Translate this page into:
A clinicopathological study of primary central nervous system lymphomas & their association with Epstein-Barr virus
Reprint requests: Dr Mehar C. Sharma, Department of Pathology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110 029, India e-mail: sharmamehar@yahoo.co.in
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Primary central nervous system lymphomas (PCNSLs) are relatively uncommon, accounting for 2-3 per cent of primary brain tumours. Majority of these are diffuse large B cell lymphomas (DLBCL) occurring both in immunocompromised and immunocompetent patients. We undertook this study to classify PCNSL into germinal centre (GC) and non-germinal centre (NGC) type based on Hans classification and to find the role of Epstein-Barr virus (EBV) in pathogenesis both by conventional immunohistochemistry (IHC) and chromogenic in situ hybridization (CISH).
Methods:
The consecutive cases of PCNSL during a 10 years period were analysed by IHC for CD45, CD20, CD3, B-cell lymphoma 2 and 6 (Bcl-2 and Bcl-6), B-cell specific octamer binding protein-1 (BOB-1), multiple myeloma oncogene-1 (MUM-1), EBV latent-membrane protein 1 (LMP-1), cyclin-D1, CD10, CD5 and CD23, as well as by CISH for EBV.
Results:
During a period of 10 years, 65 PCNSL were diagnosed which comprised 0.69 per cent (65/9476) of all intracranial tumours. The mean age of presentation was 49 yr with sex ratio (M:F) of 1.4:1. Most common location was supratentorial region with predominant involvement of frontal lobe. Single lesions were seen in 38 (58.4%) and multifocal lesions in 27 (41.5%) patients. None of the patients were immunocompromised. All cases were B cell immunophenotype and were DLBCL except one case of follicular lymphoma. According to Hans classification, majority of them were NGC (n=51, 79.6%) and 13 (20.3%) were GC type. Bcl-2 expression was noted in 34 (52.3%) tumours. EBV was positive in three (4.6%) cases; two were detected both by IHC and CISH and one case by CISH only.
Interpretation & conclusions:
In Indian population, PCNSL occurs mainly in immunocompetent patients, and a decade earlier than in western population. Immunophenotyping revealed that all cases were DLBCL with predominance of NGC type. No prognostic difference was seen between GC and NGC DLBCL. Association of EBV was rare and this virus was possibly not involved in the pathogenesis of PCNSL in immunocompetent individuals. CISH was an easy, economical and less cumbersome method for detection of EBV in PCNSL.
Keywords
CISH
CNS
DLBCL
EBV
GC
IHC
Hans classification
lymphoma
NGC
PCNSL
Primary central nervous system lymphomas (PCNSLs) are the rare brain tumours accounting for 2-3 per cent of all primary brain tumours and <1 per cent of all non-Hodgkin's lymphomas1. World Health Organization (WHO) classification of haematopoietic and lymphoid tissues describes these as diffuse large B-cell lymphoma of the central nervous system (CNS DLBCL) representing all primary intracerebral, spinal or intraocular lymphomas1. Lymphomas of CNS with evidence of systemic disease at the time of presentation are excluded. In the last few decades, a rise in the number of cases has been observed mainly in association with acquired immunodeficiency syndrome (AIDS) but this has started declining after introduction of highly active anti-retroviral therapy (HAART)2. Although immunodeficiency either inherited or acquired is a major risk factor for the development of PCNSL, but this increase in incidence has been reported in immunocompetent patients also23. Usual age of onset reported is between 6th to 7th decades of life, but these occurred earlier in immunocompromised individuals4. A few studies published from India found that age of presentation is a decade earlier than western population5678910111213. Epstein-Barr-virus (EBV) is demonstrated to be associated with PCNSL in most of the immunocompromised patients, while rarely in immunocompetent patients14. Although a few studies of PCNSL are published from India but none of these classified CNS lymphoma according to Hans classification15, and role of EBV was not studied by chromogenic in situ hybridization (CISH) which is a sensitive and specific method for detection of this virus.
We undertook this study with an aim to subtype PCNSL according to Hans classification for DLBCL and to find out role of EBV in PCNSL pathogenesis both by conventional immunohistochemistry (IHC) for latent membrane protein-1 (LMP-1) and CISH.
Material & Methods
All consecutive cases diagnosed as PCNSL during a period of 10 years (2004 -2013) in the department of Pathology, All India Institute of Medical Sciences, New Delhi, India, were retrospectively included in this study. The slides and blocks were retrieved from archives of the department. Hematoxylin and Eosin (H&E) stained sections were reviewed by three independent neuropathologists, and consensus diagnoses were made according to the WHO classification of tumors of the central nervous system4. Three cases were excluded from the study one of which was a case of Hodgkin's lymphoma and two were anaplastic large cell lymphomas involving sphenoid sinuses. Finally, 65 cases with sufficient material in tissue blocks and diagnostic concurrence were included in the study.
