and findings are presented in Table I. When the groups were compared, headache was found to be more frequent in the cytopenic group (P<0.01), while backache was more common in the non-cytopenic group (P<0.001). Sacroiliitis (n=95; 19.6%) and spondylodiscitis (n=68; 14%) were the most frequently involved sites among the patients. While there was no significant difference regarding sacroiliitis between the groups, spondylodiscitis was significantly more frequent in the non-cytopenic group in association with backache (P<0.01).
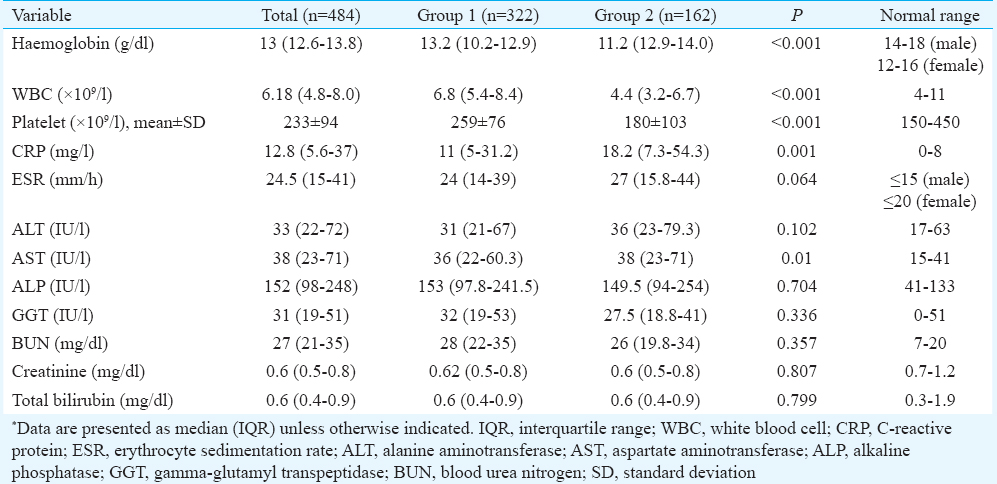
Of the entire patients, 104 (21.5%) had anaemia, 88 (18.8%) had thrombocytopenia, 71 (14.6%) had leucopenia, 31 (6.4%) had leucopenia and thrombocytopenia, seven (1.4%) had anaemia and leucopenia, seven (1.4%) had anaemia and thrombocytopenia and 28 (5.8%) had pancytopenia (data not shown). In terms of the haematological parameters in the cytopenic group, the median (IQR) haemoglobin level was 11.2 (12.9-14.0) g/dl, the median leucocyte count was 4.4 (3.2-6.7)×109/l and the mean platelet count was 180±103×109/l. The groups were found to differ significantly for these parameters (P<0.001 for all comparisons). Furthermore, the differences in terms of the blood CRP and aspartate aminotransferase (AST) values were significant between the groups (P =0.001 and P =0.01, respectively) Table II. Blood cultures yielded positive results in 111 patients (23%). Of the 111 isolates, 109 (98.2%) were Brucella melitensis and two (1.8%) were B. abortus. The RBT result was positive in 419 (86.5%) and the STA was positive in 482 (99.4%) patients. There were no significant differences in terms of frequency of positive blood culture for brucellae or positivity of RBT and STA tests between the groups (Table III).
