Translate this page into:
Impact of embryo co-culture with cumulus cells on pregnancy & implantation rate in patients undergoing in vitro fertilization using donor oocyte
Reprint requests: Dr Jagdish S. Patel, Department of Biochemistry, P.D. Patel Institute of Applied Sciences, Charotar University of Science & Technology, Changa, Petlad, Anand 388 421, Gujarat, India e-mail: jspbiochem@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Cumulus cell co-culture of embryo had been found to be beneficial for achieving better pregnancy and implantation rate (IR). The present study was aimed to evaluate efficiency of cumulus co-culture technique over simple culture of embryo in terms of pregnancy rate (PR) and IR in patients undergoing treatment for infertility using donor oocytes fertilized by intracytoplasmic sperm injection.
Methods:
This was a quasi-experimental study between control and study groups. The primary endpoint was achievement of pregnancy. Control group included 508 women who underwent embryo development without cumulus cell co-culture and study group included 394 women who underwent embryo development with cumulus cell co-culture using donor's cumulus cells.
Results:
The present study demonstrated a significant increase in the IR (37.2 vs 24.2%, P<0.001) and in PR (45.7 vs 37.8%, P<0.05) in study group than in control group. The PR and IR were found to be higher in study group, among all groups of women, grouped on the basis of different indications for use of donor oocytes.
Interpretation & conclusions:
Cumulus cell co-culture technique was found to be more effective than simple culture technique for embryo development in women undergoing treatment for infertility using donor oocytes fertilized by intracytoplasmic sperm injection.
Keywords
Cumulus cell co-culture
donor oocytes
intracytoplasmic sperm injection
in vitro fertilization
premature ovarian failure
After successful live birth using donor oocyte in 19841, demand for donated oocytes has increased across the globe, as many infertile couples willing to use this as common treatment option to overcome their infertility2. Women facing any of problems such as gonadal dysgenesis, premature ovarian failure, iatrogenic ovarian failure due to ovarian surgery or radiation or chemical castration, who have resistant ovary syndrome, who are poor responders to ovulation induction, who are carriers of recessive autosomal disorders, who have attained menopause, generally go for in vitro fertilization (IVF) using donor oocytes3.
Beneficial role of co-culturing human embryos with different helper cells/feeder cells have been proven in many studies in the past45678. Different helper cells such as those of fallopian tube, endometrium or cumulus cells have been used extensively for co-culture techniques to study their beneficial effect on the development of greater quality embryo, implantation rate (IR) and pregnancy rate (PR)8. Feeder cells remove toxin from culture medium and add certain growth factors such as insulin-like growth factors (IGF) I and IGF-II, vascular endothelial growth factor, transforming growth factor (TGF)-α and TGF-β, platelet activating factor and epidermal growth factor to morphologically sound embryos9. Feeder cells also metabolize glucose present in the medium, allowing the embryos to be exposed to bearable levels of glucose10. Co-culture of embryos provides better synchrony between the embryonic stage and site of placement of transfer (uterus) and by favouring growth up to blastocyst, it also increases availability of more cells for biopsy from blastomere for genotypic evaluations1112.
Oocytes quality is one of the crucial factors for successful fertilization and implantation. The present study was undertaken to evaluate the effect of cumulus cell co-culture technique in terms of PR and IR in patient undergoing IVF of donor oocytes by intracytoplasmic sperm injection (IVF/ICSI). The quality of oocytes was maintained by choosing donor who fulfilled criteria for egg donor as per the guidelines3. Furthermore, quality of each oocyte was assured by observing morphological characteristics. There are extensive data, signifying benefits of cumulus cell co-culture of embryos and cumulus aided co-transfer of embryo using self-egg during IVF7813.
Material & Methods
This quasi experimental study was undertaken at Akanksha IVF Clinic, Anand, Gujarat, from January 2012 to August 2015 (Control group: January 2012 to December 2013, Study Group: January 2014 to August 2015). Control group comprised 508 women, who had undergone IVF/ICSI treatment using donor oocytes and embryo developed by simple technique without cumulus cell co-culture while the study group comprised 394 women who underwent IVF/ICSI treatment using donor oocytes and embryos were cultured with cumulus cells of donor oocytes (Fig. 1).
