Translate this page into:
Equity in utilization of health care services: Perspective of pregnant women in southern Odisha, India
Reprint requests: Dr Meerambika Mahapatro, National Institute of Health & Family Welfare, Baba Gang Nath Marg, Munirka, New Delhi 110 067, India e-mail: meerambika@rediffmail.com
-
Received: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Inequity in the use of health care services is an important factor affecting the maternal and child survival. In southern Odisha, India, the health indicators remained below compared to the State and national average. This study identifies various equity issues at individual and community levels that influence women's choice affecting the utilization of maternal health services in a district in southern Odisha.
Methods:
A qualitative study was carried out in Gajam district, rural region of south Odisha. Ten in-depth interviews were carried out till data saturation with women having less than one year child and 10 focus group discussions with the average eight women in each group having less than five year old child, community and health care providers separately. A total of 120 respondents were included in the study using in-depth interview and focus group discussions.
Results:
The important determinants in utilization of health care services by women emerging from the study were transportation and financial constraints. In addition, it was found that divergent aetiological concepts and low perceived hospital benefits of the women and community were equally important determinants. Further, community had different perceptions and interpretations of danger signs influencing the risk approach and health care seeking behaviour.
Interpretation & conclusions:
Our findings show that to increase the utilization of health care services, the grass root health workers should be made aware of specific social determinants of risk, perceptions and preferences. More attention should be given to the transportation system, and its operational feasibility. The husband of the women and the elders of the family should be considered as an important unit of interjection. A more individualized antenatal consultation could be provided by taking into account women's perception of risk and their explanatory models.
Keywords
Barriers to utilization
community perception
health care seeking behaviour
health worker
maternal community
maternal health
social and spatial equity
The fundamental principle of equity is equal treatment for all socio-economic groups, as well as gender with equal needs12. Studies have shown two forms of inequity; social inequity is due to poverty, ethnicity, and lack of education while spatial inequity arises due to the place of residence, such as rural, urban, hilly and forest areas, that affect on access to health care3. The measure to gauge equity is to assess distribution of opportunities in health care system suggesting a shift to measure social and spatial barriers of morbidity and mortality, and health seeking behviour can be used as indicators to assess equity1.
Odisha is ranked one of the highest maternal mortality ratio (MMR) of 311 per 100,000 births in India4. Southern Odisha ranks the lowest among the all three divisions of Odisha, with State average of 2774. Although four routine antenatal care (ANC) visits have been advocated for a reduction in perinatal and maternal mortality5 and improve essential obstetric care6, in India about 90 per cent pregnant women receive any antenatal check-up, half of these visits made in the first trimester and only 20 per cent followed for full antenatal check-up7. It has been reported that rural women are nine times more prone to having no prenatal care and four times more prone to have home deliveries than urban women89, and many of these opportunities continue to be missed. Institutional delivery has been seen as an important strategy for preventing maternal and neonatal mortality, but about 47 per cent of births take place at home and, at best, 39 per cent are assisted by trained health professionals47. Though, home deliveries in the absence of skilled professional attendants have been associated with adverse infant and maternal outcome1011, home deliveries are chosen or occur for a variety of reasons1213.
Inequity of maternal mortality remained high in sourthern Odisha47. Several previous studies have examined the factors contributing to poor maternal and child health outcome and access to care in northern India141516. High parity, low income and socio-economic status, belonging to a minority ethnic group, low level of education, young maternal age, preferences for traditional medicine, and lack of awareness of the need for routine care visit and institutional delivery are some of the important factors17181920. Little attention has been given to the wide gap in the perception regarding obstetric services between women and the influence of local perceptions of danger signs and their interpretation21 results in preferences for place of delivery. It is difficult to judge the extent to which the fear of rural women and vulnerability of receiving treatment at the hospital setting is based on experience. To strengthen maternal health components, the National Rural Health Mission (NRHM) was introduced in 2005 to increase coverage and quality, for safe motherhood under wider network of human resources to reach the rural population22.
Antenatal and essential obstetric care services are key features of health interventions for reducing maternal and newborn morbidity and mortality. There are limited studies on procedural constraints in implementation and inadequate feedback from the community with respect to identify the underlying reasons for accepting or rejecting maternal and child health (MCH) care and patterns of care-seeking behaviour and health care utilization23. Against such a setting, there is a need to explore how the health care system is used to adapt to the ongoing changes in society. In Odisha, though the State government has taken many initiatives to converge health activities at district and subsequent levels, this problem is difficult to address and making safe motherhood a reality for women is a challenge. Therefore, in this study an attempt has been made to develop a framework of barriers arising out of inequitable heath services at social and spatial level; and understand community perceptions that influence women's health seeking behaviour and utilization of MCH care in a district of Odisha, India.
