Translate this page into:
Emergency contraception - Potential for women's health
Reprint requests: Dr Suneeta Mittal, Director & Head, Department of Obstetrics & Gynaecology, Fortis Memorial Research Institute (FMRI) Sector 44, Opposite HUDA City Centre, Gurgaon 122 002, Haryana, India e-mail: suneeta.mittal@gmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Emergency contraception (EC) is a safe and effective method which is used to prevent unwanted pregnancy after unprotected sexual intercourse. Many of the unwanted pregnancies end in unsafe abortions. The search for an ideal contraceptive, which does not interfere with spontaneity or pleasure of the sexual act, yet effectively controls the fertility, is still continuing. Numerous contraceptive techniques are available, yet contraceptive coverage continues to be poor in India. Thus, even when not planning for a pregnancy, exposure to unprotected sex takes place often, necessitating the use of emergency contraception. This need may also arise due to failure of contraceptive method being used (condom rupture, diaphragm slippage, forgotten oral pills) or following sexual assault. Emergency contraception is an intervention that can prevent a large number of unwanted pregnancies resulting from failure of regular contraception or unplanned sexual activity, which in turn helps in reducing the maternal mortality and morbidity due to unsafe abortions. However, a concern has been expressed regarding repeated and indiscriminate usage of e-pill, currently the rational use of emergency contraception is being promoted as it is expected to make a significant dent in reducing the number of unwanted pregnancies and unsafe abortions. In fact, since the introduction of emergency contraception, the contribution of unsafe abortion towards maternal mortality has declined from 13 to 8 per cent.
Keywords
Emergency contraception
IUD
levonorgestrel
pregnancy
unprotected sex
Yuzpe regimen
Introduction
Emergency contraception (EC) is a method of contraception that is used to prevent pregnancy after an act of unprotected sexual intercourse. It is known by several other names e.g. ‘morning after’ or post-coital method. These methods are for one time use following a contraceptive accident and are effective if used within a short time frame after sexual exposure. As the name signifies, it is meant only for contraceptive emergency situations and not for routine or repeated use.
Emergency contraception is effective only in the first few days following intercourse before the ovum is released from the ovary and before the sperm fertilizes the ovum. Emergency contraceptive pills cannot interrupt an established pregnancy or harm a developing embryo, thus cannot cause abortion. Emergency contraception prevents about 85 per cent of pregnancies and does not replace regular contraception1. Extensive research has been carried out on several new approaches for emergency contraception during the last decade and new studies are focussed on repeated post-coital use.
Effectiveness
Since the method is for one time use, the effectiveness cannot be calculated as Pearl index (no. of pregnancies per 100 women years). Efficacy is expressed in two ways: (i) overall pregnancy rate - Failure / 100 women; and (ii) ‘prevented fraction’ of pregnancies – calculated as:
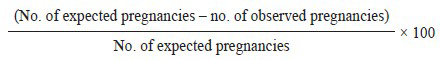
Number of expected pregnancies is calculated by probability of conception based on the cycle day of the menstrual cycle at the time of sexual exposure. Most women having single unprotected intercourse will not conceive, but it is difficult to identify fertile days. With a single random act of coitus approximately 8 per cent women would conceive, though probability may be as high as 40 per cent at the time of ovulation2.
Screening and assessment for EC use
Should include date of last menstrual period (LMP), average length of menstrual cycle, timing of last act of intercourse and previous acts, time in hours since last act of unprotected intercourse, current or recent use of contraception, history of medical disorders, sexually transmitted disease or major illness. Physical examination is not necessary except when pregnancy is suspected. Laboratory tests include urine pregnancy test if pregnancy is suspected and tests for sexually transmitted diseases, if at risk.
Need for EC
Annually, approximately 210 million pregnancies occur, of which 46 million (22%) end in induced abortions and 20 million in unsafe abortions4. Majority of these (95%) occur in developing countries and 13 per cent of pregnancy related deaths are due to unsafe abortion as a consequence of unwanted pregnancy4. Contraception is an important step to prevent pregnancy. There is a significant ‘unmet need’ of contraception, besides, contraceptive failure can also result in unwanted pregnancies. Women risk their lives to terminate an unwanted pregnancy or to carry it to term. Accidental pregnancies resulting from contraceptive failure worldwide with “perfect use” of methods are 5.9 million and with “typical use” of methods are 26.5 million4.