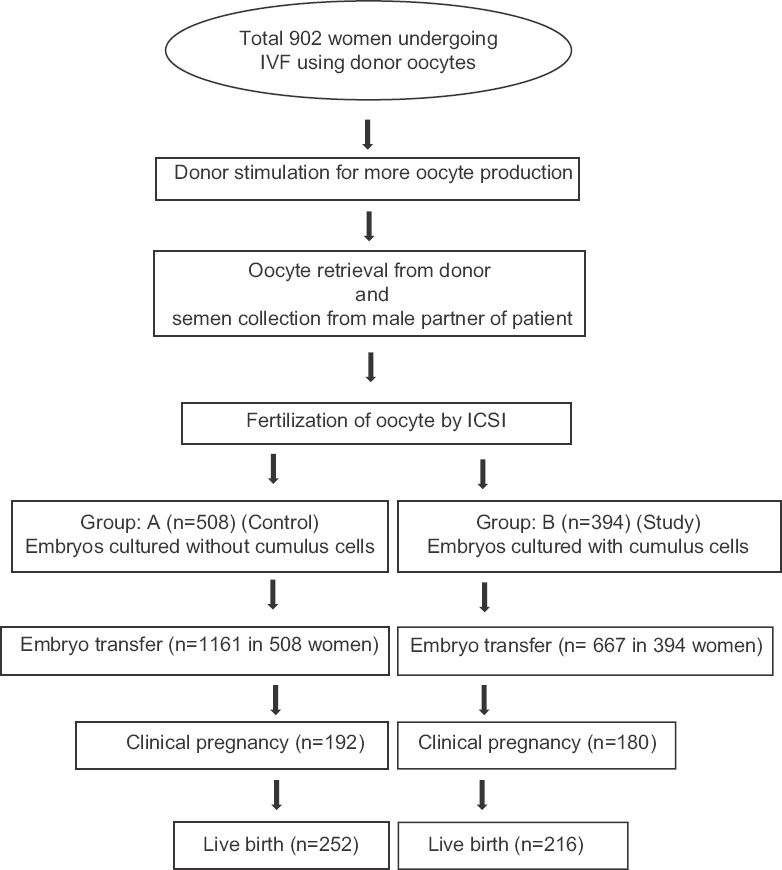
- Flowchart of the study population. IVF, in vitro fertilization; ICSI, intra cytoplasmic sperm injection.
Criteria for egg donor: Donors were screened from medical and psychological perspective, and for family history of birth defects or hereditary diseases by taking a comprehensive family history. Donors were healthy women in the age group of 21-35 yr, were not pregnant or premenopausal. At time of oocytes retrieval, none was using hormone contraceptive or any oestrogen or progestin therapy. The blood group of each donor was noted; the donors were also tested for human immunodeficiency virus (HIV), hepatitis B virus surface antigen (HBsAg), hepatitis C virus (HCV) and syphilis.
Criteria for semen: The semen characteristics of the intended father were determined to see if they were in conformity with those associated with normal fertility as per WHO guideline for semen analysis14. Recipients included in this study were women with bad egg quality due to various causes but were healthy women (determined by medical and psychological examination) having normal genitalia (as determined by physical examination) and uterine cavity (as determined by hysteron salpingography). Abnormality related to uterus and/or those whose husband had abnormal semen analysis were excluded from this study to exclude impact of sperm parameters on pregnancy outcome.
Procedure for ovarian hyperstimulation and collection of oocytes: Oocytes were harvested from donors for IVF/ICSI after standard ovarian stimulation with human chorionic gonadotropin (HCG) trigger at follicular maturity under transvaginal ultrasound.
Sperm preparation: Patients were evaluated for semen quality14. Semen samples were processed by swim-up method at 37°C, 1:2 ratio of semen sample and sperm washing medium (Flushing medium, Origio, Denmark).
