Translate this page into:
Postural & striatal deformities in Parkinson's disease: Are these rare?
Reprint requests: Dr Sanjay Pandey, Department of Neurology, Room no. 507, Academic Block, GB Pant Hospital, Delhi 110 002, India e-mail: sanjaysgpgi2002@yahoo.co.in
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution NonCommercial ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Parkinson's disease (PD) is the most common neurodegenerative disease and is characterized by tremor, rigidity and akinesia. Diagnosis is clinical in the majority of the patients. Patients with PD may have stooped posture but some of them develop different types of postural and striatal deformities. Usually these deformities are more common in atypical parkinsonian disorders such as progressive supranuclear palsy and multisystem atrophy. But in many studies it has been highlighted that these may also be present in approximately one third of PD patients leading to severe disability. These include antecollis or dropped head, camptocormia, Pisa syndrome, scoliosis, striatal hands and striatal toes. The pathogenesis of these deformities is a complex combination of central and peripheral influences such as rigidity, dystonia and degenerative skeletal changes. Duration of parkinsonism symptoms is an important risk factor and in majority of the patients these deformities are seen in advanced statge of the disease. The patients with such symptoms may initially respond to dopaminergic medications but if not intervened they may become fixed and difficult to treat. Pain and restriction of movement are most common clinical manifestations and these may mimick symptoms of musculoskeletal disorders like rheumatoid arthritis. Early diagnosis is important as the patients may respond to adjustment in dopaminergic medications. Recent advances such as deep brain stimulation (DBS) and ultrasound guided botulinum toxin injection are helpful in management of these deformities in patients with PD.
Keywords
Deformities
Parkinson's disease
postural
striatal
Introduction
James Parkinson in his essay on shaking palsy described the propensity to bend forward as an important feature of Parkinson's disease (PD)1. In one of his case description he highlighted that as the disease progressed to its last stage the trunk permanently bowed. Later Charcot described the extension of great toe and flexion of other toes as an important feature of PD which is now known as striatal toe2. Since then although there are many published studies3456 on postural and striatal deformities in PD but these are still considered to be rare and if present, raises a possibility of atypical Parkinsonian disorders such as progressive supranuclear palsy (PSP), multiple system atrophy (MSA) and drug induced parkinsonism (DIP). The classical deformity described in a PD patient is stooped posturing characterized by flexion of hips and knees. Patients with atypical parkinsonism have severe type of postural deformities which may also be present at the onset but PD patients usually have these deformities in advanced stages many years after the initial diagnosis. These deformities cause significant pain, discomfort and walking difficulty leading to severe disability and poor quality of life4. On many occasions these deformities are wrongly diagnosed as skeletal and joint disorders leading to wrong diagnosis and management. The aim of this review is to highlight that postural and striatal deformities are not rare in PD patients and these need to be identified and treated at the earliest possible time.
Types of deformities
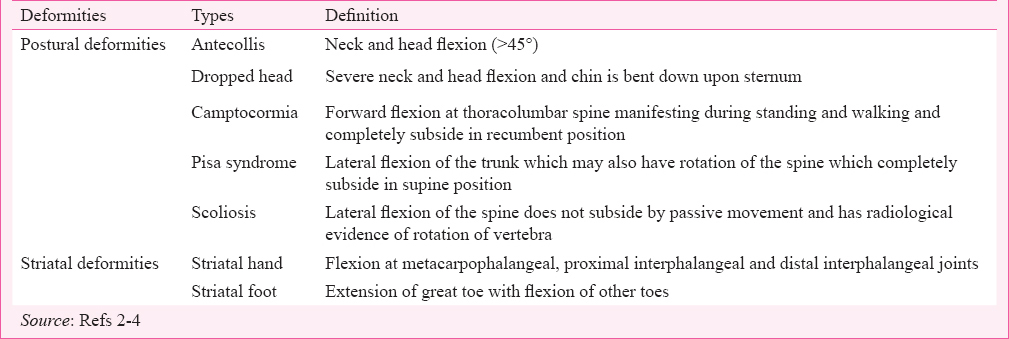
Parkinson's disease patients may have different types of postural deformities (Table I and Fig. 1) in sagittal and coronal planes3. Deformities in sagittal plane include anteocollis, dropped head, and camptocormia. Pisa syndrome and scoliosis are coronal plane deformities.
