Translate this page into:
Aetiology of childhood viral gastroenteritis in Lucknow, north India
Reprint requests: Dr Amita Jain, Department of Microbiology, King George's Medical University Lucknow 226 003, Uttar Pradesh, India e-mail: amita602002@yahoo.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Due to limited availability of data on viral aetiology of acute gastroenteritis in north India, the present study was planned to detect rotavirus, norovirus, sapovirus and astrovirus in stool samples of both in hospitalized and non-hospitalized children less than five years of age presenting with acute gastroenteritis.
Methods:
A total of 278 stool samples from equal number of children were tested for rotavirus antigen using ELISA and for norovirus, sapovirus and astroviruses by reverse transcription (RT)-PCR.
Results:
Of the 169 samples from hospitalized patients, rotavirus, norovirus, sapovirus and astrovirus were detected in 19.5, 2.3, 3.5 and 2.9 per cent samples, respectively. Of the 109 samples collected from the non-hospitalized patients, frequency of rotavirus and sapovirus detection was 9.1 and 1.8 per cent, respectively while norovirus and astrovirus were not detected.
Interpretation & conclusions:
Rotavirus was the most frequent cause of viral gastroenteritis in both hospitalized and non-hospitalized children. Maximum positivity of the viruses was seen in children less than two years of age.
Keywords
Astrovirus
diarrhoea
norovirus
rotavirus
sapovirus
stool samples
viral gastroenteritis
Acute gastroenteritis is one of the most common childhood diseases, especially in developing countries. Annually 2.5 million deaths are estimated to occur due to enteric infections, greatly impacting children younger than five years of age1. Over 20 different types of viruses have been identified as aetiological agents for gastroenteritis2. Group A rotaviruses are considered to be the main agents followed by calicivirus, adenovirus and astrovirus3. In a corss-sectional study conducted at Lucknow, Uttar Pradesh, India, rotavirus was shown to be associated with dehydrating diarrhoea, particularly in children 0-7 months of age4. Another study conducted in the same city5 also reported rotavirus as a major cause of acute diarrhoea in children aged two months to two years.
This study was performed to detect rotavirus, norovirus, sapovirus and astrovirus in stool samples of both hospitalized and non-hospitalized children, less than five years of age presenting with acute gastroenteritis in Lucknow, north India.
Material & Methods
This cross-sectional study was conducted in the Virology Laboratory, Post Graduate Department of Microbiology, King George's Medical University (KGMU), Lucknow, Uttar Pradesh, India, during August 2010 to July 2012. A total of 278 stool samples from the equal number of consecutive children less than five years of age, presenting with acute gastroenteritis were enrolled. A case of acute gastroenteritis was defined as a child less than five years of age presenting with watery diarrhoea of less than 14 days duration. Written informed consent was obtained from the parents and the study was approved by the ethics committee of the institution. Cases from either paediatric wards/emergency centre of the Gandhi Memorial and associated hospital or Shivgarh area in Lucknow district (non-hospitalized community patients screened through house-to-house survey) were enrolled. Patients presenting with bloody diarrhoea/with diarrhoea of more than 14 days/or parents declining consent were excluded. Relevant clinical data on age, sex, details of diarrhoea, presence of fever, vomiting and clinical signs and symptoms of dehydration were collected from either patient's records or from the patient's attendant.
Stool sample was collected as mentioned in CDC (Centers for Disease Control and Prevention) guidelines6. At least 10 ml of liquid, watery stool and one sample per patient was collected in a clean and dry screw capped, wide mouth plastic container. Samples from the hospital were transported to the laboratory immediately. The samples from the community were transported to the laboratory on the same day maintaining the cold chain.
Samples were processed without delay. ELISA for rotavirus group specific antigen (VP6) detection was done by a commercial kit (RIDASCREEN Rotavirus supplied by R- Biopharm AG, Darmstadt, Germany). One step reverse transcription (RT)-PCR assays for norovirus, sapovirus and astrovirus detection were performed using specific primers789. stool suspension (10%) was prepared in 0.01 M phosphate-buffered saline (PBS) (pH 7.2), vortexed and centrifuged. The supernatant was transferred to a sterile, diethyl pyro-carbonate treated centrifuge tube. RNA extraction was done using a commercial kit (QIAamp viral RNA mini kit, QIAGEN, Gmbh Hilden, Germany) and the extracted RNA was subjected to reverse transcription to form cDNA using random hexamer primer (Amersham-Pharmacia Biotech, USA). Total 35 cycles of amplification were performed and results were analyzed by 1.5 per cent (w/v) agarose gel electrophoresis using molecular weight marker (MBD-13J 100bp DNA ladder, Bangalore, Genei, India) using 264 nm wavelength UV transilluminator and Gel Doc (Alphamager 3400 HP, Alpha Innotech, USA). A band of 329 bp for norovirus, 320 bp for sapovirus and 449 bp for astrovirus of amplified cDNA if visualized along with the band of positive control at the same base pair was considered positive. Positive, negative and extraction controls were run with each batch.