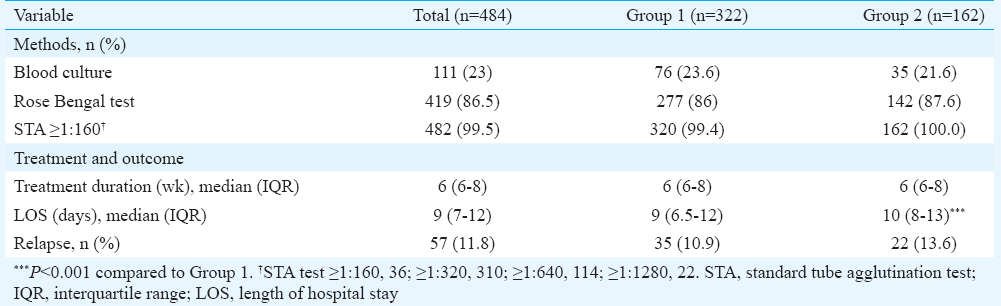
The median duration of medical treatment in all patients was six weeks (6-8 wk) (maximum 24 wk), and the median LOS was nine days (7-12 days) (maximum 38 days). While there was no difference between the groups in terms of the duration of treatment, the LOS was significantly longer in the cytopenic group (9 vs 10 days; P<0.001; Table III). In the cytopenic group, median restoration time of cytopenia was 14.0 (9.0-18.5) days (data not shown) and the two most frequently administered combination therapy regimens were doxycycline plus rifampicin and doxycycline plus streptomycin. However, no significant difference was observed in terms of LOS, duration of treatment and the reversal of cytopenia to normal levels, between the patients who received either of these combinations (Table IV). Relapses were observed in 57 (11.8%) patients and the difference between the cytopenic and non-cytopenic groups was not significant. All of the relapsed patients responded to a second course of therapy. No death was observed in this study.

Discussion
Brucellosis is an infectious disease that may manifest with various acute or chronic symptoms following an incubation period, which varies from 1 to 3 wk to a few months. Its prevalence among children is also high, and the disease is especially common in areas endemic to B. melitensis where children and animals share the same living spaces7. In two studies from Kuwait and Iran, more than 80 per cent of the patients were found to be below the age of 40 yr89. In our study, 68.8 per cent out of the 484 patients were below the age of 40 yr and the ratios between the cytopenic and non-cytopenic groups were similar. Most studies conducted in endemic regions demonstrated that males were more frequently affected by the disease, suggesting a relationship between the disease and occupation10111213. In our study, 51.9 per cent of the patients were females. The reason for this could be that females are more frequently occupied with animal husbandry than males.
Brucellosis presents as either acute or chronic infection. In this study, the acute form was more frequent (60.9%), and the symptoms during this phase, such as fever, were helpful in establishing an early diagnosis1415. The results of this study showed that the clinical stage was not important for occurrence of cytopenia in brucellosis. A study from Turkey showed frequent anaemia and leucopenia but less frequent pancytopenia and thrombocytopenia, in patients with acute brucellosis16. Other reports from our country suggest more frequent fever, hepatomegaly, splenomegaly and epididymo-orchitis (in male patients) in the acute form and more frequent spondylitis in the chronic form of brucellosis1417. Fever and arthralgia are the most frequently observed symptoms in patients with brucellosis, followed by sweating, anorexia, headache and backache1819. In our study, fever and arthralgia were the most common symptoms. In general, the symptoms were similar in both groups. However, headache was more common in the cytopenic group, while backache was significantly more frequent in the non-cytopenic group. Lymphadenopathy was observed in 10-20 per cent of patients, while hepatomegaly and/or splenomegaly were observed in 20-30 per cent20. In our patients, the frequencies of hepatomegaly, splenomegaly and lymphadenopathy were 24.2, 16.1 and 4.5 per cent, respectively. Complications in brucellosis are important both with reference to the selection of antibiotics and the duration of treatment. Osteoarticular complications are the most common complications of brucellosis, and their prevalence was found to range between 10 and 80 per cent in various studies212223. Sacroiliitis and spondylodiscitis of the lumbar vertebrae are frequently observed2122. Sacroiliitis and spondylodiscitis were the most frequently observed complications in our patients.
Mild anaemia, leucopenia and thrombocytopenia are frequently observed haematological complications in brucellosis. In addition, pancytopenia may rarely occur. The exact causes of cytopenia in brucellosis are not well defined. Hypersplenism, haemophagocytosis, hypoplasia and granulomatous lesions of the bone marrow and immune destruction seem to be the possible causes of these anomalies in the peripheral blood2324. Higher levels of interleukin (IL)-6, IL-8, interferon (IF)-gamma and tumour necrosis factor (TNF)-alpha in acute brucellosis patients suggest the presence of significant inflammation2526. In this study, high CRP levels were found in cytopenic brucellosis patients. High CRP levels may be related to production of high levels of IL-6 secondary to Brucella infection or the existence of more co-morbid conditions in cytopenic patients. High CRP levels may show that brucellosis proceeds more severely in the cytopenic group. CRP is a biomarker of inflammation, and it is an important mechanistic link between inflammation and thrombosis in the host27.