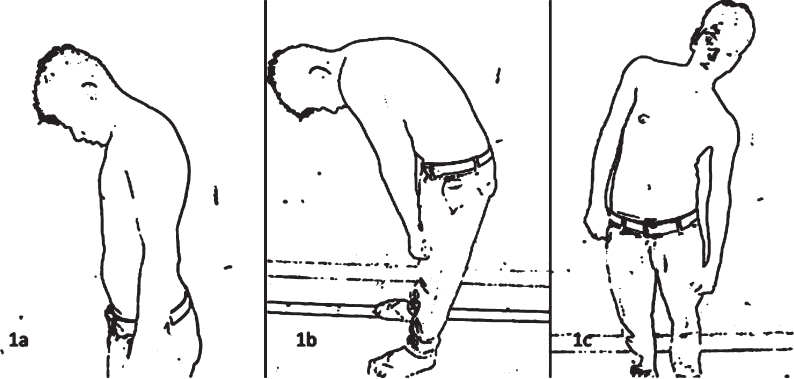
- Line diagrams showing antecollis (a), camptocormia (b) and Pisa syndrome (c).
Retrocollis is rarely seen in PD patients and usually considered as a red flag sign for the diagnosis. Striatal deformities may inolve hand (striatal hand) or toes (striatal toes)4. These may either be present alone or in combination with postural deformities5. In a study which included 164 PD patients; 55 (33.5%) had some type of deformities6 (Table II). This study also included 19 patients with MSA and 19 PSP patients where 13 (68.4%) and five (26.3%) patients, respectively had any of the deformities. This study highlighted that approximately one third of the PD patients had some type of limb deformities which was a significant number and contrary to the belief that these are only common in MSA and PSP patients.
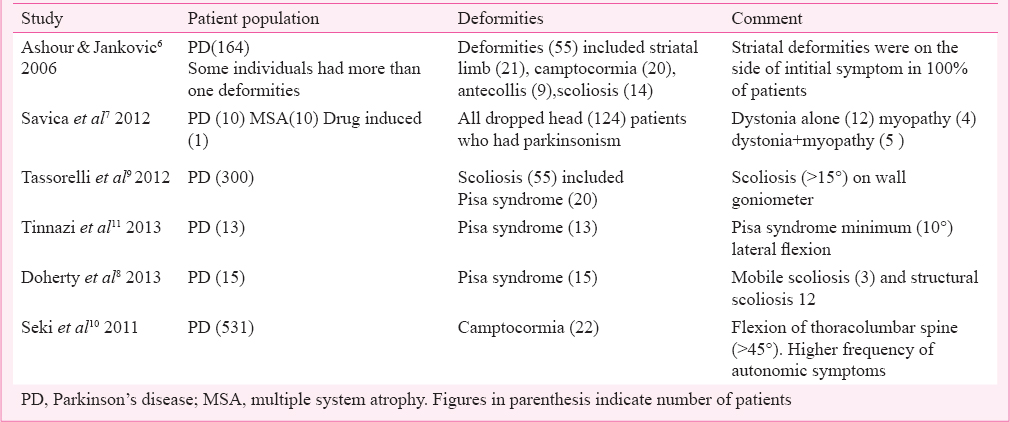
Antecollis and dropped head
In a PD patient there may be forward flexion of neck and head which is known as antecollis. When this forward flexion is severe and chin of the patient is bent down upon sternum it is called dropped head. Commonest symptom because of antecollis and dropped head is neck pain and occasional swallowing difficulties. It is important to do detailed neurological examination to rule out neuromuscular weakness like polymyositis and myasthenia gravis. Suscpicion should be stronger if there is extreme degree of neck extensor weakness. Many PD patients show fluctuation in symptoms with dopaminergic medications. It is important to rule out role of DOPA agonists which may lead to neck drop in some paients. Antecollis and neck drop have been reported in 5-9 per cent of patients in different stuidies1213. In a study which inculded 124 cases of dropped head syndrome, 21 patients had parkinsonism symtoms which included 10 patients of Parkinson's disease7. Dystonia was also present in 12 patients, four had myopathy and five patients had dystonia and myopathy7.