Statistical analysis: chi-square test was applied to find the risk of viral positivity by age of the patients. The relative risk (RR) with its 95% confidence interval (CI) was calculated to find the risk of viral positivity by symptoms. The data analysis was carried out by using EPI INFO Windows version 7 (http://www.cdc.gov/epiinfo)
Results & Discussion
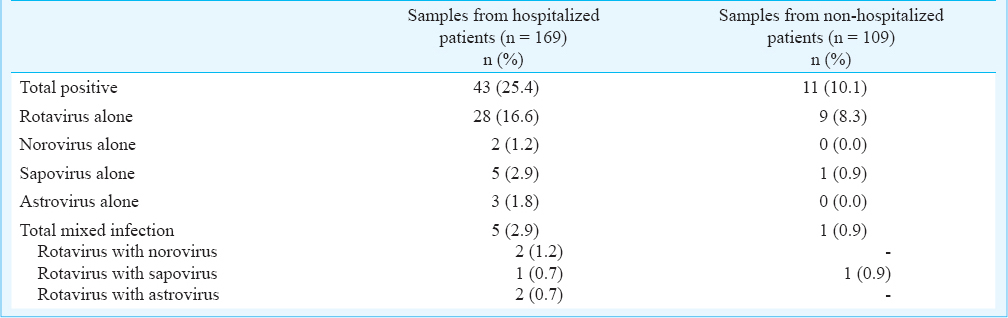
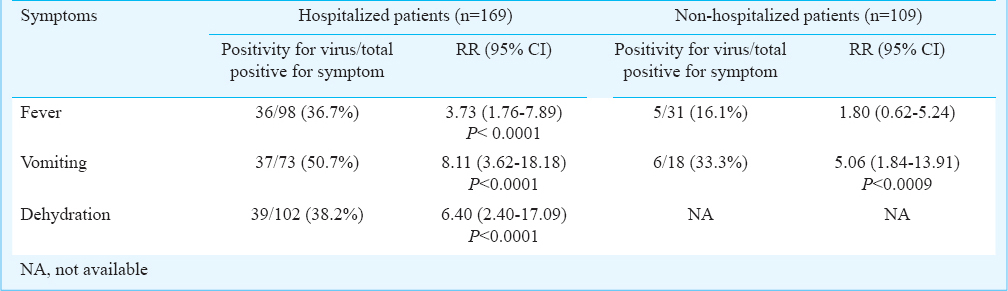
Of the total of 278 patients, 169 (60.8%) were enrolled from hospital and 109 (29.2%) from the community. Of the 278 stools samples, 54 (19.4%) were found positive for the tested viruses. Viral detection was more frequent in hospitalized (n=43, 25.4%) than in non-hospitalized (n=11, 10.1%) children (Table I). The relative risk of viral positivity by symptoms of fever, vomiting and dehydration is shown in Table II. Dehydration could not be properly assessed in non-hospitalized patients, hence, not shown in data.
The viral positivity was higher among hospitalized children less than two years of age (data on age not shown). Overall, the viruses were isolated during the cooler months of year with a peak in month between October and December among hospitalized patients (data not shown). Seasonal distribution among non-hospitalized patients could not be assessed due to small number of samples in each month.
Our study demonstrated that rotavirus was the leading cause of viral gastroenteritis with positivity rate of 16.6 per cent in hospitalized children and 8.3 per cent in non-hospitalized children followed by sapovirus (2.9%), astrovirus (1.8%), norovirus (1.2%) in hospitalized children. The rotavirus positivity in this study was comparable with the previous studies from Lucknow45, although higher rates have been reported from Kolkata (48.1%)10 and Delhi (39.2%)11. In developing countries norovirus is recognised as the second most frequent viral cause of childhood gastroenteritis after rotavirus12. We found a low positivity of norovirus (1.2%), in hospitalized children compared with the other regions like Pune (8.6%), Maharashtra13 and Kolkata (4.8%)10. Sapovirus is known to cause symptomatic infection predominantly in infants and young children8. The detection rate of sapovirus reported from Vellore (5.1%) and Kolkata (2.3%) was similar to that found in our study (2.9%), while Delhi reported it to be 10.1 per cent in hospitalized patients101415 Prevalence of human astrovirus infection ranges from 0.3-10 per cent in children worldwide16. Its positivity in the present study (1.8%) among hospitalized patients was close to that reported from Pune (3.1%) and Kolkata (5.8%)1718. The conditions like season of sampling, socio-economic level of the population may explain differences in the detection rates.