Culture system: In control group, to prepare oocyte for ICSI, oocytes were denuded by exposure to 80 IU of hyaluronidase after two hours of retrieval from donor. After ICSI, injected oocytes were incubated per droplet at 37°C in triple gas incubator with 6 per cent CO2. On day three, embryos were transferred with fresh preincubated Continuous Single Culture medium (Irvine Scientific, Santa Ana, USA).
In study group, cumulus cells were mechanically removed from each oocyte with 26G tuberculin syringe, washed with Continuous Single Culture medium (Irvine Scientific) and plated in different droplets of 50 μl in Falcon 3002 dish (Falcon®, NC, USA). Oocytes were prepared for ICSI by standard protocol15 and were denuded by exposure to 80 IU of hyaluronidase after two hours of oocyte retrieval. Injected oocytes were plated and incubated on monolayer of cumulus cells, single oocyte was kept per droplet at 37°C in triple gas incubator with 6 per cent CO2. On day three, embryos were transferred with fresh preincubated medium (Fig. 2).
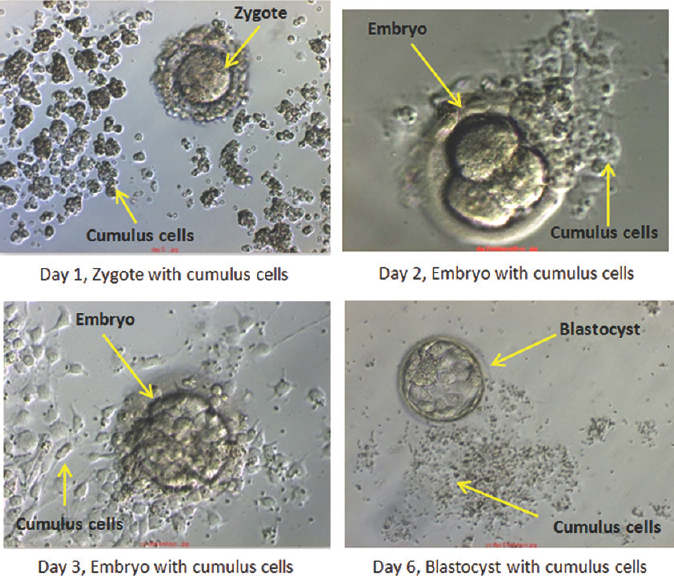
- Developing embryos with cumulus cells.
Pregnancy: Pregnancy was detected by measuring serum HCG at least 15 days after embryo replacement in uterus. Clinical pregnancy was determined by observation of a gestational sac with foetal heart beat by transvaginal ultrasound at six weeks of pregnancy. The clinical embryo IR was defined as the number of gestational sacs observed at echographic screening at six weeks of pregnancy divided by the number of embryos transferred.
The study was approved by the Institutional Review Board. Informed written consent was taken from each patient.
Statistical analysis: The PR, in individual group, was determined by proportion of pregnant women after the intervention. The IR was determined by percentage of successful implants out of total embryo transferred. Descriptive statistics [mean±standard deviation (SD), frequency (%)] were used to depict the profile of study population. Chi-square test was used to determine the similarity between the groups at baseline. Independent t test was used to compare the IR between groups whereas Chi-square test was employed to compare the PRs. A multivariable logistic regression was applied to determine unconfounded effect of group status adjusting for effect of age and indication. The analysis was performed using STATA (14.2) (StataCorp LLC, Texas, USA).
