Translate this page into:
Aetiology, outcomes & predictors of mortality in acute respiratory distress syndrome from a tertiary care centre in north India
Reprint requests: Dr Surendra K. Sharma, Department of Medicine, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110 029, India e-mail: sksharma.aiims@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Acute respiratory distress syndrome (ARDS) is a common disorder in critically ill patients and is associated with high mortality. There is a paucity of literature on this condition from developing countries. This prospective observational study was designed to find out the aetiology, outcomes and predictors of mortality in ARDS.
Methods:
Sixty four consecutive patients who satisfied American-European Consensus Conference (AECC) definition of ARDS from medical Intensive Care Unit (ICU) of a tertiary care centre in New Delhi, India, were enrolled in the study. Demographic, biochemical and ventilatory variables were recorded for each patient. Baseline measurements of serum interleukin (IL)-1β, IL-6, tumour necrosis factor-alpha (TNF-α), procalcitonin (PCT) and high sensitivity C-reactive protein (hsCRP) were performed.
Results:
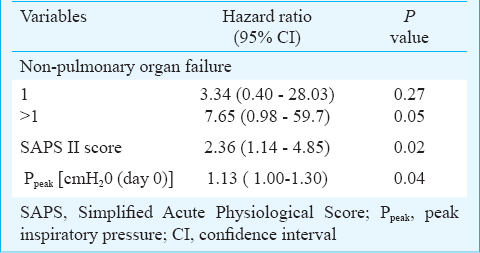
Common causes of ARDS included pneumonia [44/64 (68.7%)], malaria [9/64 (14.1%)] and sepsis [8/64 (12.5%]. Eight of the 64 (12.5%) patients had ARDS due to viral pneumonia. The 28-day mortality was 36/64 (56.2%). Independent predictors of mortality included non-pulmonary organ failure, [Hazard ratio (HR) 7.65; 95% CI 0.98-59.7, P=0.05], Simplified Acute Physiology Score (SAPS-II) [HR 2.36; 95% CI 1.14-4.85, P=0.02] and peak pressure (Ppeak) [HR 1.13; 95% CI 1.00-1.30, P = 0.04] at admission.
Interpretation & conclusions:
Bacterial and viral pneumonia, malaria and tuberculosis resulted in ARDS in a considerable number of patients. Independent predictors of mortality included non-pulmonary organ failure, SAPS II score and Ppeak at baseline. Elevated levels of biomarkers such as TNF-α, PCT and hsCRP at admission might help in identifying patients at a higher risk of mortality.
Keywords
ARDS
CRP
pneumonia
procalcitonin
tuberculosis
viruses
Acute respiratory distress syndrome (ARDS) was initially defined by Ashbaugh et al1 in 1967 as a condition characterized by rapid onset tachypnoea and hypoxaemia with loss of lung compliance and bilateral infiltrates on chest radiograph. Despite several limitations which were, highlighted in the new Berlin criteria2, the American-European Consensus Conference (AECC) criteria3 are still widely used for the diagnosis of ARDS. The reported mortality of ARDS is approximately 36-44 per cent4. As reported in a systematic review4, ARDS mortality has remained almost unchanged despite the availability of new ventilatory modes, use of low-tidal volume ventilation strategy5 and other therapeutic improvements in critically ill patients in the last decade.
Though it has been recognized that ARDS aetiology can affect prognosis/management, only a few studies on ARDS have been published from developing countries6789. Chronic liver disease, non-pulmonary organ dysfunction, sepsis, and older age have been identified to predict the risk of death in ARDS910. There is a paucity of systematically conducted prospective studies on ARDS from resource-limited countries. The present investigation was designed to prospectively study the aetiology, outcomes and predictors of mortality in ARDS from a tertiary care hospital in north India.
Material & Methods
This was a prospective observational study conducted in the Intensive Care Unit (ICU) of department of Medicine at the All India Institute of Medical Sciences (AIIMS) hospital, New Delhi, India, between July 2010 to June 2012. This hospital is a tertiary care centre located in north India serving middle to lower socio-economic status patients from several adjacent States. Consecutive patients who fulfilled the AECC3 criteria for ARDS, acute onset; arterial hypoxaemia with ratio of arterial oxygen tension over fractional inspired oxygen (PaO2/FiO2) lower than 200 (regardless of positive end-expiratory pressure level); bilateral infiltrates seen on chest radiograph; pulmonary artery wedge pressure lower than 18 mmHg or no clinical evidence of left atrial hypertension, were enrolled. Patients with pre-existing lung diseases, transferred from any other hospital, positive serology for human immunodeficiency virus (HIV) or age less than 15 yr were excluded. Patients with sequelae due to past history of pulmonary tuberculosis were also excluded from the study, however, newly diagnosed patients of tuberculosis with ARDS were included in the study. A written informed consent was obtained from patients and the study protocol was approved by the institutional ethics committee.