Introduction of EC in India
India participated in research trials of WHO Division for reproductive health and high risk pregnancy (WHO-RHR/HRP) in 1995-1997 in 1998-2001. Research provided sound scientific foundation of efficacy and safety in Indian women. A Consortium on National Consensus for Emergency Contraception was held in January, 2001 where the following issues were discussed for consensus5: (i) Dedicated method of choice for EC in India; (ii) Pre-introduction IEC and media campaigns; (iii) Training of healthcare providers; (iv) Ideal approach for distribution to the masses; (v) Client information and counselling; and (vi) Monitoring of the programme.
The Report & Recommendations of the Consortium was released in June, 20015. Subsequently, EC was approved by the Drug Controller General of India (DCGI) in September 2001, permission was granted for manufacture / import of levonorgestrel (LNG) and social marketing on prescription and the drug was made available in the country in January 2002. There were several challenges for introducing EC in India, including the size and diversity of the country and poor awareness of both users and providers.
Impact of EC
EC today is an important method for women whose contraception had failed or who have had unprotected sex, however, it is no substitute for correct regular use of contraception.
It is a safe option and is maximally effective in the first 12 hr after contraceptive accident or unprotected sex, thus access to this treatment needs to be fast. Studies show that women need more awareness about exactly when they should take ECP and understand what puts them at risk of pregnancy6. In Shanghai, significant reduction was reported in number of induced abortions following availability of ECP from vending machine (Personal communication, Lian Chang, Shanghai Institute of Population Studies, Shanghai)Table I.
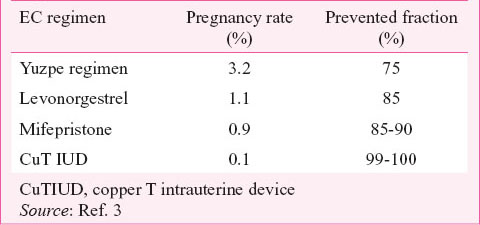
Contraceptive acceptance following the use of emergency contraception
A field based cross-sectional study after six months of EC use was carried out in New Delhi, India, with all EC acceptors regarding there regular use of contraception7. The results depicted in Table II, clearly indicate that EC use can act as a bridge for regular contraceptive use, as consultation for EC provided an opportunity to discuss regular contraception. Most contraceptives were initiated in the very first cycle7.
Advance provision of EC
Emergency contraception is most effective at preventing unintended pregnancy when taken as early as possible following unprotected sexual intercourse. Advance provision of this medication supports more timely and effective use. Usage of emergency contraception increased with advance provision and there was no increase in negative sexual behaviours or decrease in usage of other contraceptive forms8. The existing literature suggests that among women 24 years of age or younger, advance provision has a positive impact on use and time to use of EC8. Most findings indicate that increased use of EC does not have significant negative effects for ongoing contraceptive use or sexual risk taking behaviours. Despite increased use, advanced provision of EC has not been found to be associated with a significant corresponding decrease in pregnancy8.
A Cochrane review (2007)9 has shown that advanced provision does not reduce pregnancy rate when compared to conventional provision. This does not negatively impact sexual and reproductive health behaviour and outcomes. Women should have easy access to EC because it may decrease the chance of pregnancy, however, interventions tested so far have not reduced overall pregnancy rates in the populations studied9.
Types of emergency contraceptive pills (ECPs)
The progestin only method uses the progestin levonorgestrel in a dose of 1.5 mg, either as two 750 μg doses 12 h apart, or as a single dose pill (typically up to 72 h after intercourse; can be upto 120 h)10. The combined or Yuzpe regimen uses large doses of both estrogen and progestin, taken as two doses at a 12 h interval and is less effective and less well-tolerated than the progestin-only method10. Ulipristal acetate was approved as an ECP in Europe in early 2009 and in the US in August 2010. It works for up to 120 h after intercourse11. A recent meta-analysis of two randomized clinical trials showed ulipristal acetate to have a pregnancy risk 42 per cent lower than levonorgestrel up to 72 h and 65 per cent lower in the first 24 h following unprotected intercourse12. Moreover, when taken beyond 72 h, significantly more pregnancies were prevented with ulipristal acetate than with levonorgestrel. Side effects are mild and similar to those seen with levonorgestrel.
In China and Russia mifepristone is generally used as either EC or as an abortfacient. Intrauterine device (IUD) for emergency contraception is an effective alternative to ECPs. Copper-T IUD can be used up to five days after unprotected intercourse to prevent pregnancy13. Insertion of an IUD is more effective than the use of ECPs. Pregnancy rates when used as emergency contraception are the same as with normal IUD use13.