Material & Methods
Area/setting and study population: A qualitative study was carried out in Ganjam district rural region in Odisha during 2011-2012. Ganjam district was selected based on poor MCH indicators such as infant and maternal mortality rates (IMR, MMR) and low institutional deliveries. Two Health Sub-Centre (HSC) villages near to the medical college, i.e. Phulta and Nua Khejuria, were purposely selected. As per the inclusion criteria pregnant women, women delivered in the last one year and women with 5 yr old child, health professionals, service providers, and key influencers, were eligible. With the help of the medical records maintained by auxiliary nurse midwife (ANM) and accredited social health activist (ASHA), at the HSC, the women participants were invited to participate in the study. A total of 120 respondents were included in the study using indepth interview and focus group discussion.
Data collection: Using participatory method, transact walk was conducted in the village with the health professionals for functional health services resource mapping. Interviews with pregnant women were held after obtaining written consent, focused on: (i) the women's perception about barriers to using obstetric care, (ii) the underlying reasons for unfavourable pregnancy outcomes of women and treatment options, and (iii) women's perception of a set of professionally defined risk factors. Interviews with health workers and key-informants probed their understanding of risk factors and their notion of barriers to pregnant women for use of village health care.
Pre-tested semi-structured interview schedule was used for indepth interview. Ten in-depth interviews (IDIs) with the study participants led to data collection. All these interviews were recorded in Oriya language and later translated into English. All IDIs and focus group discussions (FGDs) were recorded with consent from respondents and transcribed. Six FGDs with an average of eight women in each group were conducted with women who delivered in last five years; two FGD with ASHA/ANM/anganwadi worker (AWW) and two FGD with Mahila Mandals and key influencers were carried out. Five key informant interviews (KII) with the key influencers and ten interviews with the service providers/implementers were carried out.
Data analysis: The data collected in the form of recorded interviews were transcribed with the help of field notes24. Transcripts of the interviews and FGDs with mothers, health workers, and key informants were reviewed. Latent thematic content analysis was done in the following ways. As the first step, the data were reviewed and transcripts were re-read to identify important themes. Then the patterns, possible relationships between themes, contradictory responses were identified. The statements in the interviews were categorized and analysed according to frequency in general, frequency in each different group of interview, controversial discussion of the statement and emotional involvement of the interview participants. Typical statements were marked and used for later citation. Analysis, interpretation and conclusions were carefully drawn describing the research context and the characteristics of the study participants.
The written consent of the participants was taken and the study protocol was approved from Institutional Review Board, National Institute of Health and Family Welfare (NIHFW), New Delhi.
Results
Social, and spatial inequity:
(i) Geographical accessibility and transportation - All informants unanimously mentioned geographical accessibility and transportation as the main obstacle for using healthcare facilities. Only about 30 per cent (n=96) of women used Janani Express (JE) facility under Janani Suraksha Yojna (JSY). About 48 per cent (n=151) of women used private vehicle mostly auto rickshaw for institutional delivery expressed inability to avail JE on time. Apart from risk due to lack of smooth transportation by auto, 60 per cent of the users lost one hour to 30 min in arranging a vehicle.
The transport situation was perceived difficult by every woman. There was no public transport system linked with the hospital. The single vehicle JE, was stationed at the community health centre (CHC), 17 km away from the village. Due to distance and lack of efficient system for the villagers to get the access to the vehicle, and untimely demand resulted in poor utilization of JE. During this fieldwork, the vehicle was sometimes not found functional. The situation was even worse if childbirth took place at night. The community also pointed out the high transportation cost.
(ii) Traditional family structures - About 70 per cent households were joint family structures. Unlike nuclear family, joint family decision making is collective and not independent. However, the decision was mostly swayed by the financial capacity of the joint family. During the time of delivery, the decision-makers were the elders and not the women. In such a situation, if ASHA/ANM interaction was limited to the women, knowledge transfer from women to elders was not effective.
(iii) Perception of care - The finding of the FGD indicated that the difference in the perception of hospital care depended on doctors’ differential treatment on the basis of socio-economic backgrounds of the families. The differentiation was less and community perception was homogenously positive towards ANC care. But, the people were more critical about hospital care during the time of delivery as perception varied with the perceived gap between the doctors response to the seriousness. The frequently raised issues in FGD were lack of facilities as barrier regarding operation, hospital discriminatory culture against rural poor, and lack of timely availability of drugs and attitude of health care providers, raising negative emotions.