Study design: Patients were mechanically ventilated as per the ARDS Network protocol11. Recorded data included demographic characteristics (age and sex), pre-existing diseases, co-morbidities, risk factors for ARDS, number of organ failures, use of corticosteroids and neuromuscular blockers, biochemical variables, requirement of renal replacement therapy (RRT), ventilatory parameters, outcome, length of ICU and hospital stay. An attempt was made to establish the aetiology of ARDS in each case. Pneumonia was defined from the radiographic presence of new infiltrates, along with the identification of at least one pathogen in a sputum specimen or bronchoalveolar lavage (BAL) fluid culture and clinical evidence of infection.
Patients who met the criteria for both sepsis and pneumonia were classified as having pneumonia. We calculated Acute Physiology and Chronic Health Evaluation (APACHE II) score12, Simplified Acute Physiology Scores (SAPS II and 3)1314 and Sequential Organ Failure Assessment (SOFA) scores15. The following mechanical ventilation variables were recorded: peak airway pressure (Ppeak), plateau pressure (Pplat), positive end-expiratory pressure (PEEP), tidal volume (VT), respiratory rate (RR) and respiratory system compliance (CRS). All ventilatory variables were recorded daily at a fixed time at 0900 h.
In all patients diagnosis of malaria was made from OptiMAL-IT Malaria Test Kit (TCS Biosciences Ltd, UK), and four patients also had peripheral smear examination positive.
Diagnosis of viral aetiology: Real-time PCR was done only once to determine the viral aetiology of pneumonia using BAL fluid. Nucleic acid extraction was done using Roche L.C.2.0.l (Roche Diagnostics, Basel, Switzerland). The PCR was performed on every sample for detection of influenza A/B, respiratory syncytial virus (RSV), human metapneumovirus (hMPV) and adenovirus according to Centers for Disease Control and Prevention (CDC) protocol16. All influenza A positive samples were further subtyped using primers for seasonal AHINI, AH3N2 and pandemic AH1N116.
Estimation of biomarkers: A panel of five biomarkers [interleukin (IL-1β, IL-6, tumour necrosis factor-alpha (TNF-α), procalcitonin (PCT), high sensitivity C-reactive protein (hsCRP)] was measured in duplicate in serum samples that were collected at the time of enrollment. These biomarkers were chosen based on prior demonstration of their association with adverse outcomes1718. Five ml of venous blood was taken and kept at room temperature for two h and was later centrifuged at 1207 g for 10 min. The supernatant was stored at -70° C until analysis. Serum levels of all five variables were measured using enzyme linked immunosorbent assay (ELISA) according to the manufacturer's instruction (R&D Systems, Minneapolis, USA; Biocheck. Inc. Foster city, USA and Ray Biotech. Inc. Norcross, Georgia).
Statistical analysis: In absence of any prospective observational study on this topic from India, the sample size was calculated from the expected mortality of ARDS. With a sample size of 62, a two-sided 95 % confidence interval (CI) for the expected proportion of mortality among patients with ARDS, using the large sample, normal approximation will extend 12.5 per cent from the expected proportionary death of 50 per cent. Hence, a sample size of 65 was proposed. Continuous variables including age and SOFA score were summarized as mean ± standard deviation (SD). Categorical variables such as gender, sepsis and vasopressor use were summarized as proportions along with 95% CI. Skewed variables were summarized as median with interquartile range and non-parametric tests (Mann-Whitney U-test) were applied. Quantitative variables at admission were compared between survivors and non-survivors using Student's t test or Wilcoxon's rank sum test and qualitative variables by chi-square test. Using the day of death or discharge, Kaplan-Meier survival analysis was performed. Log rank test was used to compare the survival between different categories of each study variable. Multivariable cox regression analysis was done to identify independent predictors of mortality.