Tumour samples received in neutral buffered formalin were routinely processed and paraffin embedded. Five micron thick sections were cut for H&E staining and for IHC. Reticulin staining was done to highlight the perivascular framework of tumour cells. For immunohistochemical staining, streptavidin biotin conjugate immunoperoxidase method16 was used, after appropriate antigen retrieval wherever required. Immunohistochemical studies were performed on 5µ thick formalin fixed, paraffin-embedded tumour sections using antibodies directed against CD45 (Dako, Denmark, dilution 1:100), CD20 (Neomarker, USA, dilution, 1:200), CD3 (Dako, dilution, 1:100), B-cell lymphoma 2 (Bcl-2) (Neomarker, dilution, 1:50) and multiple myeloma oncogene 1 (MUM-1) (dilution, 1: 200), B-cell specific octamer binding protein-1 (BOB-1) (dilution, 1:200), Epstein-Barr virus latent membrane protein 1 (EBV LMP-1) (dilution 1:200), cyclin-D1 (dilution 1:100), CD10 (dilution 1:50), CD5 (dilution 1:25), CD23 (dilution 1:100), CD15 (dilution 1:200), CD30 (dilution 1:100) and B-cell lymphoma 6 (bcl-6) (dilution 1:100) all from Diagnostic BioSystems, USA. Labelled streptavidin biotin kit (Universal) was used as a detection system (Dako, Denmark). Antigen retrieval was performed in a microwave oven using citrate buffer at pH 6.0 for all antibodies except bcl-6, for which ethylenediamine tetra acetic acid (EDTA) was used. For each batch, appropriate positive controls were taken and for negative controls primary antibodies were omitted.
CISH technique: CISH study was performed on 5µ thick formalin fixed paraffin-embedded tumour sections using Zytofast PLUS CISH implementation kit HRP-DAB (Zyto Vision GmBH, Germany). Standard deparaffinization technique as used for IHC was followed by 10 min incubation in 3 per cent H2O2. Following rinsing in deionized water (DW), target retrieval was achieved using pepsin digestion in humidity chamber for 15 min. Slides were incubated in EDTA solution at 95°C in a boiling water bath for 15 min after washing in DW. Slides were washed in DW and drained off; 10 μl of CISH probe was poured over each slide, and covered with a cover slip using glue. Denaturation at 75°C for 5 min was subsequently followed by hybridization at 37°C for 60 min in the Thermobrite TM hybridization chamber (Vysis Inc., USA). Tris-buffered-saline (TBS) washing, at 55°C and room temperature, each for five min was done concurrently after removal of cover slip. Mouse-anti-DIG (Zyto Vision GmBH, Germany) was poured drop-wise over each slide, and incubated in a humidity chamber at 37°C for 30 min. Three washings, each for a minute with TBS was done, before and after incubating slides in anti-mouse-HRP-polymer for 30 min at room temperature. 3,3’-diaminobenzidine (DAB) solution was prepared as per guidelines (Zytofast PLUS CISH) and poured 3-4 drops in each slide for 10 min at room temperature, and washed in running tap water for two min. Haematoxylin was used for counterstaining. Slides were dehydrated in graded alcohol solutions, air dried and mounted with DPX. Slides were examined under light microscope for evaluation. Only nuclear positivity was taken into account.
Classification of tumours as GC and NGC type: Tumours were sub-classified according to immunoprofile expression using Hans classification system15. In the Hans classification a decision tree is devised based on three markers: CD10, Bcl-6, and MUM-1 to distinguish DLBCL into two subgroups. CD10+ only, both Bcl-6+ and CD10+ and CD10-, Bcl-6+ and MUM-1- positive cases were assigned to the GC group. NGC group included cases with CD10- and one of either combinations Bcl-6+ and MUM-1+ or Bcl-6- and MUM-1+. The cases with all three negative markers were assigned to NGC group.
Results
During a period of 10 years (2004-2013), a total of 9476 intracranial tumours including 4573 (48.2%) of glial tumours were diagnosed in the department of Pathology. Of these, 65 cases were of PCNSL which comprised 0.69 per cent (65/9476) of all intracranial tumours. There was no absolute increase in the incidence of PCNSL in the last decade (Fig. 1).