Pisa syndrome
Pisa syndrome (PS) is defined as lateral flexion of the trunk which may also have rotation of the spine which completely subsides in supine positioning. This syndrome is seen commonly in patients on antipsychotic therapy and has also been described in MSA and Alzheimer's disease. It is not clear why some PD patients develop this syndrome. Diagnostic criteria and definition lack consensus leading to a high variability in reported prevalence ranging from 2 to 90 per cent14. A small group of patients may show response in symptoms of PS following levodopa treatment3. In a study from Italy which included 1400 parkinsonism patients, PS was found in 2 per cent cases15. The criteria for diagnosis of PS was lateral flexion (≥15° measured on wall goniometer) which increased during walking and disappeared in the recumbent position. In a study 15 PD patients fulfilled the diagnostic criteria for PS but all had radiological evidence of scoliosis8. Clinically, three had mobile scoliosis and 12 had structural scoliosis which persisted in the supine position (Table II). In another study, it was highlighted that the majority of patients with PS, trunk bending was contralateral to the side of symptom onset and paravertebral thoracic muscles and abdominal oblique muscles had abnormal tonic hyperactivity on the side of the deviation9.
Scoliosis
Scoliosis is defined as lateral flexion of the spine which does not subside by passive movement and has radiological evidence of rotation of vertebra. The available studies have found much variation in prevalence of scoliosis ranging from 9 to 91 per cent616. In a study scoliosis was seen in only 9 per cent of PD patients assessed by clinical examination6. In another study, 19 patients among 21 consecutive patients of parkinsonism (17 PD, 4 postencephalitic parkinsonism) detected by clinical examination had scoliosis16. But in a different study where scoliosis was measured by Cobb's method considering ≥10° as significant lateral flexion, scoliosis was found in 33 per cent PD patients17. It was also documented that the prevalence of scoliosis among healthy elderly patients varied from 6 to 30 per cent, but this figure ranged from 43 to 90 per cent in PD patients17. Scoliosis is usually contralateral to the initial side of symptoms. This happens due to gradual deviation of spine away from the initial affected side due to cholinergically mediated tonic influences on posture and locomotion by caudate nucleus.
Camptocormia
The earliest description of camptocormia was given by Broadie in 181818. Different criteria have been used for the diagnosis of camptocormia but most of the authors have considered flexion (>45°) at thoracolumbar joint while walking or standing and subsiding in lying down position36. The commonest symptoms of camptocormia is back pain which aggravates on walking or standing position. Prevalence of camptocormia among PD patients have ranged from 3-17.6 per cent6192021. In a study of camptocormia patients, 68.8 per cent had a diagnosis of PD22. It has been seen that camptocormia is positively associated with disease severity and duration with average duration being 7-8 yr. In a recent study of 531 PD patients from Japan 22 had camptocormia which was associated with disease severity, higher L- DOPA usage and autonomic symptoms such as constipation and urinary frequency (Table II)10. PD patients with camptocormia should be investigated with radiography and associated degenerative spondyloarthropathy should be ruled out if there is fixed deformity.
Striatal hand and striatal toe (Figs 2 and 3)

- Striatal deformity of left hand characterized by flexion at metacarpophalangeal joint in a Parkinson's disease patient (71 yr old male).

- Striatal deformity of left foot characterized by big toe lateral flexion in a Parkinson's disease patient (66 yr old female).
Striatal hand deofrmities include flexion at metacarpophalangeal, proximal interphalengeal and distal interphalangeal joints. Striatal foot deformities are characterized by extension of great toe and plantar flexion of other toes. There may be associated claw like or talipes equinovarus like deformities. Intitially these deformities may be non-fixed but later on these become fixed. Striatal deformities might be present in up to 10 per cent of untreated cases of advanced PD and these are more common in early onset or younger PD patients (PARKIN mutation)23. These deformities may be responsive to levodopa and may be a part of wearing off dystonia. Misdiagnosis of these deformities as rheumatoid or some other types of arthritis is very common.