Results
All patients in the medical ICU, AIIMS were prospectively screened daily for ARDS between day 0 and day 7 of admission, using all available clinical and radiological data. Seventy one patients were found to have ARDS during the study period (Fig. 1). Seven patients were excluded as they had known previous lung pathology. Out of 78, seven patients with HIV were excluded. Sixty four patients with ARDS were finally included. Patients were predominantly males (60.9 vs. 39%). Their median age was 29 yr (24-49 yr). Patients were critically ill with baseline mean SOFA and SAPS II scores of 7.4 and 33.5, respectively. The majority (55/64, 85.9%) of patients had at least one non-pulmonary organ failure at admission. Thirty one of the 64 (48.4%) patients required vasopressor support at baseline. Twenty patients (31.2%) met the ARDS criteria 48 h after hospitalization and were subsequently included in the study.
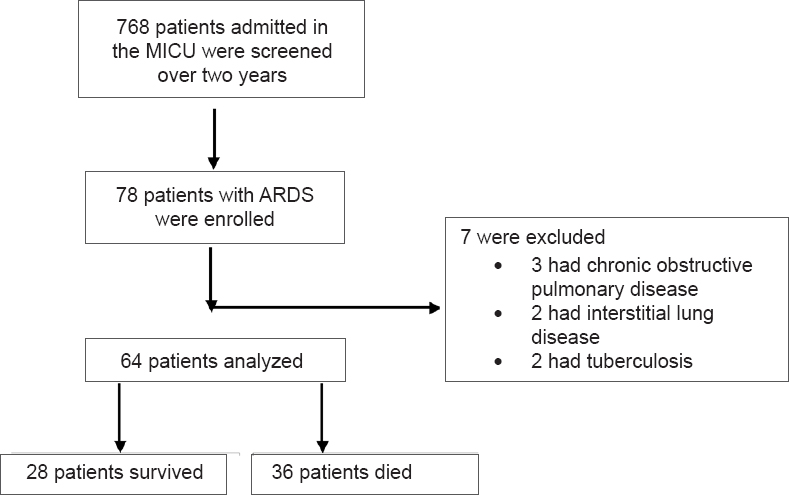
- Flowchart showing enrollment and follow up of the study participants.
The most common cause of ARDS was pneumonia [44/64 (68.7 %)], followed by malaria [9/64 (14.1%)] and sepsis [8/64 (12.5%)]. All the organisms isolated from cases of bacterial pneumonia were Gram-negative. Actinetobacter sp. was the most common organism [12/44 (27.27%)] isolated. Of the eight patients with viral aetiology, respiratory syncytial virus was isolated in three patients, adenovirus