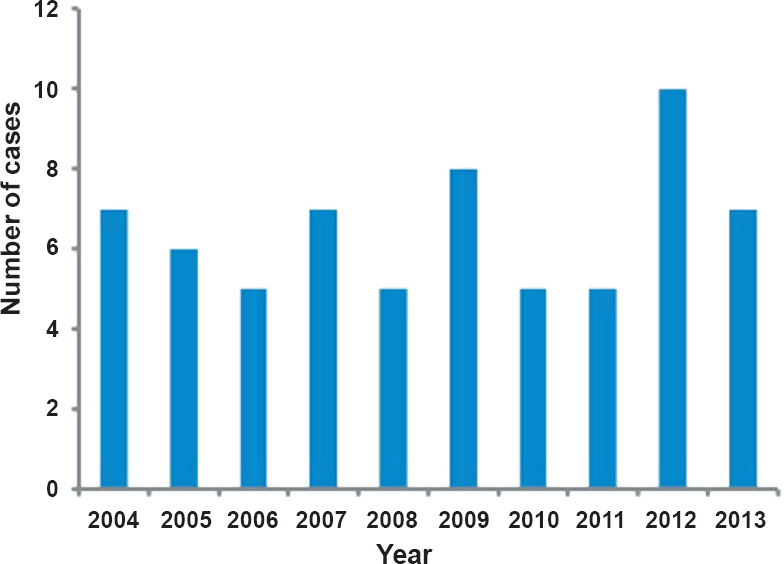
- Year wise incidence of primary central nervous system lymphoma (PCNSL).
Clinicopathological parameters (Table): PCNSL showed a wide age distribution range varying from 14 to 80 yr with a mean age of 49 yr at presentation. Ten patients were under 30 yr age group. A male predominance with a male to female ratio of 1.4:1 was noted. A vast majority of cases were supratentorial (ST) in location (56/65; 85%), followed by infratentorial region (6/65; 9%), and in 4.61 per cent (3 cases) both ST and IT were involved. Within the ST region the most common location was frontal lobes (45%) followed by parieto-occipital (11%), temporo-parietal (7%), basal ganglia (7%), all cortical lobes (7%), thalamus (5%), parietal (5%), occipital (5%) and one case each in selllar-suprasellar, temporal and fronto-temporal region. In the infratentorial region three tumours were in the cerebellum, two in fourth ventricles and one case occurred in the brainstem. Meningeal infiltration was noted in two cases (3.0%). Single lesions were seen in 38/65 (58.46%) of the patients and multiple lesions in 27/65 (41.53%). All cases were non reactive for HIV by ELISA test.
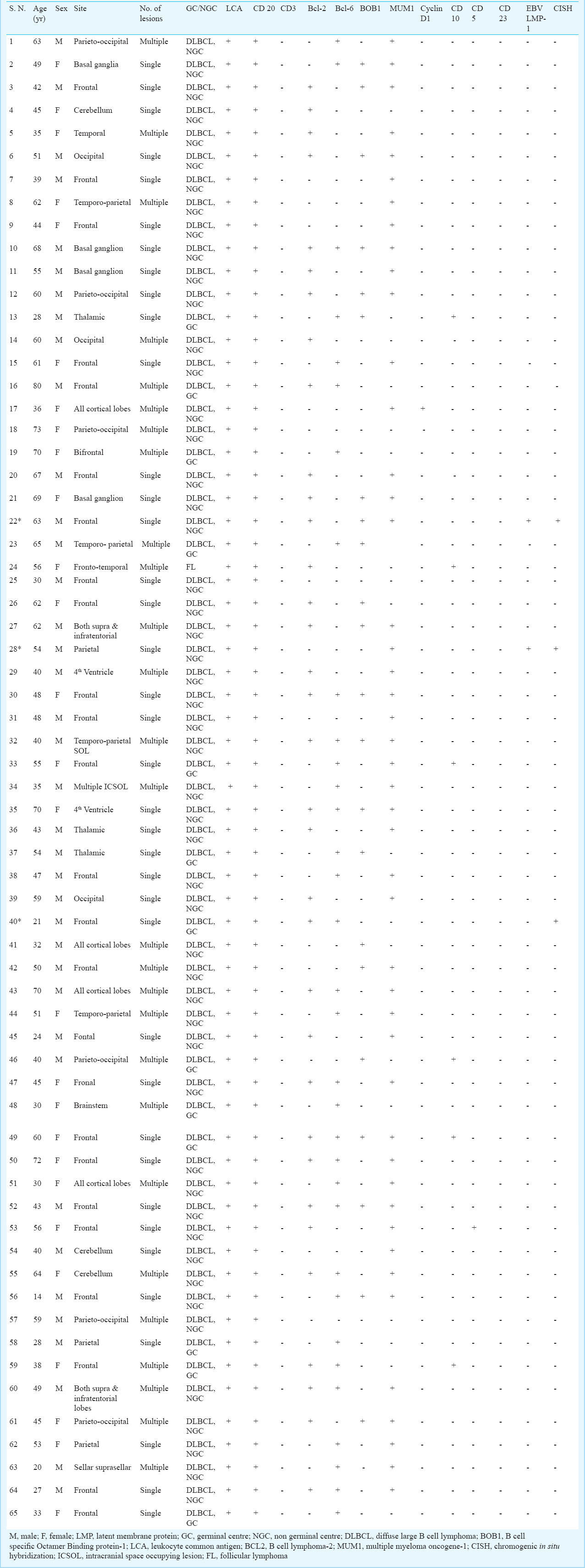
Pathologic findings and imunophenotyping: Tumours were composed of large cells with vesicular nuclei and prominent nucleoli admixed with some mature looking lymphoid cells. Perivascular cuffing and prominent network of reticulin was evident in majority of cases (Fig. 2). Necrosis was observed in 50 per cent of the cases. In five cases diagnoses were missed and were diagnosed as viral encephalitis. These patients were on steroids. A repeat biopsy clinched the diagnosis.
