Translate this page into:
Observation on dengue cases from a virus diagnostic laboratory of a tertiary care hospital in north India
Reprint requests: Prof. Amita Jain, Department of Microbiology, King George's Medical University Lucknow 226 003, Uttar Pradesh, India e-mail: amita602002@gmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
The epidemiology of dengue fever (DF) is complex in the Indian subcontinent as all the four serotypes are circulating. This study reports observations on dengue cases from a virus diagnostic laboratory of a north Indian tertiary care hospital catering to areas in and around Lucknow, Uttar Pradesh.
Methods:
Serum samples were obtained from suspected cases of dengue referred to the virus diagnostic laboratory during 2011 to 2013, and detailed history was taken on a pre-structured datasheet. All samples were tested for anti-dengue virus (DV) IgM antibodies and DV-non structural protein 1 antigen (NS1Ag) by ELISA. NS1Ag positive samples were tested further by conventional RT-PCR for DV-RNA detection and serotyping.
Results:
Of the 4019 suspected patients of dengue, 886 (22%) showed laboratory evidence of dengue virus infection. Of these, 19, 17 and 27 per cent were positive in 2011, 2012 and 2013, respectively. Children and adults were similarly affected by dengue in all the three years. Males were more commonly affected than females. The predominant DV serotype detected was DV-2, DV-1 and DV-3 in 2011, 2012 and 2013, respectively. DV-4 serotype was not detected. About half the cases positive for DV infection, showed symptoms of dengue with warning signs/severe dengue. A distinct seasonality with increase in number of dengue cases in the post monsoon period was seen.
Interpretation & conclusions:
Change in circulating serotype of dengue virus; a distinct adult dengue involvement; and a remarkable number of cases presenting with severe dengue manifestations are the main findings of this study.
Keywords
Annual trend
dengue fever
dengue virus
epidemiology
hospital based
serotypes
Dengue virus (DV) infection is a major public health problem in north India1. During the last several decades, the demographic and clinical features of dengue virus infection have changed rapidly12. Infection with DV causes a spectrum of illness ranging from asymptomatic infection to dengue fever, a self limiting febrile illness, to severe dengue, a clinical syndrome that presents as DHF (dengue haemorrhagic fever) or dengue shock syndrome (DSS)3.Dengue virus is an enveloped, single-stranded, positive sense RNA virus belonging to the genus Flavivirus in family Flaviviridae. Four serotypes (DV1-4) of DV are known4.
In India, dengue fever was first reported in 19465. Thereafter, after a gap of 18 years, the first confirmed epidemic was reported from the Eastern Coast of India in 1963-19645. The disease spread northwards and reached Delhi and Uttar Pradesh (UP) during 1967 and 1968, respectively67. At the same time, it also became prevalent in the southern part of the country8 and gradually the whole country was involved with extensive epidemics followed by endemic/hyperendemic prevalence country-wide5.
The epidemiology of dengue circulation is changing in UP, with increased frequency of outbreaks, besides the establishment of dengue as an endemic disease in this region12. This study was undertaken to characterize the circulating serotypes of dengue virus and to report observations on dengue cases during 2011-2013, as analyzed by a virus diagnostic laboratory of a tertiary care hospital in north India catering predominantly to areas in and around Lucknow, UP.
Material & Methods
This study was conducted in a Grade 1 virus diagnostic laboratory, established at King George's Medical University (KGMU), Lucknow, UP. In the laboratory, clinical data sheets of all the patients were filled by a physician on duty, before accepting the sample for testing. Consecutive paediatric and adult patients of either sex, clinically suspected to have dengue infection and referred to the virology laboratory for establishing the diagnosis were enrolled in the study over a three year period (January 2011 - December 2013). History was taken to elucidate fever, nausea, vomiting, rash, aches and pains, abdominal pain or tenderness, bleeding from any site, lethargy, restlessness, impaired consciousness or respiratory distress. Cases showing laboratory evidence of DV infection were classified into the following three categories as per the WHO classification3: severe dengue, dengue with warning signs and dengue without warning signs. A case was defined as probable dengue if along with fever any two of the following were present: nausea/vomiting, rash, aches/pains, positive tourniquet test, or leucopenia. Dengue with warning signs was defined as presence of abdominal pain/tenderness, persistent vomiting, clinical fluid accumulation, mucosal bleed, lethargy/restlessness, liver enlargement >2cm, or increase in haematocrit concurrent with a rapid decrease in platelet count. Severe dengue was defined as presence of either severe plasma leakage, or severe bleeding or severe organ involvement. The cases positive for DV infection were followed up to a period of seven days/discharge from the hospital (whichever was later) to know the course of disease, though the final outcome could not be noted in most of the cases.