and influenza H1N1 in two patients each. Influenza H5N1 was responsible for pneumonia in one patient. There were no other bacteria or parasite isolated from the patients identified as viral pneumonia. Eight patients had sepsis in our study. Four patients had documented urinary tract infection (UTI), one had pelvic infection. In three patients source of sepsis could not be identified. There were five patients with tuberculosis; of whom, three patients had miliary tuberculosis who later died (Table I).
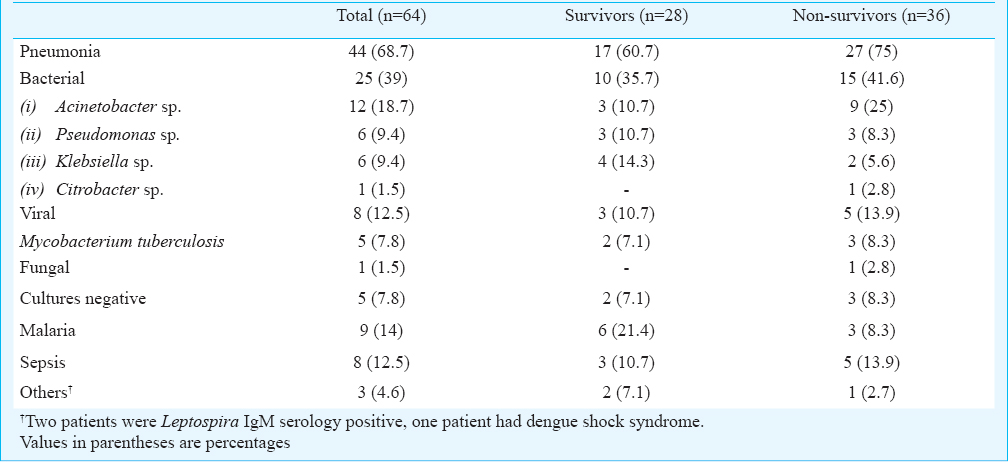
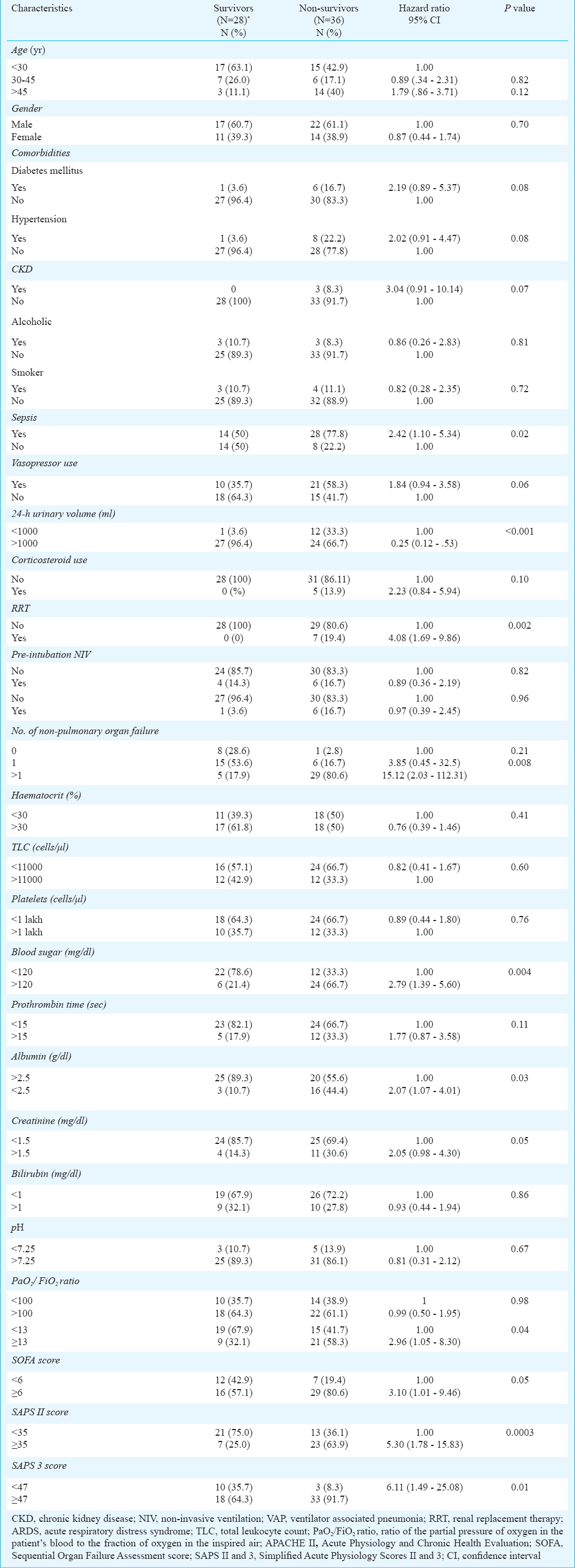
Table II depicts the baseline characteristics of survivors and non-survivors. Survivors were slightly younger as compared to non-survivors. Similarly, a decrease in the mean 24 h urinary volume was associated with a poor outcome (1354.3 ± 326.7 vs.1170.8 ± 393.1 ml; P<0.05). The baseline severity of illness scores (APACHE II, SOFA, SAPS II and SAPS 3) were significantly higher among non-survivors than survivors. Among biochemical variables, higher blood sugar at admission was associated with increased risk of mortality (140.2 ± 48.7 vs. 111.6 ± 5.5 mg/dl; P<0.01) and serum albumin at admission was lower among non-survivors (2.6 ± 0.5 vs. 2.9 ± 0.3 g/dl; P<0.01). There were no significant differences in the baseline ventilatory parameters except for significantly (P<0.001) higher Ppeak and PPlat among non-survivors (Table II).