- Showing H&E staining of non-germinal centre (NGC) diffuse large B cell lymphoma (DLBCL) with immunopositivity for CD20, MUM-1 and reticulin rich network (X 200 each). DAB was used as chromogen.
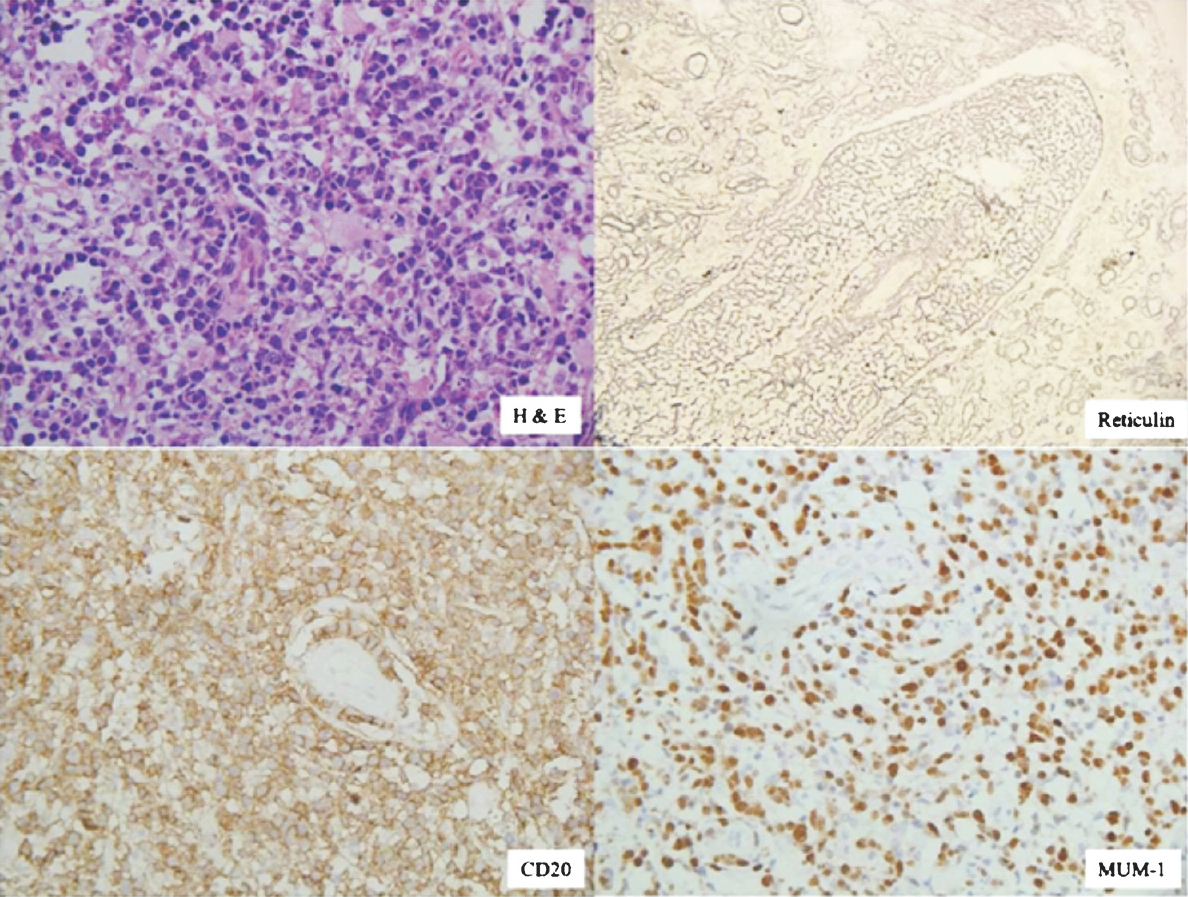
All the tumours were immunopositive for CD45 and CD20 and were B immunophenotype. DLBCL comprised 98.4 per cent (64/65) of the cases and a single case was of follicular lymphoma (FL). The FL was immunopositive for CD10, Bcl-2 besides CD20 and CD45. Of the 64 cases of DLBCL, 79.68 per cent (51/64) were non-germinal centre type (NGC) and 20.31 per cent (13/64) were of germinal centre type. Of the 51 NGC-DLBCL, 41.1 per cent (21/51) showed reactivity to both Bcl-6 and MUM-1, 43.3 per cent (23/51) to MUM-1 only and 13.7 per cent (7/51) were non-reactive to both these markers (Figs 2, 3). Among GC-DLBCL, 30.7 per cent (4/13) were immunopositive for Bcl-6 and CD10 while the rest 61.5 per cent (8/13) and 7.6 per cent (1/13) were immunoreactive only to Bcl-6 and CD10, respectively. Bcl-2 expression was noted in 52.30 per cent (34/65) cases. Cyclin-D1, CD5 and CD23 were immunonegative in all cases. LMP-1 immunopositivity was seen in only two cases in the cytoplasm.