Pathogenesis
Pathogenesis of postural and striatal deformities in Parkinson's disease is a combination of ongoing parkinsonian symptoms (rigidity and slowness), dystonia, musculoskeletal changes, loss of postural reflexes and influence of dopaminergic medications (Fig. 4). Duration of disease, amount of rigidity, female sex (possibly due to role of oestrogen) and family history of PD have been considered as important risk factors6. It has been found that PD patients on DOPA agonist develop contracture earlier24. It is not clear whether treatment with levodopa has any role in the pathogenesis or not. Dystonic complication may be due to an imbalance between decrease in dopaminergic level and increase in GABAergic level25. Animal models have helped to understand the pathogenesis. In monkeys where parkinsonism was induced by MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) foot dystonia was reported similar to PD patients26. In a mouse model abnormal posturing was induced by 6-OHDA (hydroxydopamine) injection in the sensorimotor striatum27.
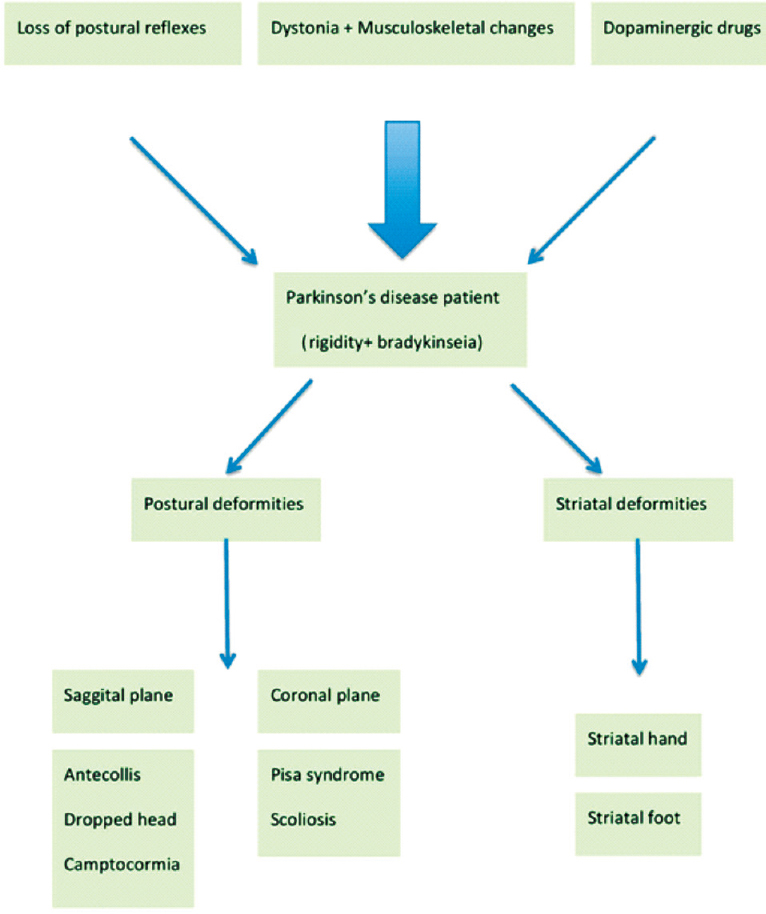
- Pathogenesis and spectrum of postural and striatal deformities in Parkinson's disease.
Treatment
Every PD patient presenting with postural and striatal deformities should be evalauted regarding duration of symptoms, current dopaminergic medications and extent of disability. Important modalities of treatment are modification in dopaminergic drugs, anticholinergic agents, botulinum toxin, neurosurgery, orthopaedic surgery, non-surgical corrections and physical-occupational therapy.
Antiparkinsonian drugs: Postural and striatal deformities are harbinger of advanced PD, but sometimes these can occur in early stage also. DOPA agonists should be avoided and adjustment in other dopaminergic medications may be helpful67. Camptocormia is considered unresponsive to levodopa. Only a few reports of antecollis improving by levodopa are available, but results are not consistent36. Anticholinergics can be used to control dystonic component leading to postural deformity (Pisa syndrome, scoliosis, and striatal deformity). Beclofen and benzodiazepines have also been found to be useful for striatal hand and foot dystonia4.