Bone marrow examination of brucellosis patients with haematological involvement has revealed hypercellularity, non-caseified granulomas, and haemophagocytosis28. Brucellae also have a directly suppressive effect on bone marrow, which may lead to a reduction in the production of erythropoietin. In the majority of brucellosis patients, the haematological findings are normal29. Therefore, in patients with anaemia, leucopenia and/or thrombocytopenia, brucellosis may be overlooked. In a study conducted in Turkey, 43 per cent of the patients had anaemia, 14 per cent had thrombocytopenia, 12 per cent had leucopenia, seven per cent had leucopenia and anaemia, five per cent had pancytopenia, six per cent had anaemia and thrombocytopenia and four per cent had leucopenia and thrombocytopenia16. In our study also, 21.5 per cent of the 484 patients had anaemia, 18.8 per cent had thrombocytopenia, 14.6 per cent had leucopenia, 5.8 per cent had pancytopenia, 6.4 per cent had leucopenia and thrombocytopenia, 1.4 per cent had anaemia and leucopenia and 1.4 per cent had anaemia and thrombocytopenia.
Blood culture, the gold standard for laboratory diagnosis of brucellosis, was positive in 111 (23%) of 484 patients. Positive blood cultures occur in 10-70 per cent of suspected infections, depending on the duration, localization of the infection, the type of Brucella species and the culture techniques used. It is more often positive during the acute phase71529. Moreover, automated culture systems are much more often positive than conventional cultures for sterile body fluids30. In this study, more patients (60.9%) being in the acute phase and the use of an automated culture system may both have affected the blood culture results. However, they are in agreement with the current literature15. We detected that 482 (99.5%) patients had positive STA test, with 446 (92.1%) of them having STA test titres ≥1:320, which was consistent with the expectation in endemic areas due to frequent contact with brucellosis infection. Turkey is an endemic area for brucellosis, and in a previous study from our region of Turkey (district of Van), the STA test was found to be positive in 99 per cent (779/787) of brucellosis patients16. The test was also reported positive in 86.2 per cent of Iranian brucellosis cases12.
The treatment of brucellosis is difficult due to the side effects of the antibiotics, relapses and development of resistance. The World Health Organization recommended regimen is doxycycline plus rifampin for six weeks for the treatment of adult brucellosis. However, the regimen of doxycycline for six weeks plus streptomycin for 2-3 wk is reported to be the most effective therapy430. In patients with serious localization, a triple antibiotherapy should be administered and the duration of treatment should be extended31. Although the relapse rate in cytopenic patients was found to be slightly higher than that of the non-cytopenic group, the groups were not different for relapse rates. Relapse rates for brucellosis are reported between 5 and 15 per cent depending on drug combinations30. In our study, doxycycline plus rifampicin and doxycycline plus streptomycin were the two most common treatment options in the cytopenic patients group. Both median treatment duration (six weeks) and median LOS (10 days) were found to be the same for both combinations of drug regimens. Other treatment regimens showed similar results for treatment duration and LOS. In addition, in cytopenic patients with brucellosis, the median LOS was significantly longer compared to patients without cytopenia. Significant additional co-morbid conditions may have contributed to longer LOS in this group of patients and this will also be reflected in the treatment costs. Although data on the hospitalization period for brucellosis patients are limited, the LOS was reported to range between 7 and 14 days in Iranian brucellosis patients5. Dilek et al16 showed that the thrombocytopenia and leucopenia returned to the normal range within one week, while anaemia took 3-4 wk. In another study, the normalization time for the cytopenia was observed to be 2-6 wk32. In our study, it was 14 days, and the longest duration (35 days) was observed in a patient treated with the doxycycline plus rifampicin plus streptomycin therapy regimen.
In conclusion, our study showed that the epidemiological, clinical and treatment features and relapse rates of adult brucellosis patients with cytopenia and those without cytopenia were similar. Further, both time span until normalization of the cytopenia was 14 days and the LOS was longer in cytopenic patients than the non-cytopenic patients. It is recommended that patients with cytopenia should be investigated for brucellosis, especially if living in, or with a history of travel to, endemic areas, in view of the increase in world travel.