- Non-germinal centre (NGC) diffuse large B cell lymphoma (DLBCL) showing perivascular cuffing of the tumour cells in H&E staining (arrow) with immunopositivity for CD20, Bcl-6 and MUM-1 (X 200 each). DAB was used as chromogen.
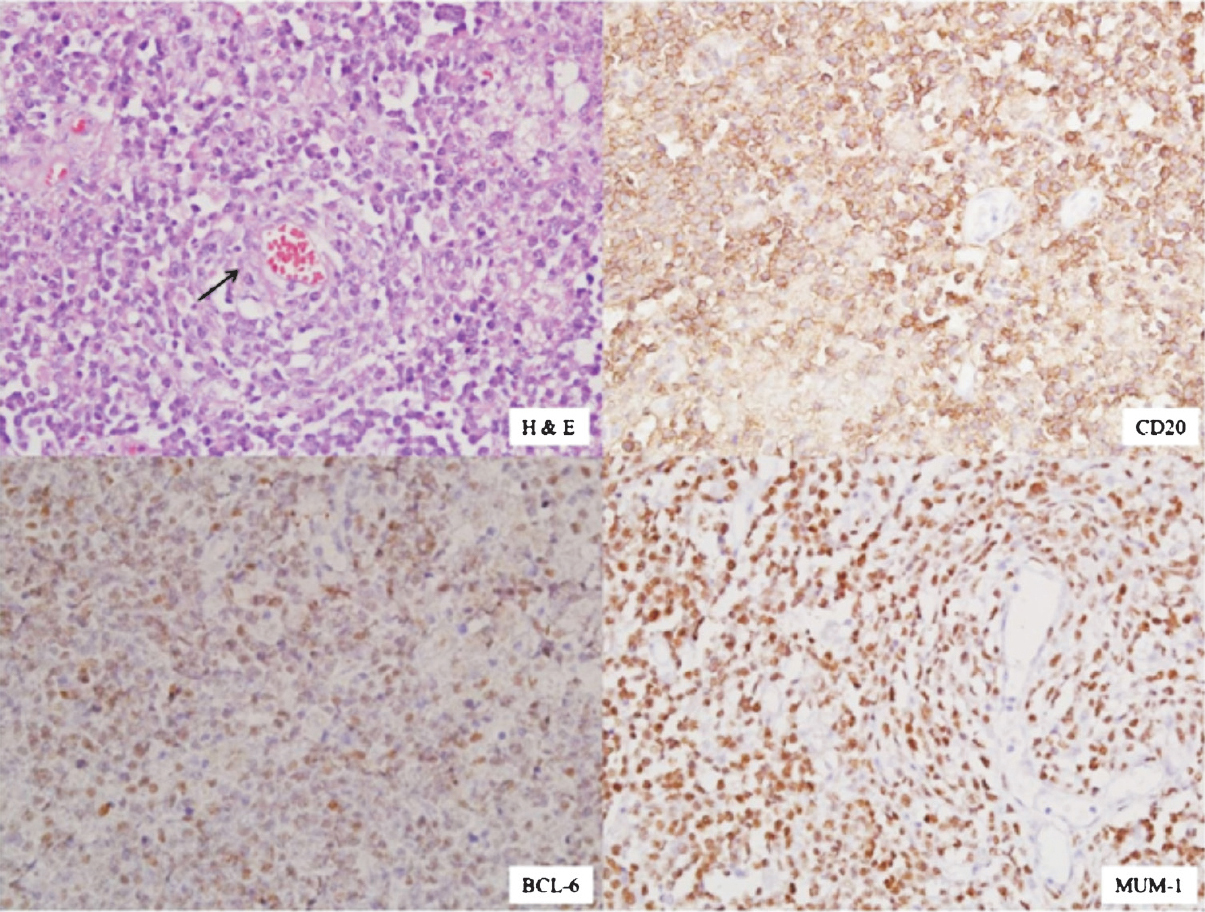
CISH study: CISH showed positivity for EBV only in three cases (4.6%), of whom two were immunopositive for LMP by IHC. EBV positivity was seen in two cases of NGC (case nos 22 & 28) and one case of GC type (case 40) (Fig. 4). Only in one case there was discordance between the two methods. EBV positivity by CISH was stronger as compared to LMP immunopositivity. This positivity was observed in a few cells which were neoplastic. None of the mature looking lymphoid cells were positive.