Botulinum toxin: Botulinum toxin acts by producing chemodenervation and local paralysis in the injected muscle due to presynaptic neuromuscular junction defect. This is helpful in alleviating dystonia which is an important component of postural and striatal deformity. Dosages and location of botulinum toxin injection is better guided by use of electromyography and ultrasound technique. Paraspinal, rectus abdominis and iliopsoas muscles are usually injected for camptocormia. In Pisa syndrome paraspinal muscles and in antecollis neck muscles are site of injections. For striatal hand deformity injections in finger flexors and lumbricals have been found to be quite effective4. In a study on 14 patients of dystonic clenched fist which included seven PD patients who were treated with botulinum toxin injection, all had significant improvement in pain and muscle relaxation leading to better quality in life28.
Neurosurgery: Bilateral deep brain stimulation (DBS) has been used for management of camptocormia, antecollis and Pisa syndrome. Initial cases included PD patients with camptocormia who had globus pallitus internus (GPi) and subthalamic nucleus (STN) stimulation. Postural abnormality is improved due to improvement in dystonia and rigidity of paraspinal muscles29. In another study seven patients (3 dystonia, 3 PD and 1 dystonia and myopathy) having camptocormia underwent DBS surgery30. Two PD patients had bilateral STN DBS and one had GPiDBS and all three had 55 per cent improvement in their off/on unified Parkinson's disease rating scale (UPDRS) in a mean follow up of 21 months (range, 12-36 months). Zona incerta and pedunculopontine nucleus are being explored as an alternative target for postural deformities. Combination of PPN and standard target such as STN may be another option31.
Orthopaedic surgery and non-surgical intervention: Different types of surgical corrections have been tried in striatal and postural deformities in Parkinson's disease. Spinal corrective surgery is helpful in camptocormia and Pisa syndrome. In a study two patients who had PD with severe camptocormia showed significant benefit with surgery32. On the contrary, in a case series of PD patients undergoing spine surgeries 86 per cent had a need for revision surgeries following the first procedure33. Spinal braces and neck collar may be helpful for camptocormia and antecollis. Tendon transfer and Z-lenghtning procedure may be helpful in striatal deformities not responding to dopaminergic medications4. Rehabillitation is another integral part of management of PD patients with postural and striatal deformities. Lating postures applied on shoulders and passive relaxation is helpful in reducing scoliosis34.
Ongoing research
Most of the ongoing research on postural and striatal deformities in PD are related to pathogenesis and treatment. Newer development in neuroimaging has helped in better understanding of pathogenesis of paraspinal and non-paraspinal muscles35. Treatment related research is primarily related to deep brain stimulation surgery and repetitive trans-spinal magnetic stimulation (r-TSMS) which have been found to be effective in treatment of camptocormia in PD patients11. Another ongoing investigation in the management of camptocormia is lidocaine which can be injected ultrasound guided in the abdominal external oblique muscles36.
Conclusion
Postural and striatal deformities are common in PD patients but these are under-reported. These deformities lead to increased incidence of unsteadiness and falls in these patients. Younger age of onset and duration of symptoms are most important risk factors. Early diagnosis and treatment is important as majority may respond to adjustment in dopaminergic medications. Other patients will require botulinum toxin injection, deep brain stimulation, orthopaedic surgical interventions and rehabilitative therapies.
References
- An essay on the shaking palsy. 1817. J Neuropsychiatry Clin Neurosci. 2002;14:223-36.
- [Google Scholar]
- Lectures on the diseases of the nervous system, lecture V. London: New Sydenham Society; 1877. p. :140-7.
- [Google Scholar]
- Striatal deformities of the hand and foot in Parkinson's disease. Lancet Neurol. 2005;4:423-31.
- [Google Scholar]
- Concomitant appearance of Pisa syndrome and striatal hand in Parkinson's disease. J Mov Disord. 2011;4:78-9.