Serum sample was collected from all patients. These samples were tested by ELISA for DV specific IgM antibody (Arbovirus diagnostics, National Institute of Virology, Pune, India) and for DV-non structural protein1 antigen (NS1Ag) (J. Mitra and Co. Pvt. Ltd., India) according to manufacturers’ protocols. The remaining serum sample was stored at -80°C. All samples testing positive for DV-NS1Ag, were tested by reverse transcription-PCR (RT-PCR) for serotyping of DV9. RNA was extracted from 250 μl of serum sample by using Trizol reagent (Ambion/RNA Life Technologies, USA) as per manufacturer's protocol. Extracted RNA was used for RT-PCR immediately. For RT-PCR, extracted viral nucleic acid was reverse transcribed to cDNA and then amplified according to the protocol described by Lanciotti et al9. The final amplified product was of 511bp. Only those samples which showed the desirable band of 511 bp on first round were taken for second round of amplification for serotyping. For serotyping a semi-nested PCR was carried out with the DV detection forward primer and four dengue serotype-specific reverse primers targeting C-prM gene junction as per protocol described by Lanciotti et al9. The identification was done by size of DNA bands: DV-1 (482bp), DV-2 (119bp), DV-3 (290bp) and DV- 4 (392bp). The ethical approval for the study was given by the institutional ethics committee and all the patients or their guardians (in case of children and unconscious adults) provided informed written consent.
Statistical analysis: Statistical Package for GraphPad Prism version 5.0 (Graph Pad Software, USA) was used for data entry, processing and statistical analysis. Descriptive statistics were used to calculate all the relevant variables.
Results
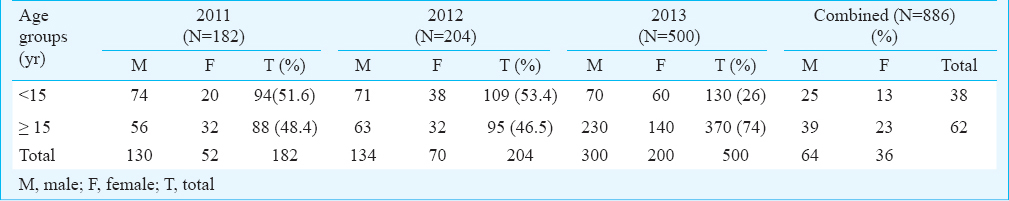
Over a period of three years, from January 2011 to December 2013, a total of 4019 patients suspected to have dengue virus infection were referred to the virology laboratory for confirmation of diagnosis, of whom 945, 1219 and 1855 patients were enrolled in 2011, 2012 and 2013, respectively. Eight hundred eighty six (22%) patients showed laboratory evidence of DV infection, of whom 19, 17 and 27 per cent cases were positive in 2011, 2012 and 2013, respectively (Table I). Of the total DV positive patients, 17 per cent (n=148), 29 per cent (n=257) and 54 per cent (n=481) presented as severe dengue, dengue with warning signs and dengue without warning signs, respectively (Table I). Approximately half the patients (45.7%) infected with DV, developed either warning signs or severe dengue during their course of infection.

The demographic characteristics of dengue (anti-DV IgM or DV-NS1Ag) positive patients are shown in Table II. A high percentage (>46%) of all dengue positive patients was adults (≥ 15 yr). Overall, twice as many males were affected compared to females.
Total 263, DV-NS1Ag and/or anti-DV IgM positive samples were subjected to RT-PCR, of which 103 were tested positive for DV-RNA. Of these, 12 (12.4%) were positive for anti-DV IgM also, while of the 160 DV-RNA negative and DV-NS1Ag positive samples, 49 (30.6%) were positive for anti-DV IgM. Only 103 RT-PCR positive samples were processed for serotyping, of which 39 (37.9%), 26 (25.2%) and 38 (36.9%) samples were positive for DV-1, DV-2 and DV-3, respectively (Table III). DV-2 was the predominant serotype in 2011 while DV-1 became predominant serotype in 2012. DV-3 was not found in 2011, appeared in 2012 and became the predominant serotype in 2013. DV- 4 serotype was not detected in any of the samples.

Seasonal distribution of dengue positive cases is shown in the Figure. A distinct rise in the number of dengue positive cases was seen between August to December.