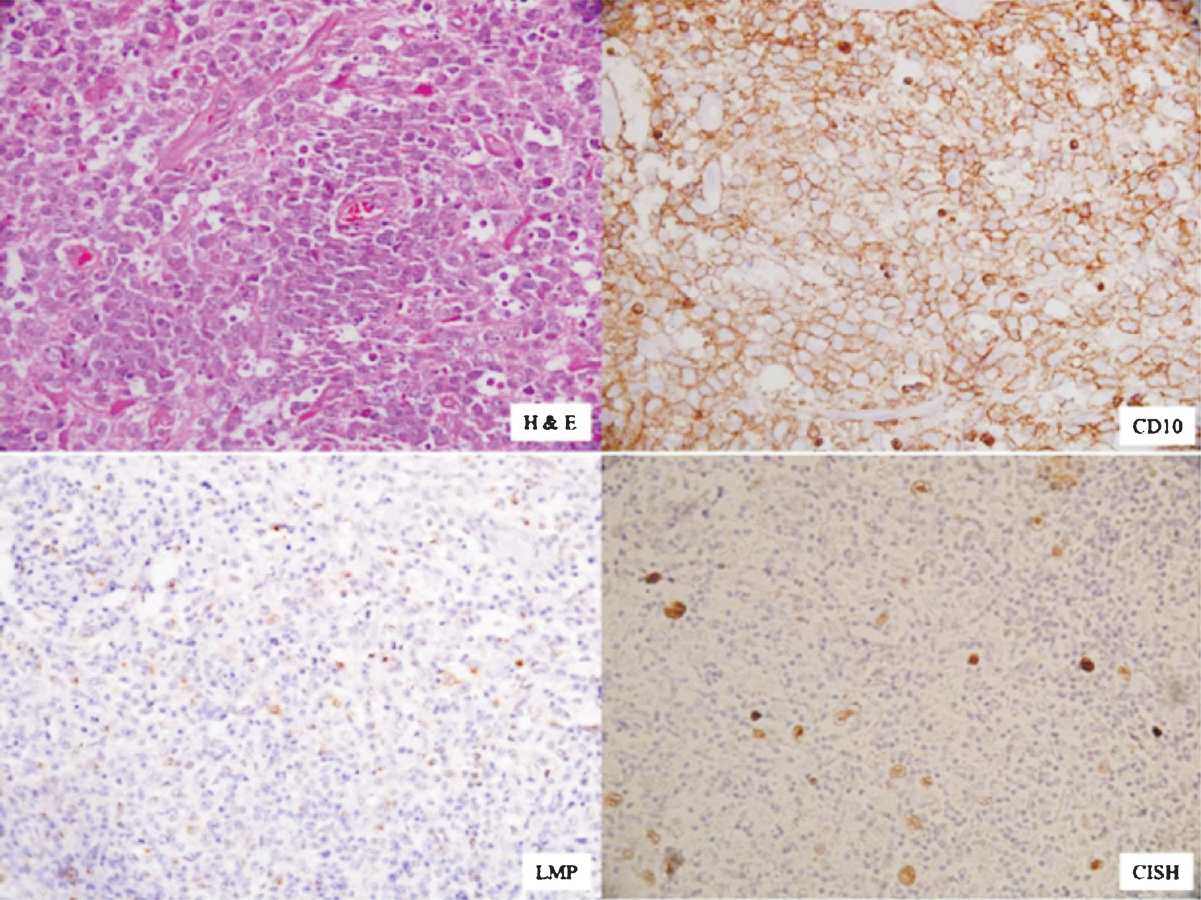
- Showing H&E staining of GC DLBCL with immunopositivity for CD10, LMP-1 (cytoplasmic) and chromogenic in situ hybridization (CISH) positivity (nuclear) for EBV(X 400 each). DAB was used as choromogen.