Results
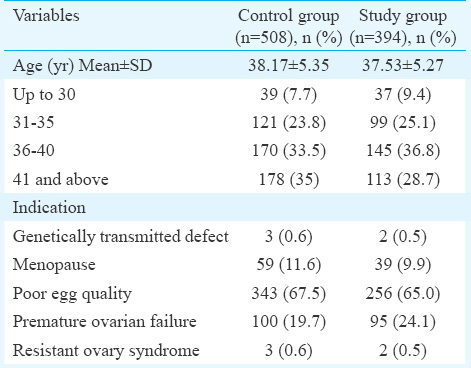
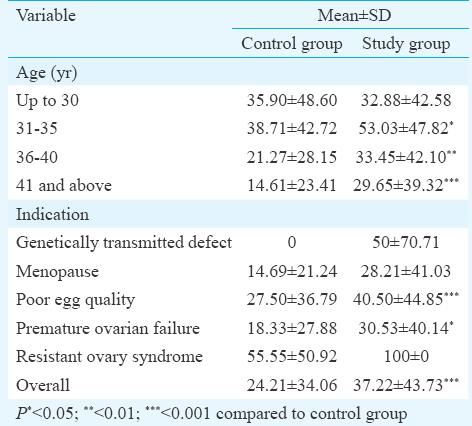
A total of 902 women were enrolled in the study [508 control condition (without cumulus cell co-culture) and 394 study condition]. The mean (SD) age of the study participants was 37.89 (5.33) (range: 23-50) yr. Most of the study participants were above age 35. Poor egg quality (66.4%) and premature ovarian failure (21.6%) were most common indications for seeking infertility treatment. The baseline characteristics of the control and study groups were similar with respect to age as well as indication (Table I).
The overall PR was significantly higher in study group as compared to control group [180 (45.7%) vs 192 (37.8%), P=0.01]. This was prominent in the age group 41 and above and those suffering from poor egg quality (P<0.05) (Table II).
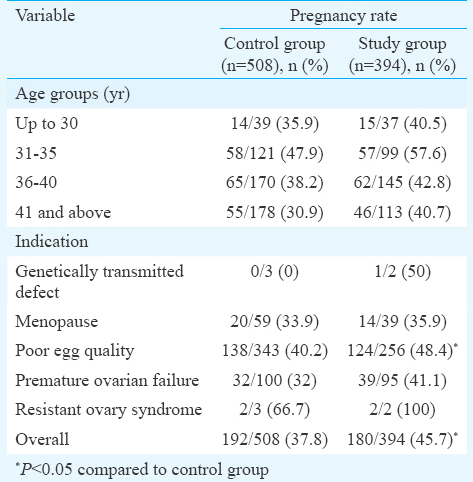
The mean IR was significantly higher in study group as compared to control group (37.22±43.73 vs 24.21±34.06, P<0.001]. This difference was prominent in all age groups above age 30 and in all indications (Table III).
A multivariable logistic regression analysis revealed that even after adjusting for age (P=0.021) and indication (P=0.16), the group status had significant impact with odds of achieving pregnancy was significantly higher in study group as compared to control group (odds ratio=1.39, 95% confidence interval: 1.06-1.82, P=0.017).
Discussion
Role of mammalian cumulus cells during oocyte growth and maturation has been proven. Cumulus cells are known to nurture the oocyte while it is in the ovarian follicle during ovulation phase. It is speculated that the close association between the cumulus cells and the oocyte is maintained through transzonal cumulus cell projections and intercumulus projections16.
In the present study, significant increase in pregnancy and IRs was found in women in whom cumulus cell co-culture technique was used for culturing the embryos, which was in concordance with a study by Parikh et al17, who performed cumulus aided embryo transfer along with cumulus cell co-culture. Such higher rates of pregnancy were achieved due to the fact that development of superior quality embryos occured16, in the presence of cumulus cells which nurtured the embryos during in vitro development and increased the number of embryos that reached the 4-cell and 8-cell stages with regular blastomeres6, compared to the embryos developed by simple technique.
In the present study, as donor's oocytes were used for IVF, age of recipient mother was not considered for implantation of embryos and achievement of pregnancy. However, the IR and PR were evaluated in different age groups of recipient mothers. The PR was found to be higher in age groups of 31-40 yr than age group of up to 30 yr among control and study groups. In the study group, PR of age group 41 and above was found to be similar with youngest age group. Likewise, in both groups, higher IR was found in age group of 31-35 yr than that of 30 yr and below. These results indicated that when donor eggs were used for IVF, implantation and PR was not affected by higher age of recipient mother.
Results of the present study indicated that greater quality of embryos were achieved by culturing the embryos with cumulus cells, which were more competent to implant and to achieve pregnancy. This finding differed from results of Cihangir et al18 who did not observe an increase in implantation and clinical PR using cumulus cell co-culture and cumulus aided embryo transfer.