IUDs may be left in place following the subsequent menstruation to provide ongoing contraception (3–10 years depending upon type). In a prospective, multicentre, cohort clinical trial of Copper T380A intrauterine device for emergency contraception, women requesting emergency contraception were followed at 1, 3 and 12 months after the insertion of CuT380A. No pregnancies occurred prior to or at the first follow up visit, making CuT380A 100 per cent effective as emergency contraception in this study14. The pregnancy rate over the 12-month period was 0.23 per 100 women. In all, 1.5 per cent women experienced a difficult IUD insertion process, requiring local anaesthesia or prophylactic antibiotics. No uterine perforations occurred. The main side-effects were increased menstrual bleeding and menstrual disturbances. The 12-month postinsertion continuation rate was 94.0 per 100 woman-years14. An enteric-coated levonorgestrel emergency contraceptive pill (E-LNG-ECP) is an improved formulation, in terms of side effects, which is both dissolved and absorbed in the intestine15.
Newer emergency contraception drugs
The selective progesterone receptor modulators (SPRMs) are progesterone receptor ligands that bind to progesterone receptor (PR) and exert antagonistic, agonistic or mixed agonist-antagonistic effects and include mifepristone, onapristone, asoprisnil, ulipristal, proellex among other compounds16. Currently developed SPRMs exert contraceptive effects inhibiting ovulation and retarding endometrial synchronization. Low-doses of progesterone antagonists retard endometrial maturation without affecting ovulation16.
Ulipristal acetate goes one-step ahead of levonorgestrel in the field of emergency contraception treatment. It is a SPRM with similar effectiveness and side effect profiles as 1.5 mg levonorgestrel EC, has shown wider ‘window of effect’ by inhibition of the luteinizing hormone (LH) peak even if administered at the advanced pre-ovulatory phase, a time when use of levonorgestrel EC is no longer effective17. Further studies are needed to explore the potential of other SPRMs as emergency contraceptive drugs. Ulipristal acetate is generally well tolerated, with a similar tolerability profile to that of levonorgestrel. In general, the onset of menstruation is delayed by 2-3 days following treatment17. Although, ulipristal acetate is more expensive than levonorgestrel, it may represent a cost-effective alternative to levonorgestrel for women requesting emergency contraception within 120 hours of unprotected intercourse.
Need for emergency contraception in India
The relevance of EC can be derived from the fact that attempts to stabilize the population have not met success yet. While every unwanted pregnancy is a burden on maternal physical and mental health, it is also a contributor to infant morbidity and mortality. National Family Health Survey (NFHS) III figures reveal the couple protection rate to be 56 per cent and unmet need to be 12.8 per cent18. A significant percentage of maternal mortality is due to unsafe abortions, taking place in women with unwanted pregnancies. The desire to limit family size and to space the next birth are the main reasons given by the majority of those who seek an abortion. Rational use of emergency contraception in India can play a very important role in reducing maternal mortality and morbidity, and improving women's health. It can also indirectly contribute towards reduction of perinatal mortality and morbidity by preventing unwanted births. In India knowledge about various temporary and permanent methods among men and women ranges between 45-97 per cent, knowledge about EC is only 20 per cent in men and 11 per cent in women18.
Indications of use of emergency contraception
These include unanticipated sexual intercourse, teenage sex, unprotected exposure (sexual assault, rape, sexual coercion), contraceptive accidents with natural and regular methods, miscalculation of safe period, failed coitus interruptus, condom rupture or slippage, late insertion of spermicide, pill forgotten for two consecutive days or pill free interval of nine or more days between packets, more than 12 hour delay in taking progesterone only pill, delay of progestin injectable contraceptive injection by 2 wk, delay of combined estrogen and progestin injectable contraceptive injection by 3 days, and expelled or misplaced IUD.
What influences young women to choose between the emergency contraceptive pill and an intrauterine device?
Most women had an unrealistically high expectation about efficacy of the ECP and lacked knowledge of the IUD as an alternative method of EC14. Previous use, easy accessibility, ease of use, and advice from peers influenced women to choose the ECP, whereas past experience of abortion, firm motivation to avoid pregnancy, presentation after 72 hours, and considering that an IUD may provide long-term contraception as well, inclined women to choose the IUD. Showing the IUD during counselling might help correct misconceptions and would improve acceptability.