Discussion
PCNSL is relatively a rare but distinct form of extranodal lymphoma commonly seen in the immunocompromised individuals. Initially, with increased incidence of HIV, it was predicted that PCNSL would surpass the glial tumours; however, the incidence decreased possibly with introduction of HAART217. PCNSL constituted 0.69 per cent of all intracranial tumours and 1.42 per cent of all glial tumours in the present study, similar to that reported earlier568. Manoj et al13 from south India reported an increase in the incidence in PCNSL. In the present study, there was no absolute increase in the incidence of PCNSL and these results were similar to previous study from our centre5.
The PCNSL occurred over a wide age range with a peak incidence in the sixth or seventh decades in immunocompetent, and at a younger age in immunocompromised individuals4. All individuals with congenital as well acquired immunodeficiency are prone to develop PCNSL. Interestingly, the age of onset was a decade earlier in Indian patients who were immunocompetent5678910111213. Immunodeficiency is the major predisposing factor for the development of PCNSL, but none of our patient was immunodeficient. This has been observed earlier also from our centre as well as from other centres from India5612. Manoj et al13 reported a large series of 76 patients of PCNSL and found HIV association in three of 35 patients (8.6%) tested. This observation was duplicated in most of the studies from India810. In a series of 56 patients Paul et al8 found only one patient to be HIV positive.
It has been observed that peripheral DLBCL do not have uniform behaviour. Alizadeh et al18 and Rosenwald et al19 have shown that (based on molecular profiling) DLBCL are two different groups. Further, Hans et al15 have shown that these groups can be segregated into two categories by immunohistochemical staining and both subgroups are prognostically different. Systemic DLBCLs have been shown to pose a more heterogenous clinical and immunohistochemical features20. Many large studies on systemic DLBCL have shown that NGC DLBCLs behave in worse manner as compared to GC DLBCL. However, PCNSL have been found to be more homogenous and have aggressive behaviour and poor prognosis2122. Camilleri-Broët et al21 reported a series of 83 patients of DLBCL of brain and found 96.3 per cent of them were NGC subtype and attributed poor prognosis to this subtype. Similar results were reported by Bhagavathi et al22 in another study. In the present study of PCNSL, the NGC subtype was the predominant group and comprised 80 per cent of the cases but this was not that dominant as reported in earlier studies2122.
EBV is commonly implicated in the aetiopathogenesis of various lymphoproliferative disorders in immunocompromised individuals including PCNSL but less frequently in immunocompetent individuals23. Rao et al7 studied 11 cases of PCNSL for EBV by in situ hybridization and found only one case to be positive, HIV status of that patient was not known. Tandon et al9 reported 19 patients of PCNSL and all of them were immunopositive for LMP of EBV; however, none was positive by in situ hybridization, thus suggesting false positivity by IHC. In the present study of 65 patients of PCNSL, only three were positive for EBV; two by IHC for LMP and CISH and one additional case was detected with CISH technique but was missed by IHC. Therefore, our study showed that EBV was infrequently associated with the development of PCNSL in immunocompetent patients. Further, there is a possibility that EBV may also not be the aetiological agent of PCNSL in HIV patients. These observations are supported by some earlier studies from India2425. Lanjewar et al24 from western part of India, reported central nervous system changes in 84 autopsies conducted on HIV positive individuals and did not find any case of PCNSL. This is further supported by another study on 135 patients by Sharma et al25 who did not find any case of PCNSL except two cases of peripheral non Hodgkin's lymphoma. This low incidence of PCNSL could be due to short survival of AIDS patients as HAART was not available in India earlier. There is a possibility that with increasing awareness, affordability, free availability of treatment from government agencies and longer survival of these patients the number of PCNSL will increase in future.
Several laboratory detection techniques have been advocated for EBV. Southern blotting detection of EBV-DNA requires frozen tissue which can be used to determine the EBV clonality based on the variable number of tandem repeat sequences at the end of each EBV DNA molecule. Detection of EBV related antigens by IHC gives inconsistent results due to variable expression profiles26. A PCR based positivity may occur due to EBV-DNA in reactive lymphocytes26. Paraffin section DNA in situ hybridization using radiolabelled probes is a difficult and time consuming technique due to low concentration of specific nucleotide sequences and masking by the associated proteins. However, CISH is a simple and convenient technique with high sensitivity and specificity which can be incorporated in the routine evaluation of EBV association in PCNSLs.
To conclude, PCNSLs occurred a decade earlier in Indian patients and primarily in immunocompetent patients. There was no absolute increase in the incidence of PCNSL over a period of 10 years, although number of cases diagnosed per year increased. NGC subtypes were the most common and probably attributed to the poor prognosis. EBV was not the aetiological factor for PCNSL in India. CISH is a good and easy technique for the detection of EBV in PCNSL.