The health workers’ attitudes, bad language, feeling of being neglected and unwelcome were mentioned as reasons for non-compliance. They also felt that the health workers at the hospital were biased against poor rural illiterate women and preferential treatment was given to people with higher social and economic status, either due to their higher castes or ability to pay. All respondents complained about the non-availability of drugs and long waiting times for the rural poor and gender insensitive system.
There was a fear of hospital environment and caesarean sections in the respondents. The reasons highlighted were unfamiliar surroundings, lack of ability to mobilize social support, fear of sudden medical complications, fear of not able to comprehend the doctor's recommendation, and fear of relatives not being beside the woman inside the operation theater. There was also the perception that caesarean sections were unnecessarily performed in the hospital. The FGD supported the findings that caesarean sections led to more threat to the women life who was more safe in home delivery.
(iv) ASHA's caste and knowledge - Multi-caste villages have male dominated and caste stratified system. In the villages during the daily interaction ASHA was categorized more by her caste than her abilities to provide health care services. The status of health providers in the hospital was higher than health workers in the village. Despite direct contact with the community, the low status of ANM and ASHA the in the health care system was reflected in the acceptability and recognition.
A perception based framework of barriers: The community perception is an outcome of repeated experience based on inequity. Seldom clinical experts knowledge and services and community perception are compatible. Thus clinical risk factor does not automatically imply complimentary community perception and practice. Based on this observation, a model was developed (Table) on the relation between clinical risk factors and perceived danger signs by the women. This model comprises three levels/stages of agreement. It illustrates how differences in the perception of risk factors and their causes can lead to diversity of health care-seeking behaviour in the community.
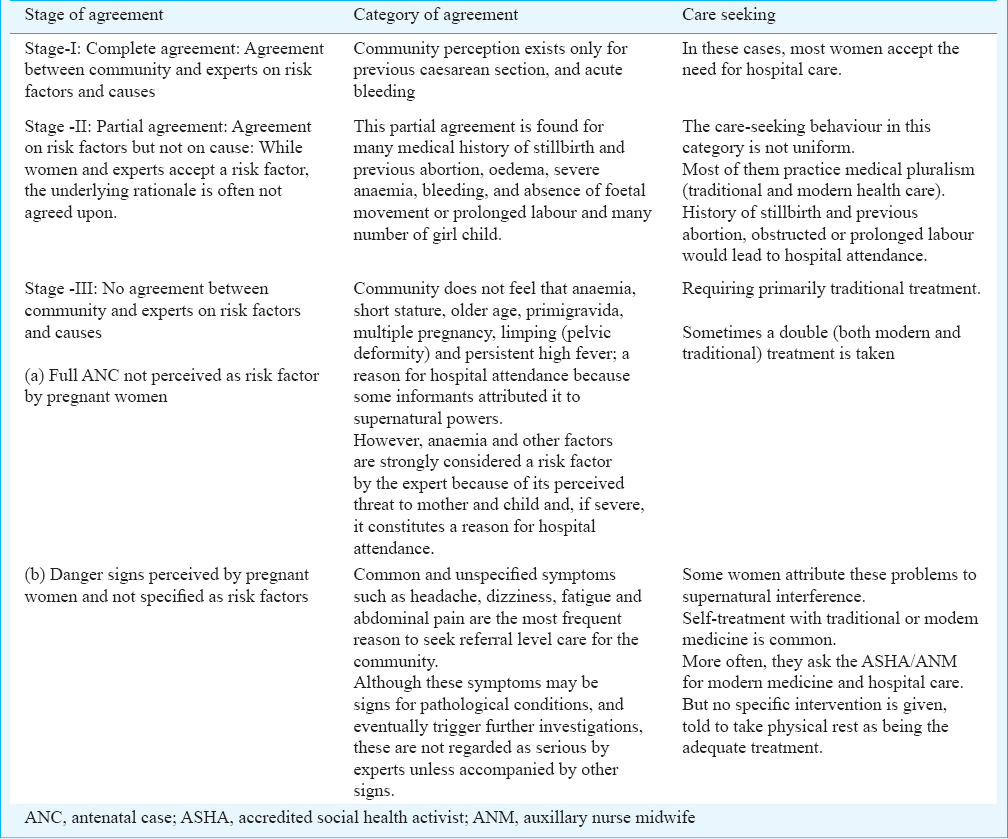
(i) Stage-1: Complete agreement on risk factors and causes: Such agreement between the community and experts on risk factors and the aetiology exists only for cases of previous caesarean sections and acute bleeding. In these cases, most women accept the need for hospital care.