Financial support & sponsorship: None
Conflicts of Interest: None.
References
- Risk factors for brucellosis - Leylek and Kadamjay districts, Batken Oblast, Kyrgyzstan, January-November, 2003. MMWR Suppl. 2006;55:31-4.
- [Google Scholar]
- Brucellar pericarditis: A report of four cases and review of the literature. Int J Infect Dis. 2013;17:e428-32.
- [Google Scholar]
- Mandell GL, Bennet JE, Dolin R, eds. Principles and Practice of Infectious Diseases (6th ed). Philadelphia: Elsevier Churchill Livingstone; 2005. p. :2669-74.
- Brucellosis in children: Clinical observations in 115 cases. Int J Infect Dis. 2002;6:182-6.
- [Google Scholar]
- Human brucellosis: Epidemiological situation in Chile, 2001-2010. Rev Chilena Infectol. 2013;30:653-9.
- [Google Scholar]
- Trends of human brucellosis in Italy, 1998-2010. Epidemiol Infect. 2014;142:1188-95.
- [Google Scholar]
- Epidemiological, laboratory, diagnostic and public health aspects of human brucellosis in Western Iran. Asian Pac J Trop Biomed. 2013;3:589-94.
- [Google Scholar]
- Brucellosis in Guangdong province, people's republic of China, 2005-2010. Emerg Infect Dis. 2013;19:817-8.
- [Google Scholar]
- Clinical appearance of brucellosis in adults: Fourteen years of experience. Turk J Med Sci. 2012;42:497-505.
- [Google Scholar]
- Manual of Clinical Microbiology. Washington, DC: ASM Press; 1995. p. :549-55.
- Hematological complications in 787 cases of acute brucellosis in Eastern Turkey. Turk J Med Sci. 2008;38:421-4.
- [Google Scholar]
- Clinical manifestations and complications in 1028 cases of brucellosis: A retrospective evaluation and review of the literature. Int J Infect Dis. 2010;14:e469-78.
- [Google Scholar]
- The changing pattern of human brucellosis: Clinical manifestations, epidemiology, and treatment outcomes over three decades in Georgia. BMC Infect Dis. 2010;10:346.
- [Google Scholar]
- Natural history of brucellosis in an endemic region in different time periods. Acta Clin Croat. 2009;48:41-6.
- [Google Scholar]
- Complications associated with Brucella melitensis infection: A study of 530 cases. Medicine (Baltimore). 1996;75:195-211.
- [Google Scholar]
- Brucellar sacroiliitis: Findings in 63 episodes and current relevance. Clin Infect Dis. 1993;16:761-5.
- [Google Scholar]
- Brucellar spondylitis: Review of 35 cases and literature survey. Clin Infect Dis. 1999;29:1440-9.
- [Google Scholar]
- Pancytopenia, a rare hematologic manifestation of brucellosis in children. J Pediatr Hematol Oncol. 2004;26:803-6.
- [Google Scholar]
- TNF-α signalling and inflammation: Interactions between old acquaintances. Inflamm Res. 2013;62:641-51.
- [Google Scholar]
- Cytokine profile and nitric oxide levels in sera from patients with brucellosis. Braz J Med Biol Res. 2004;37:1659-63.
- [Google Scholar]
- Linking inflammation and thrombosis: Role of C-reactive protein. World J Cardiol. 2010;2:365-9.
- [Google Scholar]
- Pancytopenia in children with brucellosis: Clinical manifestations and bone marrow findings. Acta Haematol. 1993;89:132-6.
- [Google Scholar]
- Clinical manifestations, complications and treatment of brucellosis: An evaluation of 480 patients. Med Mal Infect. 2002;32:485-93.
- [Google Scholar]
- Mandell, Douglass, and Bennett's Principles and Practice of Infectious Diseases. (8th ed). Philadelphia: Elsevier Co; 2015. p. :2584-9.
- [Google Scholar]
- Madkour's Brucellosis 2001:1-14.
- An analysis of children with brucellosis associated with pancytopenia. Pediatr Hematol Oncol. 2011;28:203-8.
- [Google Scholar]