How emergency contraception works
Emergency contraceptive pills prevent pregnancy primarily, or perhaps exclusively, by delaying or inhibiting ovulation. There is no evidence to suggest that either of the FDA-approved EC options, (LNG) or ulipristal acetate (UPA) works after an egg is fertilized. In two recent studies1920 among women taking LNG before ovulation, there were no pregnancies, those who took it on the day of ovulation or after, there were about the same number of pregnancies that would be expected with no use of EC. If LNG was effective at preventing implantation, it would most certainly be more effective when taken after ovulation. No morphological or molecular alterations in the endometrium that could interfere with the implantation of the fertilized egg have been demonstrated. A study of UPA has shown that at certain doses, it can decrease the thickness of the endometrium (by 0.6 to 2.2 mm), but it is not clear that this would in fact prevent the implantation of a fertilized egg20. The copper-T IUD does not affect ovulation, but it can prevent sperm from fertilizing an egg. It may also prevent implantation of a fertilized egg19.
ECPs do not interrupt an established pregnancy, defined by medical authorities such as the United States Food and Drug Administration/National Institutes of Health and the American College of Obstetricians and Gynecologists as beginning with implantation. Therefore, ECPs are not abortifacient. The best available evidence shows that levonorgestrel and ulipristal acetate ECPs prevent pregnancy primarily by delaying or inhibiting ovulation and inhibiting fertilization, mechanisms that do not involve interference with post-fertilization events21. Its high effectiveness implies that emergency insertion of a copper IUD must be able to prevent pregnancy after fertilization. IUDs when used as a regular method of contraception, act primarily through spermicidal and ovicidal mechanisms, but it is considered possible that these same mechanisms are also harmful to zygotes that have not yet implanted.
Contraindications to EC Use
Existing pregnancy is not a contraindication in terms of safety, as there is no known harm to the woman, the course of her pregnancy, or the foetus. EC is not indicated for a woman with a known or suspected pregnancy. The WHO lists no medical condition for which the risks of emergency contraceptive pills outweigh the benefits22. Progestin-only ECPs may be preferable to combined ECPs containing estrogen in women with a history of blood clots, stroke, or migraine, there is no medical conditions in which progestin-only ECPs are contraindicated. Current venous thromboembolism, current or past history of breast cancer, inflammatory bowel disease, and acute intermittent porphyria are conditions where the advantages of EC generally outweigh the theoretical or proven risks22
Side effects of ECs
Side effects include nausea and vomiting, abdominal pain, breast tenderness, headache, dizziness, and fatigue. About 50 per cent of women who take combined ECPs experience nausea and 20 per cent vomit. If vomiting occurs within two hours after taking a dose, repeating that dose is also recommended. The non-prescription anti-nausea medicine meclizine has been demonstrated to reduce the risk of nausea by 27 per cent and vomiting by 64 per cent when two 25 mg tablets are taken 1 hour before combined ECPs, but the risk of drowsiness was doubled (to about 30%)23.
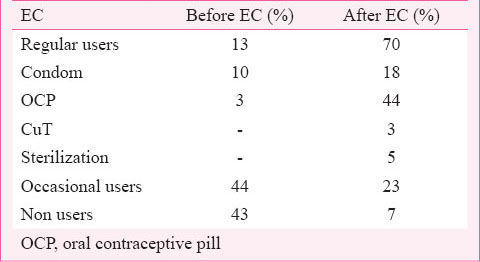
Side effects usually do not occur for more than a few days after treatment, and generally resolve within 24 hours. Temporary disruption of the menstrual cycle is commonly experienced. If taken before ovulation, the high doses of progestogen may induce progestogen withdrawal bleeding a few days after the pills are taken. If taken after ovulation, it may increase the length of the luteal phase, thus delaying menstruation by a few days. Mifepristone, if taken before ovulation, may delay ovulation by 3-4 days24. Disruptions only occur in the cycle in which ECPs are taken; subsequent cycle length is not significantly affected. If a woman's menstrual period is delayed by a week or more, she should go for a pregnancy test. Follow up algorithm is given in the Figure.
- Alogorithm for follow up after the use of emergency contraceptive (EC).
Effects of EC on pregnancy
There have been no conclusive studies of births to women who were already pregnant when they took combined ECPs or following failure of combined ECPs. However, one study of 332 pregnant women who had used levonorgestrel-only ECPs in the conception cycle found no increased risk of birth defects25. First, in the event of treatment failure, ECPs are taken long before the organogenesis starts so they should not have a teratogenic effect. Second, studies that have examined births to women who inadvertently continued to take combined oral contraceptives (including high dose formulations) without knowing they were pregnant have shown no risk of birth defects26.