As seen in our study fever, vomiting and dehydration are usually associated features of acute gastroenteritis more so of viral gastroenteritis19. The existence of co-infections makes the determination of the primary aetiologic agent, as well as the determination of virus specific symptoms difficult, however, the mixed infections were low in the present study and rotavirus was always the common detected pathogen.
Diarrhoea causing adenoviruses are known to be associated with gastroenteritis in children19. Diarrhoeal pathogens occur at a high frequency in developing countries thus, may be present in a notable proportion of control subjects as well as patients20. Thus, inclusion of control in diarrhoeal studies play a major role, especially when comparing the relative contribution of different pathogens to the overall burden of disease.
In conclusion, rotavirus was the major viral pathogen in both hospitalized and non-hospitalized children with acute gastroenteritis. Other viruses like norovirus, sapovirus and astrovirus were found to be associated with acute gastroenteritis in a small number of hospitalized children.
Acknowledgment
The author express sincere gratitude to Late Dr G. K. Malik, Professor, PG department of Paediatrics, KGMU, Lucknow, for his guidance and support during the study. Authors thank Dr. Triveni Krishnan, National Institute of Cholera and Enteric Diseases (NICED), Kolkata for providing positive controls for the respective viruses. The financial support received from the Indian Council of Medical Research, New Delhi, is acknowledged also.
References
- A review of vaccine research and development: human enteric infections. Vaccine. 2006;24:2732-50.
- [Google Scholar]
- the AFHSC-GEIS Enteric Surveillance Writing Group. Enteric disease surveillance under teh AFHSC-GEIS: Current efforts, landscape analysis and vision forward. BMC Public Health. 2011;11:572-11.
- [Google Scholar]
- Adenovirus, calicivirus and astrovirus detection in fecal samples of hospitalized children with acute gastroenteritis from Campo Grande, MS, Brazil. Mem Inst Oswaldo Cruz. 2008;103:741-4.
- [Google Scholar]
- Genomic diversity of group A rotavirus strains in patients aged 1-36 months admitted for acute watery diarrhoea in northern India: a hospital-based study. Clin Microbiol Infect. 2010;16:45-50.
- [Google Scholar]
- Clinical profile and prevalence of rotavirus infection in children presented with acute diarrhea at tertiary care referral hospital at northern part of India. J Commun Dis. 2009;41:183-8.
- [Google Scholar]
- Centers for disease control and prevention, Atlanta. Guidelines for specimen collection, 2011. Available from: http://www.cdc.gov/outbreaknet/references.../guide_specimen_collection
- [Google Scholar]
- International collaborative study to compare reverse transcriptase PCR assays for detection and genotyping of noroviruses. J Clin Microbiol. 2003;41:1423-33.
- [Google Scholar]
- Molecular detection and epidemiology of Sapporo-like viruses. J Clin Microbiol. 2000;38:530-6.
- [Google Scholar]
- Typing of human astroviruses from clinical isolates by enzyme immunoassay and nucleotide sequencing. J Clin Microbiol. 1995;33:797-801.
- [Google Scholar]
- Emerging trends in the etiology of enteric pathogens as evidenced from an active surveillance of hospitalized diarrhoeal patients in Kolkata, India. Gut Pathog. 2010;2:4.
- [Google Scholar]
- Multicenter, hospital-based surveillance of rotavirus disease and strains among Indian children aged <5 years. J Infect Dis. 2009;200(Suppl 1):147-53.
- [Google Scholar]
- Acute infantile gastroenteritis associated with human enteric viruses in Tunisia. J Clin Microbiol. 2008;46:1349-55.
- [Google Scholar]
- Epidemiological, clinical, and molecular features of norovirus infections in western India. J Med Virol. 2009;8:922-32.
- [Google Scholar]
- Human caliciviruses in symptomatic and asymptomatic infections in children in vellore, south India. J Med Virol. 2007;79:544-51.
- [Google Scholar]
- Genetic diversity of noroviruses and sapoviruses in children with acute sporadic gastroenteritis in New Delhi, India. J Clin Virol. 2008;43:42-8.
- [Google Scholar]
- Emergence of unique variants and inter-genotype recombinants of human astroviruses infecting infants, children and adults in Kolkata, India. Int J Mol Epidemiol Genet. 2011;2:228-35.
- [Google Scholar]
- Astrovirus associated acute gastroenteritis in western India: predominance of dual serotype strains. Infect Genet Evol. 2010;10:575-9.
- [Google Scholar]
- Molecular epidemiology of human astrovirus infections in Kolkata, India. Infect Genet Evol. 2006;6:425-35.
- [Google Scholar]
- Laboratory diagnostic challenges in case/control studies of diarrhoea in developing countries. Clin Infect Dis. 2012;55(Suppl 4):S312-6.
- [Google Scholar]