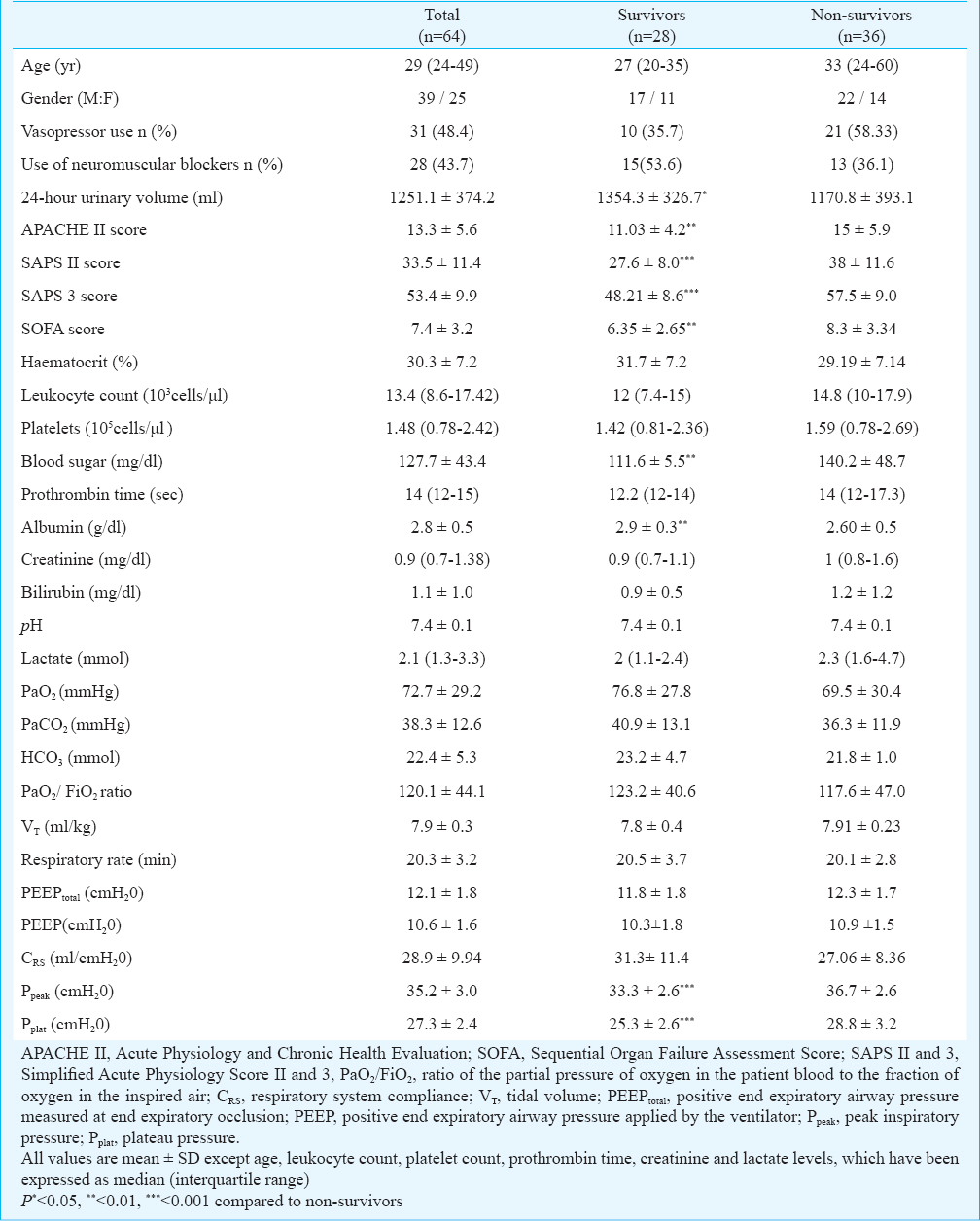
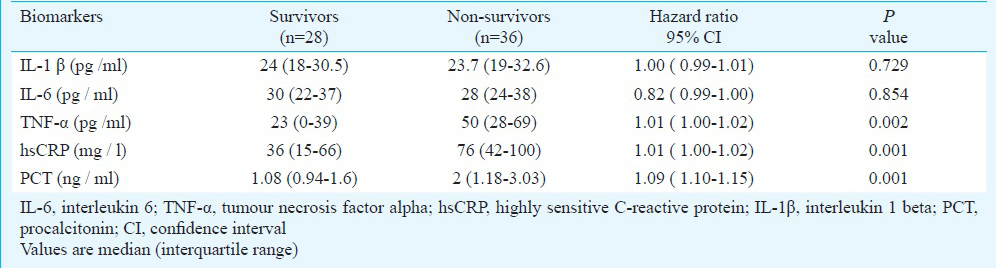
The 28-day mortality in the present study was 56.2 per cent (36/64). Baseline variables that predicted mortality in univariate analysis included 24 h urinary volume, sepsis, serum albumin and creatinine, RRT, non-pulmonary organ dysfunction, all the ICU severity of illness scores, serum hsCRP, procalcitonin, TNFα, Pplat and Ppeak (Tables II, III and IV). In multivariate analysis, non-pulmonary organ failure, SAPS II score and Ppeak at the time of admission were found to be independent predictors of mortality (Table V). To compare the survival probability of ARDS patients of different aetiologies we plotted the duration in ICU stay vs. cumulative survival probability in these groups using Kaplan-Meier survival estimate (Fig. 2). Since infectious aetiology was considered in most of these patients on admission, almost all of them received antibiotics from the first day itself.