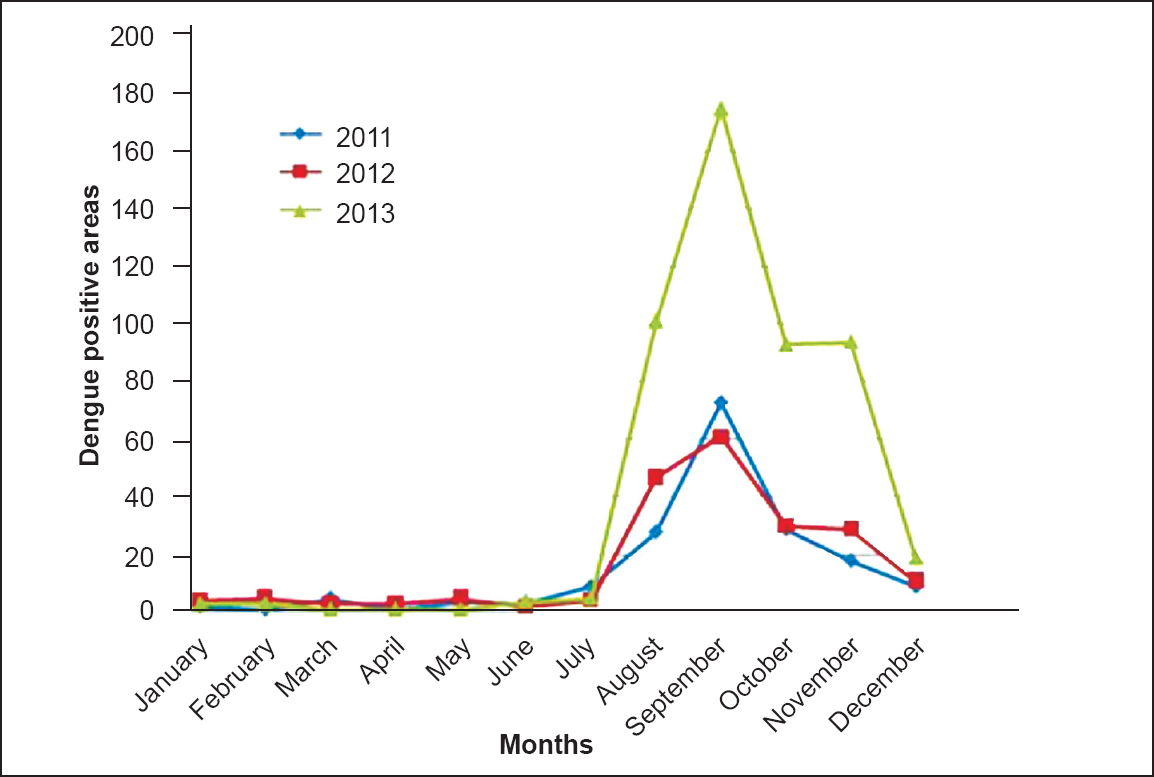
- Seasonal distribution of dengue cases over a three year period.
Discussion
Dengue is one of the major re-emerging viral infections; the global incidence of dengue has shown a 30-fold increase over the past 50 years and the disease has become one of the most rapidly spreading mosquito-borne viral diseases10. Several factors like urbanization, transport development, changing habitats and improper water storage practices, which facilitate breeding of Aedes aegypti, contribute to its rapid spread11. The demographic, economic, behavioural and societal factors greatly influence the key epidemiological determinants including host, viral and vector status12.
In the present study, adults and children were similarly affected by dengue. Dengue was typically thought to be a paediatric disease in South-east Asian countries with rare adult clinical cases of dengue fever (DF)11. However, in recent years, an increasing incidence of DV infection was found in the adults. This age shift has been observed in other Asian countries including Singapore, Indonesia, Bangladesh and Thailand where dengue has been epidemic for several years13.
Males were more commonly affected than females in the present study. Another hospital based study from India also suggested a higher male to female ratio in DV infected hospitalized cases14. However, this may represent only those who access the healthcare facilities and may not be applicable to the general population.
All four serotypes of DV are known to be circulating in North India1516. We have earlier reported DV-2, DV-3 and DV-1 to be the dominant circulating serotypes in 2008, 2009 and 2010, respectively1 in the Lucknow region. DV-2, DV-1 and DV-3 were the dominant circulating serotypes in the present study. Similar periodic serotype shift has been seen in Delhi and may contribute to increased severity of dengue cases15.
The present study also demonstrated that number of cases presenting as dengue with warning signs/severe dengue was almost equal to cases presenting as dengue fever without warning signs. A comparison of year 2011-2013 NVBDCP (National Vector Borne Disease Control Programme) data with that of previous years indicated a shift from mild illness towards a more severe manifestation of the disease17, which could be interpreted as an epidemiologic transition pattern and is a sign of hyperendemicity of the dengue virus in UP1819. In addition, genotypic changes in dengue viruses may contribute further to emergence of severe dengue2021.