Inclusion of patient with normal sperm parameters and performance of ICSI as standard protocol for fertilization of oocyte could be a limitations of this study. In both groups, the quality of oocyte and sperm were constant, as the study was carried out using donor oocytes fertilized by ICSI with sperm from semen with normal parameters; further randomized control trials or a series of careful observational studies are required to verify the efficiency of cumulus cell co-culture technique for embryo development using simple IVF technique which can reduce cost of the procedure and also with abnormal sperm parameters along with self-eggs.
In conclusion, the results of our study demonstrated beneficial role of cumulus cells co-culture technique in embryonic development in women undergoing IVF using donor oocytes fertilized by ICSI. This study showed that a simple, low-cost and non-laborious cumulus cell co-culture system could result in improved IRs and clinical PRs during IVF.
Acknowledgment
The authors thank Ms Urvi Patel and Ms Madhuri Visawadiya of Akanksha Hospital and Research Institute, Anand, India for their technical help.
Conflicts of Interest: None.
References
- The establishment and maintenance of pregnancy using in vitro fertilization and embryo donation in a patient with primary ovarian failure. Nature. 1984;307:174-5.
- [Google Scholar]
- Indian Council of Medical Research - Ministry of Health and Family Welfare, India. The Assisted Reproductive Technologies (Regulation) Rule - 2010. Available from: http://www.icmr.nic.in/guide/ART%20REGULATION%20Draft%20Rules%201.pdf
- [Google Scholar]
- Improved pregnancy rate after transfer of embryos grown in human fallopian tubal cell coculture. Fertil Steril. 1992;58:569-74.
- [Google Scholar]
- Coculture of embryos on homologous endometrial cells in patients with repeated failures of implantation. Fertil Steril. 1995;63:109-14.
- [Google Scholar]
- Co-culture of human pronucleate oocytes with their cumulus cells. Hum Reprod. 1994;9:1727-9.
- [Google Scholar]
- Beneficial effects of coculture with cumulus cells on blastocyst formation in a prospective trial with supernumerary human embryos. J Assist Reprod Genet. 1996;13:9-14.
- [Google Scholar]
- Cumulus coculture and cumulus-aided embryo transfer increases pregnancy rates in patients undergoing in vitro fertilization. Fertil Steril. 2006;86:839-47.
- [Google Scholar]
- Assessment of growth factor effects on post-thaw development of cryopreserved mouse morulae to the blastocyst stage. Hum Reprod. 2000;15:410-8.
- [Google Scholar]
- Culture of preimplantation embryos: Facts and artifacts. Hum Reprod Update. 1995;1:91-148.
- [Google Scholar]
- Use of coculture with cumulus cells in insemination medium in human in vitro fertilization (IVF) J Assist Reprod Genet. 1994;11:270-7.
- [Google Scholar]
- Polymerase chain reaction analysis of the cystic fibrosis delta F508 mutation in human blastomeres following oocyte injection of a single sperm from a carrier. Prenat Diagn. 1993;13:873-80.
- [Google Scholar]
- A simplified coculture system using homologous, attached cumulus tissue results in improved human embryo morphology and pregnancy rates during in vitro fertilization. J Assist Reprod Genet. 1999;16:344-9.
- [Google Scholar]
- World Health Organization. WHO laboratory manual for the examination and processing of human semen. (5th ed). Geneva: WHO; 2010.
- [Google Scholar]
- Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992;340:17-8.
- [Google Scholar]
- Dynamic changes of cumulus-oocyte cell communication during in vitro maturation of porcine oocytes. Biol Reprod. 2000;63:723-9.
- [Google Scholar]
- A novel way of enhancing pregnancy rates in ART cycles-cumulus co-culture and cumulus aided embryo transfer. Obstet Gynecol India. 2004;54:571-4.
- [Google Scholar]
- Influence of cumulus cell coculture and cumulusaided embryo transfer on embryonic development and pregnancy rates. J Turk Ger Gynecol Assoc. 2010;11:121-6.
- [Google Scholar]