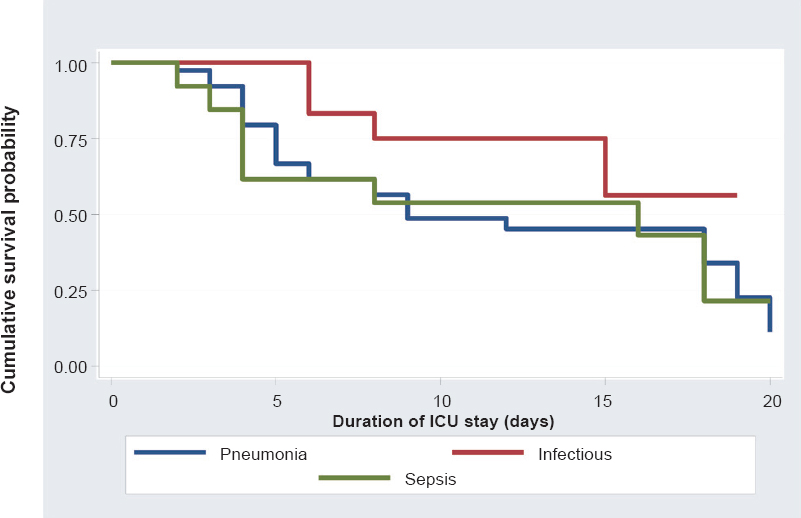
- Kaplan-Meier survival curve of 44 patients of pneumonia,12 patients of infectious aetiology (malaria, dengue and Leptospira) and eight patients of sepsis. There was no significant difference between the three categories. Curve is truncated at 20 days as there were only two deaths after 20 days (P value - 0.54).
Discussion
In the present study, the most common risk factor for development of ARDS was pneumonia followed by malaria. Acinetobacter sp. was the most common organism identified, but all these patients developed ARDS 48 h after hospitalization. Hence, it was not clear if these were hospital acquired or community acquired. There were five cases with falciparum malaria and four cases with vivax malaria. All these patients were given standard artemisinin-based combination therapy (ACT). One of the five patients with falciparum malaria and of the four patients with vivax malaria died. Eight patients had ARDS due to viral pneumonia including two patients with the pandemic influenza H1N1 infection. However, these were likely to be sporadic cases as there was no ongoing outbreak in the community during that period. Tuberculosis resulted in ARDS in five patients. A study from western India7 has reported extrapulmonary causes such as malaria (27.6%) and Leptospira (20.7%) as the commonest cause of ARDS.
Hypoproteinaemia has been shown to be a risk factor for the development of acute lung injury (ALI)/ARDS. In a retrospective analysis of patients with severe sepsis at risk for developing ALI/ARDS, Mangialardi et al19 showed that the initial serum total protein (STP) level and changes in STP level were most significant variables in predicting the development of ARDS. The Saline versus Albumin Fluid Evaluation (SAFE) study20 compared 4 per cent albumin and 0.9 per cent normal saline in patients requiring fluid resuscitation. Although there was no difference in mortality in the subgroups of patients with ARDS treated with albumin versus saline, there was a modest reduction in mortality in sepsis subgroup, with an adjusted odds ratio for mortality of 0.71 (95% CI 0.52 - 0.97, P=0.03). Low serum albumin was an independent predictor of mortality in univariate analysis in our study. Whether correcting or preventing hypoalbuminaemia will decrease ventilator dependent days and eventually improve survival still requires further investigation with large randomized studies. In our study higher blood sugar at admission was associated with increased risk of mortality. Hyperglycaemia during critical illness is common and is associated with increased mortality. Intensive insulin therapy maintaining blood sugar level less than 180 mg/dl has been shown to improve outcomes in some, but not in all studies20212222.