The modalities available for diagnosis of dengue infection include isolation of the virus, serological tests and molecular methods. The detection of dengue virus genes in serum sample by PCR coincides with the viraemia and the febrile phase of disease22. However, the limitation of this test is that the test remains positive only when the serum is collected from patients during the first five days of symptoms. On the contrary, DV-NS1Ag can be detected upto 18 days post onset of symptoms22. Most of the cases in the present study had post illness day varying from 5-15 days. This might explain the low PCR positivity as compared to NS1Ag positivity in the present study.
In conclusion, involvement of a high proportion of adult population and predominantly male involvement are the main findings of the study. Annual change in the predominant circulating serotype and increase in the number of severe dengue cases were also observed.
Acknowledgment
Authors acknowledge the Indian Council of Medical Research (ICMR), New Delhi, for providing financial support.
Conflicts of Interest: None.
References
- Trend of dengue virus infection at Lucknow, north India (2008- 2010): a hospital based study. Indian J Med Res. 2012;136:862-7.
- [Google Scholar]
- Descriptive epidemiology of dengue transmission in Uttar Pradesh. Indian Pediatr. 2008;45:315-8.
- [Google Scholar]
- World Health Organization (WHO) and the Special Programme for Research and Training in Tropical diseases (TDR) 2009. Dengue: guidelines for diagnosis, treatment, prevention, and control”. Available from: http://whqlibdoc.who.int/publications/2009/9789241547871,eng.pdf
- [Google Scholar]
- An outbreak of dengue fever in rural areas of northern India. J. Commun Dis. 2001;33:274-81.
- [Google Scholar]
- Investigations on an outbreak of dengue in Delhi in 1967. Indian J Med Res. 1969;57:767-74.
- [Google Scholar]
- Virological study of an epidemic of febrile illness with haemorrhagic manifestations at Kanpur, India, during 1968. Bull World Health Organ. 1970;43:289-93.
- [Google Scholar]
- Virological investigations of the 1966 outbreak of dengue type 3 in Vellore, Southern India. Indian J Med Res. 1969;57:1392-401.
- [Google Scholar]
- Rapid detection and typing of dengue viruses from clinical samples by using reverse transcriptase-polymerase chain reaction. J Clin Microbiol. 1992;30:545-51.
- [Google Scholar]
- The changing epidemiology of yellow fever and dengue, 1900 to 2003: full circle? Comp Immunol Microbiol Infect Dis. 2004;27:319-30.
- [Google Scholar]
- Changing epidemiology of dengue in South-East Asia. WHO South-East Asia J Public Health. 2013;2:23-7.
- [Google Scholar]
- Epidemiology of dengue: past, present and future prospects. Clin Epidemiol. 2013;5:299-309.
- [Google Scholar]
- Dengue - changing trends and the need for research. Res J Pharm Biol Chem Sci. 2014;5:144-8.
- [Google Scholar]
- Changing trends of dengue disease: a brief report from a tertiary care hospital in New Delhi. Braz J Infect Dis. 2011;15:184-5.
- [Google Scholar]
- Cocirculation of dengue serotypes, Delhi, India, 2003. Emerg Infect Dis. 2006;12:352-3.
- [Google Scholar]
- Reemergence of dengue virus type-3 (subtype-III) in India: implications for increased incidence of DHF & DSS. Virol J. 2006;6:3-55.
- [Google Scholar]
- Dengue: Dengue cases and deaths in the country since 2009. National Vector Borne Disease Control Programme (NVBDCP), Directorate General of Health Services. Ministry of Health and Family Welfare, Government of India, New Delhi, India. Available from: http://www.nvbdcp.gov.in/dencd.html
- [Google Scholar]
- Clinico-virological study of the recurrence of dengue epidemic with haemorrhagic manifestations at Kanpur during 1969. Indian J Med Res. 1972;60:329-33.
- [Google Scholar]
- The first major outbreak of dengue hemorrhagic fever in Delhi, India. Emerg Infect Dis. 1999;5:589-90.
- [Google Scholar]
- Molecular characterization of dengue viruses circulating during 2009-2012 in Uttar Pradesh, India. J Med Virol. 2015;87:68-75.
- [Google Scholar]
- Epidemiology of dengue in Sri Lanka before and after the emergence of epidemic dengue hemorrhagic fever. Am J Trop Med Hyg. 2002;66:765-73.
- [Google Scholar]
- Centres for Disease Control and Prevention, Dengue, laboratory guidance and diagnostic testing. Available from: http://www.cdc.gov/dengue/clinicalLab/laboratory.html
- [Google Scholar]