Acknowledgment
Authors acknowledge Shri Ravi for helping in CISH technique and Shri Pankaj and Shrimati Kiran for performing immunohistochemistry.
Conflicts of Interest: None.
References
- Primary diffuse large B-cell lymphoma of the CNS. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW, eds. WHO classification of tumours of haematopoietic and lymphoid tissues (4th ed). Lyon, France: International Agency for Research on Cancer; 2008. p. :240-1.
- [Google Scholar]
- Decreasing incidence rates of primary central nervous system lymphoma. Cancer. 2002;95:193-202.
- [Google Scholar]
- Primary central nervous system lymphomas in 72 immunocompetent patients: pathologic findings and clinical correlations. East West Group for the Study of Leucénies and Other Diseases of the Blood (GOELAMS) Am J Clin Pathol. 1998;110:607-12.
- [Google Scholar]
- Malignant lymphomas. In: Louis DN, Ohgaki H, Wiestler OD, Cavenee WB, eds. WHO classification of tumours of the central nervous system (4th ed). Lyon, France: International Agency for Research on Cancer; 2007. p. :188-92.
- [Google Scholar]
- Primary central nervous system lymphoma - a hospital based study of incidence and clinicopathological features from India (1980-2003) J Neurooncol. 2005;71:199-204.
- [Google Scholar]
- A study of primary central nervous system lymphoma in northern India. Surg Neurol. 2002;57:113-6.
- [Google Scholar]
- Association of primary central nervous system lymphomas with the Epstein-Barr virus. Neurol India. 2003;51:237-40.
- [Google Scholar]
- Primary central nervous system lymphomas: Indian experience, and review of literature. Indian J Cancer. 2008;45:112-8.
- [Google Scholar]
- Epstein-Barr virus as a possible etiologic agent in primary central nervous system lymphoma in immunocompetent individuals. Neurol India. 2009;57:36-40.
- [Google Scholar]
- Primary central nervous system lymphoma: a profile of 26 cases from Western India. Neurol India. 2009;57:756-63.
- [Google Scholar]
- Primary central nervous system lymphoma: prognostication as per international extranodal lymphoma study group score and reactive CD3 collar. J Postgrad Med. 2009;55:247-51.
- [Google Scholar]
- Primary central nervous system lymphoma: a study of clinicopathological features and trend in western India. Indian J Cancer. 2011;48:199-203.
- [Google Scholar]
- Central nervous system lymphoma: Patterns of incidence in Indian population and effect of steroids on stereotactic biopsy yield. Neurol India. 2014;62:19-25.
- [Google Scholar]
- Brain lymphomas of immunocompetent and immunocompromised patients: study of the association with Epstein-Barr virus. Mod Pathol. 1993;6:427-32.
- [Google Scholar]
- Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103:275-82.
- [Google Scholar]
- Use of avidin-biotin peroxidase complex (ABC) in immunoperoxidase techniques: a comparison between ABC and unlabeled antibody (PAP) procedures. J Histochem Cytochem. 1981;29:577-80.
- [Google Scholar]
- Pathology with clinical correlations of primary central nervous system non-Hodgkin's lymphoma. The Massachusetts General Hospital experience 1958-1989. Cancer. 1994;74:1383-97.
- [Google Scholar]
- Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature. 2000;403:503-11.
- [Google Scholar]
- Lymphoma/Leukemia Molecular Profiling Project: the use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. N Engl J Med. 2002;346:1937-47.
- [Google Scholar]
- Immunohistochemical expression patterns of germinal center and activation B-cell markers correlate with prognosis in diffuse large B-cell lymphoma. Am J Surg Pathol. 2004;28:464-70.
- [Google Scholar]
- A uniform activated B-cell-like immunophenotype might explain the poor prognosis of primary central nervous system lymphomas: analysis of 83 cases. Blood. 2006;107:190-6.
- [Google Scholar]
- Activated B-cell immunophenotype might be associated with poor prognosis of primary central nervous system lymphomas. Clin Neuropathol. 2008;27:13-20.
- [Google Scholar]
- Primary cerebral lymphoma: a study of 47 cases probed for Epstein-Barr virus genome. J Clin Pathol. 1992;45:587-90.
- [Google Scholar]
- Profile of central nervous system pathology in patients with AIDS: an autopsy study from India. AIDS. 1998;12:309-13.
- [Google Scholar]
- Spectrum of clinical disease in a series of 135 hospitalised HIV-infected patients from north India. BMC Infect Dis. 2004;4:52-60.
- [Google Scholar]
- Molecular diagnosis of Epstein-Barr virus-related diseases. J Mol Diagn. 2001;3:1-10.
- [Google Scholar]