- [Google Scholar]
- Joint and skeletal deformities in Parkinson's disease, multiple system atrophy, and progressive supranuclear palsy. Mov Disord. 2006;21:1856-63.
- [Google Scholar]
- Parkinsonism and dropped head: dystonia, myopathy or both? Parkinsonism Relat Disord. 2012;18:30-4.
- [Google Scholar]
- Pisa syndrome in Parkinson's disease: a mobile or fixed deformity? J Neurol Neurosurg. 2013;84:1400-3.
- [Google Scholar]
- Pisa syndrome in Parkinson's disease: clinical, electromyographic, and radiological characterization. Mov Disord. 2012;27:227-35.
- [Google Scholar]
- Camptocormia in Japanese patients with Parkinson's disease: a multicenter study. Mov Disord. 2011;26:2567-71.
- [Google Scholar]
- Pisa syndrome in Parkinson's disease: an electrophysiological and imaging study. J Neurol. 2013;260:2138-48.
- [Google Scholar]
- The pathogenesis of Pisa syndrome in Parkinson's disease. Mov Disord. 2014;29:1100-7.
- [Google Scholar]
- Botulinum toxin treatment of lateral axial dystonia in Parkinsonism. Mov Disord. 2007;22:2097-103.
- [Google Scholar]
- Note on the scoliosis of Parkinsonism. J Neurol Neurosurg Psychiatry. 1975;38:787-93.
- [Google Scholar]
- Camptocormia in Parkinson disease: an epidemiological and clinical study. J Neurol Neurosurg Psychiatry. 2009;80:145-8.
- [Google Scholar]
- A specific clinical pattern of camptocormia in Parkinson's disease. J Neurol Neurosurg Psychiatry. 2006;77:1229-34.
- [Google Scholar]
- Camptocormia: pathogenesis, classification, and responseto therapy. Neurology. 2005;65:355-9.
- [Google Scholar]
- Contractures of the extremities in parkinsonian subjects: a report of three cases with a possible association with bromocriptine treatment. Clin Neuropharmacol. 1988;11:268-77.
- [Google Scholar]
- The pharmacology of foot dystonia in parkinsonism. Clin Neuropharmacol. 1987;10:47-56.
- [Google Scholar]
- MPTP induced dystonia and parkinsonism: clues to the pathophysiology of dystonia. Neurology. 1997;49:1432-8.
- [Google Scholar]
- A model of L-DOPA-induced dyskinesia in 6-hydroxydopamine lesioned mice: relation to motor and cellular parameters of nigrostriatal function. Neurobiol Dis. 2004;16:110-23.
- [Google Scholar]
- Treatment of dystonic clenched fist with botulinum toxin. Mov Disord. 2001;16:907-13.
- [Google Scholar]
- Effect of subthalamic deep brain stimulation on postural abnormality in Parkinson disease. J Neurosurg. 2010;112:1283-8.
- [Google Scholar]
- Deep brain stimulation for camptocormia in dystonia and Parkinson's disease. J Neurol. 2011;258:96-103.
- [Google Scholar]
- Bilateral deep brain stimulation of the pedunculopon- tine and subthalamic nuclei in severe Parkinson's disease. Brain. 2007;130:1596-607.
- [Google Scholar]
- Surgical correction of kyphosis in patients with camptocormia due to Parkinson's disease: a retrospective evaluation. J Neurol Neurosurg Psychiatry. 2011;82:364-80.
- [Google Scholar]
- Spinal surgery in patients with Parkinson's disease: construct failure and progressive deformity. Spine. 2004;29:2006-12.
- [Google Scholar]
- The effect of the complex rehabilitation on posture and gait in Parkinson Disease. Neurol Neurochir Pol. 2003;37(Suppl 5):67-81.
- [Google Scholar]
- Immediate effect of spinal magnetic stimulation on camptocormia in Parkinson's disease. J Neurol Neurosurg Psychiatry. 2014;85:221-6.
- [Google Scholar]
- Camptocormia in Parkinson's disease: definition, epidemiology, pathogenesis and treatment modalities. J Neurol Neurosurg Psychiatry. 2016;87:75-85.
- [Google Scholar]