(ii) Stage-2: Partial agreement on risk factors but not on causes: While women and experts accept a risk factor, the underlying rationale is often not agreed upon. This partial agreement is found for many medical histories such as stillbirths and abortions, oedema, severe anaemia, and absence of foetal movement. The care-seeking behaviour in this category is not uniform. Emergencies like obstructed or prolonged labour lead to hospital attendance. Others are seen as potential dangers, but as these are often attributed to supernatural causes, traditional treatment is frequent. Although anaemia is strongly feared because of its perceived threat to mother and child and, if severe, constitutes a reason for hospital attendance, for women, anaemia is not a straightforward reason for hospital treatment and is mostly attributed to supernatural causes requiring primarily traditional treatment.
(iii) Stage-3: No agreement on risk factors and causes: Some danger signs perceived by women are not considered risk factors by health care providers. These include common and unspecified symptoms such as headache, dizziness, fatigue, and abdominal pain. These top the list of perceived danger signs, and the most frequent reasons to seek referral-level care. Lack of response by ASHA/ANM to the perceived risk of the women was seen as one of the main reasons for low utilization of health care services. The most frequent response to the presence of pregnancy-related risks is primarily the perception of a supernatural aetiology leading to traditional treatment, double treatment (modern and traditional), self-treatment, and no treatment at all.
Discussion
This study found that social and spatial inequity influenced health care seeking behaviour and utilization of maternal health services in the study area. The important barriers emerging from the study were transportation and financial constraints which were also evidenced in the research carried out in India, Tanzania, and Afghanistan252627. In addition, it was found that divergent aetiological concepts and perceived hospital culture and care were equally important determinants to control maternal health care seeking behaviour in Ganjam district, Odisha, as has been shown in other Indian StatesStates28. The community members were not convinced with the impact of antenatal care in reducing the risk, as even without ANC, a woman was able to deliver normally. The study showed that the perceived attitudes of women towards supernatural healing further reduced their readiness to seek care at the health-facility level. A risk approach, solely based on epidemiologically defined risk factors without consideration of women's perception (local community), does not benefit at-risk mothers. A traditional concept dominates whenever recurrence of complications of previous pregnancies is possible. Women know about the danger of recurrence, but they regard treatment by traditional healers as appropriate action. This may explain the low perceived risk in comparison to actual risk by the women and community at large29.
The results also indicate that in the traditional family, decision-making for ANC or institutional delivery lies with the mother and elders of the family. The current health practices allows ASHA/ANM to interact with the pregnant women in the village30 that do not transform the choice of the elders, and knowledge transfer is not effective for deciding utilization of MCH services. The health care provider and women have different perspectives about hospital care during the time of delivery31. The discrepancies between the provider's and the community's perspectives and social realities create predicament at the very core of diffusion, acceptability, and utilization of health care services32. To improve institutional access, it is important to internalize these as barriers and develop a strategy towards overcoming these33.
The limitation of the study was that the selected respondents who had recently given birth were encouraged to give their actual experiences.
Respondents probably gave us general attitudes prevalent in the communities. Another possible limitation was that the study focused on MCH care practices and did not target health care issues other than when these were thought to impact the mother and newborn.
As a first step to increase the acceptability of hospital care to rural women, health workers should be aware of their specific social determinants of risks. The minor influence of clinical risk status on the actual use of hospital-level care found in Ganjam highlights a general problem of the risk approach in antenatal and natal care. Much more attention should be given to the transportation system, and its operational feasibility. The study emphasises on lack of orientation towards the community's perceptions and preferences. The identification of overlapping areas between experts and community perception of health needs is important, because interventions in the overlapping areas are much more likely to be accepted and succeed. The ANM/ASHA strategy is to sensitize women to create awareness. But to convert knowledge into decision, the husband and the elders of the family should be considered as an important unit of interjection. It is also important for maternal health programmes to engage community to advocate success of institutional delivery and simultaneously reduce misconceptions, to enable pregnant women for appropriate care-seeking behaviour.
Acknowledgment
Author acknowledges the contribution of the Director, National Institute of Health and Family Welfare (NIHFW), Prof. R.M. Tripathy and his team at the Berhampur Medical College, Berhampur, Ganjam and thanks to participants at the Annual Global Health Conference, Singapore, on the basis of which the earlier draft of this paper was extensively revised.
Conflicts of Interest: None.
References
- Determinants of equity in utilization of maternal health services in Butajira, Southern Ethiopia. Ethiop J Health Dev. 2012;26:265-70.
- [Google Scholar]
- Equity in use of maternal health services in western rural China: a survey from Shaanxi province. BMC Health Ser Res. 2014;14:3-8.
- [Google Scholar]
- Mortality determinants in Zimbabwe: A policy implications. Mimeo: University of Zimbabwe, Sociology Department; 1994.