Several ICU severity of illness scores have been developed in the past for critically ill patients. However, their exact role in ARDS patients remains to be defined. We computed APACHE II12, SOFA15, SAPS II13 and SAPS 314 scores from the baseline variables and found that APACHE II ≥13, SAPS II≥35, SAPS 3≥47 and SOFA ≥6 were predictors of mortality in univariate analysis. SAPS II score was an independent predictor of mortality in multivariate analysis.
In the present study, 36 of 64 patients died, resulting in a 28-day mortality of 56.2 per cent. In one study from China8 mortality of 70.4 per cent (90-day mortality) and 55.7 per cent (in-hospital mortality), respectively have been reported. In a systematic review4 the pooled mortality has been shown to vary from 44 per cent (95% CI 40.1-47.5) for observational studies, and 36.2 per cent (95% CI 32.1-40.5) for randomized control trials. One possible explanation for the relatively high mortality noted in the current study could be small number of ARDS cases with extrapulmonary causes such as trauma, poisoning, pancreatitis, burns, etc. in which mortality is usually low23. Also, there could be a selection bias in the ICU admission policy of hospitals in resource-limited countries where only the most sick patients are admitted to the ICU because of limited availability of ICU beds.
Serum levels of the acute phase reactant C-reactive protein have been found to predict disease activity in patients with sepsis and pneumonia24. In the current study, higher serum hsCRP levels predicted mortality in univariate analysis. Bajwa et al17 measured serum level of C-reactive protein instead of hsCRP and reported higher CRP levels among survivors as compared to non-survivors. Higher CRP levels should correlate with unfavourable outcome as elevated CRP levels reflect ongoing inflammation. Our study suggested higher CRP level as a poor prognostic marker in ARDS patients and these results were similar to the application of CRP as an outcome parameter in various other diseases2324.
Procalcitonin is a 116 amino acid peptide and its levels are used in pneumonia for diagnosis, guiding duration of antibiotic therapy and prognosis25. In the present study, higher PCT levels predicted mortality in the univariate analysis. Tseng et al25 showed PCT as a prognostic biomarker in ARDS caused by community-acquired pneumonia. Meduri et al26 found that patients with higher plasma levels of TNF-α, IL-1 β, IL-6, and IL-8 on day one of ARDS had persistent elevation of these inflammatory cytokines over time and died. Higher TNF-α levels also predicted mortality in univariate analysis. Role of TNF-α in ARDS is controversial2728. As procalcitonin, hsCRP, TNF-α levels in the present study were not found to be independent predictors of mortality in multivariate analysis, these findings need confirmation in larger studies to establish their prognostic role in ARDS.
There was no difference in the baseline pulmonary variables such as RR, VT, CRS, level of PEEP among survivors and non-survivors except for higher Ppeak and Pplat in non-survivors. In the present study, higher Ppeak was an independent predictor of mortality. Ppeak is a function of flow resistance in the airways and the compliance of the lung and chest wall. Non-survivors could have had worse lung or chest wall compliance, which might explain the higher Ppeak in these patients. It is important to note that ventilatory parameters are usually worse at the time of admission and improve within a few hours with good ventilation strategy.
Our study had several merits. First, we demonstrated viruses as a common cause of ARDS in developing countries and should be actively searched as an important aetiology of ARDS particularly if targeted therapeutic strategies are available. Second, as reported by us earlier29, this study also showed tuberculosis as an important cause of ARDS and should be considered as a risk factor for development of ARDS. Third, use of easily available inflammatory markers such as hsCRP and procalcitonin might help in early stratification of severity of illness.
Our study also had several limitations. First, the sample size was small and the study duration was short. Second, the study was done in a medical ICU where patients with trauma, burns and pancreatitis are usually not admitted, hence these extrapulmonary causes of ARDS were not studied. Third, inflammatory markers were measured only at the baseline. Repeated measurements of these markers during the course of disease would have been more ideal. Fourth, ventilatory parameters were measured at a fixed time daily rather than taking repeated measurements throughout the day and then selecting the maximum and the minimum values.