- [Google Scholar]
- Annual health survey, second reound updation 2012-13. New Delhi: Office of the Registrar General and Census of India. Government of India; 2013.
- [Google Scholar]
- World Health Organisation (WHO). The world health report - make every mother and child count. Geneva: WHO; 2005.
- [Google Scholar]
- World Health Organization (WHO). Pregnancy, childbirth, postpartum and newborn care: a guide for essential practice. Geneva: WHO; 2003.
- [Google Scholar]
- Annual health survey 2010-11. New Delhi: Office of the Registrar General and Census of India. Government of India; 2013.
- [Google Scholar]
- Barriers to the utilization of maternal health care in rural Mali. Soc Sci Med. 2007;65:1666-82.
- [Google Scholar]
- Antenatal care: provision and inequality in rural north India. Soc Sci Med. 2004;59:1147-58.
- [Google Scholar]
- Family planning clinics through women's eyes and voices: a case study from rural Bangladesh. Int Fam Plan Perspect. 1998;24:170-5.
- [Google Scholar]
- Variation in prenatal care quality for the rural poor in Mexico. Health Aff. 2007;26:310-23.
- [Google Scholar]
- International Institute for Population Sciences (IIPS). National Family Health Survey (NFHS-2) 1998-99; India. Mumbai: IIPS; 2000.
- [Google Scholar]
- Applying a framework for assessing the quality of maternal health services in urban India. Soc Sci Med. 2007;64:2083-95.
- [Google Scholar]
- Contextual influences on reproductive health service use in Uttar Pradesh, India. Stud Fam Plann. 2002;33:309-20.
- [Google Scholar]
- Contextual influences on reproductive wellness in Northern India. Am J Public Health. 2003;93:1820-9.
- [Google Scholar]
- Does the safe-motherhood programme reach the poor in Uttar Pradesh, India? Asian Popul Stud. 2010;6:173-91.
- [Google Scholar]
- Prenatal care use among women of low income: a matter of ‘Taking Care of Self’. Qual Health Res. 2003;13:319-32.
- [Google Scholar]
- Determinants of maternal care in a region of South India. Health Transit Rev. 1995;5:127-42.
- [Google Scholar]
- Utilization of maternal health services in Southern India. Soc Sci Med. 2002;55:1849-69.
- [Google Scholar]
- Is antenatal care effective in improving maternal health in rural Uttar Pradesh? Evidence from a District Level Household Survey. J Biosoc Sci. 2006;38:433-48.
- [Google Scholar]
- Organising delivery care: What works for safe motherhood? Bull World Health Organ. 1999;77:399-406.
- [Google Scholar]
- National Rural Health Mission (NRHM). Meeting people's health needs in rural areas. Framework of implementation 2005 -2012. New Delhi: NRHM, Government of India; 2005.
- [Google Scholar]
- Weighing up and balancing out: a meta-synthesis of barriers to antenatal care for marginalised women in high-income countries. An Int J Obstet Gynaecol. 2009;116:518-29.
- [Google Scholar]
- Qualitative methods in public health- A field guide for applied research. California, USA: Jossey-Bass; 2005.
- [Google Scholar]
- International Institute of Population Sciences (IIPS). District level health survey and facility survey. Mumbai: IIPS; 2009.
- [Google Scholar]
- Use of healthcare services in two rural communities in Tanzania community. Dent Oral Epidemiol. 1993;21:133-5.
- [Google Scholar]
- Raising institutional delivery in war-torn communities: Experience of BRAC in Afghanistan. Asia Pac J Fam Med. 2007;6:2.
- [Google Scholar]
- Impact of health centre availability on utilisation of maternity care and pregnancy outcome in a rural area of Haryana. J Indian Med Assoc. 1997;95:448-50.
- [Google Scholar]
- Assessment of MCH services offered by professional and community health workers in the district of So-lenzo, Burkina Faso I. Utilization of MCH services. J Trop Pediatr. 1989;35:2-9.
- [Google Scholar]
- Promoting institutional deliveries in rural I ndia: The role of antenatal care services. National Family Health Survey Report Number 20. 2001
- [Google Scholar]
- The cutting edge in the blunt space: an anthropological construct of auxiliary nurse midwives’ social world in the community. Health Low-resour Settings. 2013;1:e10.
- [Google Scholar]
- Medical technologies in developing countries: issues of technology development, transfer, diffusion and use. Soc Sci Med. 1989;28:769-81.
- [Google Scholar]
- The strategy of risk approach in antenatal care: evaluation of the referral compliance. Soc Sci Med. 1995;40:529-35.
- [Google Scholar]