In conclusion, Gram-negative bacteria, malaria, respiratory viruses and tuberculosis were common causes of ARDS. Non-pulmonary organ dysfunction, SAPS II score and Ppeak at the time of admission were individual predictors of mortality. Elevated levels of inflammatory markers such as hsCRP, procalcitonin, TNF-α at admission might identify patients at higher risk of death. These parameters may help in predicting mortality in patients with ARDS in a selected population, but our findings can not be generalized as there is always a referral bias with any study which is carried out at a tertiary care centre.
Acknowledgment
Authors acknowledge the nursing staff and other supporting staff of the intensive care unit of the department of Medicine, All India Institute of Medical Sciences, New Delhi, for support, and all laboratory personnel who assisted in this study.
Conflicts of Interest: None.
References
- Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526-33.
- [Google Scholar]
- The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818-24.
- [Google Scholar]
- Has mortality from acute respiratory distress syndrome decreased over time? A systematic review. Am J Respir Crit Care Med. 2009;179:220-7.
- [Google Scholar]
- [No authors listed]. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342:1301-8.
- [Google Scholar]
- Etiology and outcomes of pulmonary and extrapulmonary acute lung injury/ARDS in a respiratory ICU in North India. Chest. 2006;130:724-9.
- [Google Scholar]
- Clinical characteristics and outcomes of patients with acute lung injury and ARDS. J Postgrad Med. 2011;57:286-90.
- [Google Scholar]
- Retrospective analysis on acute respiratory distress syndrome in ICU. Chin J Traumatol. 2007;10:200-5.
- [Google Scholar]
- Identification of patients with acute lung injury. Predictors of mortality. Am J Respir Crit Care Med. 1995;152:1818-24.
- [Google Scholar]
- Early predictive factors of survival in the acute respiratory distress syndrome. A multivariate analysis. Am J Respir Crit Care Med. 1998;158:1076-81.
- [Google Scholar]
- NIH NHLBI ARDS Clinical Network Mechanical Ventilation Protocol Summary. Available from: http://www.ardsnet.org/files/ventilator_protocol_2008-07.pdf
- APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818-29.
- [Google Scholar]
- A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957-63.
- [Google Scholar]
- SAPS 3 - From evaluation of the patient to evaluation of the intensive care unit. Part 2: Development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med. 2005;31:1345-55.
- [Google Scholar]
- The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22:707-10.
- [Google Scholar]
- 2009. World Health Organization. CDC protocol of real- time PCR for influenza A (H1N1). Available from: http://www.who.int/csr/resources/publications/swineflu/CDCRealtimeRTPCR_SwineH1Assay-2009_20090430.pdf
- Plasma C-reactive protein levels are associated with improved outcome in ARDS. Chest. 2009;136:471-80.
- [Google Scholar]
- The predictive role of serum and bronchoalveolar lavage cytokines and adhesion molecules for acute respiratory distress syndrome development and outcome. Respir Res. 2002;3:25.
- [Google Scholar]
- Hypoproteinemia predicts acute respiratory distress syndrome development, weight gain, and death in patients with sepsis. Ibuprofen in Sepsis Study Group. Crit Care Med. 2000;28:3137-45.
- [Google Scholar]
- A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350:2247-56.
- [Google Scholar]
- A prospective randomised multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: The Glucontrol study. Intensive Care Med. 2009;35:1738-48.
- [Google Scholar]
- C-reactive protein levels in community-acquired pneumonia. Eur Respir J. 2003;21:702-5.
- [Google Scholar]
- Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195-207.
- [Google Scholar]
- Procalcitonin is a valuable prognostic marker in ARDS caused by community-acquired pneumonia. Respirology. 2008;13:505-9.
- [Google Scholar]
- Persistent elevation of inflammatory cytokines predicts a poor outcome in ARDS. Plasma IL-1 beta and IL-6 levels are consistent and efficient predictors of outcome over time. Chest. 1995;107:1062-73.
- [Google Scholar]
- Plasma levels of tumor necrosis factor in the adult respiratory syndrome. Am Rev Respir Dis. 1991;143:590-2.
- [Google Scholar]
- Early and marked up-regulation of TNFα in acute respiratory distress syndrome after cardiopulmonary bypass. Front Med. 2012;6:296-301.
- [Google Scholar]
- Predictors of development and outcome in patients with acute respiratory distress syndrome due to tuberculosis. Int J Tuberc Lung Dis. 2006;10:429-35.
- [Google Scholar]