EC and ectopic pregnancy
Studies have concluded that ECPs, like all other contraceptives, reduce the absolute risk of ectopic pregnancy by preventing pregnancies. In a randomized controlled trial (RCT) with over 7,800 women there was no increase in the relative risk of ectopic pregnancy in women who became pregnant after using progestin-only ECPs27. A systematic review of ectopic pregnancy and emergency contraceptive pills showed that the rate of ectopic pregnancy when treatment with emergency contraceptive pills fails does not exceed the rate observed in the general population28. Because emergency contraceptive pills are effective in lowering the risk of pregnancy, their use will reduce the chance that an act of intercourse will result in ectopic pregnancy. Although the possibility of ectopic pregnancy after intake of LNG as EC pill is there, the causality has not been well established29. A high serum LNG concentration decreases ciliary activity and tube motility30, but further epidemiological studies are necessary to establish the risk of ectopic pregnancy following intake of LNG ECP.
Emergency contraception: Safe for repeat use
According to all available data, there is no risk associated with the repeat use of EC. The FDA's Safety Review31 confirms that no cases of overdose or addiction to the drug have been reported and points to several studies over the past several decades to affirm the safety of repeat use. At the same time, other contraceptive methods are more reliable, and may help women avoid side effects, such as menstrual irregularity, thus there use is to be encouraged. EC may be used even if the woman has used it before, even within the same menstrual cycle, there is no contraindication to repeated ECP use, and women should not be denied repeat access to ECPs if needed. Repeat use is uncommon, even when women have an easy access to the method32. Medical and behavioural research does not provide any basis for limiting the number of times women use ECPs
In every single case, ECPs are safer than pregnancy especially when the pregnancies are unintended and women do not have access to safe abortion services. Women could use ECPs as often as needed.
EC and sexual assault: Pregnancy rates among rape victims of child-bearing age are around 5 per cent in the U.S33 about half of rape victims who become pregnant have abortions. EC is commonly used as an option for victims of sexual assault.
Potential of emergency contraception
Emergency contraception is a woman's last chance to prevent unintended pregnancy. Population studies have not shown that increased access to EC decreases abortion rates; this is likely due to inconsistent and infrequent use even when it is available34. Use does not lead to more risky sexual practices or behaviours35.
Way forward - Plan of action
Gender-sensitive information tools on EC need to be designed for chemists and pharmacists. There is a need to develop training modules and train providers in the public and private sector. Also public awareness about EC, should be raised. There is enormous potential for EC in improving the reproductive health of women in the country.
Unwanted pregnancy is a social as well as economic burden for the society with a high complication rate. National guidelines for family planning should encourage the use of regular contraception as well as consider counselling for emergency contraception specially for women undergoing medical termination of pregnancy. It is important that everyone understands that no contraceptive method is 100 per cent effective. All women may need a last-minute chance to prevent unwanted pregnancy by making emergency contraception accessible as a back-up method.
References
- Emergency contraception. In: Hatcher RA, Trussell J, Nelson AL, eds. Contraceptive technology (17th ed). New York: Ardent Media; 1998.
- [Google Scholar]
- Timing of sexual intercourse in relation to ovulation: effects on the probability of conception, survival of the pregnancy and sex of the baby. N Engl J Med. 1995;333:517-21.
- [Google Scholar]
- Consortium for National Consensus on Emergency Contraception in India. Published by WHO-CCR in Human Reproduction. 2001. Available from: www.aiims.ac.in
- [Google Scholar]
- Emergency contraception with update on regular contraception - Guidebook for health care providers. Geneva: WHO-CCR in Human Reproduction; 2006.
- [Google Scholar]
- Advance supply of emergency contraception: a systematic review. Contraception. 2013;87:590-601.
- [Google Scholar]
- Advance provision of emergency contraception for pregnancy prevention. Cochrane Database Syst Rev 2007:CD005497.
- [Google Scholar]
- Task Force on Post-ovulatory Methods of Fertility Regulation. Randomized Control Trial of levonorgestrel versus Yuzpe regimen of combined oral contraceptives for emergency contraception. Lancet. 1998;352:428-33.
- [Google Scholar]
- Immediate pre-ovulatory administration of 30 mg ulipristal acetate significantly delays follicular rupture. Hum Reprod. 2010;25:2256-63.
- [Google Scholar]
- Ulipristal acetate versus levonorgestrel for emergency contraception: a randomized non-inferiority trial and meta-analysis. Lancet. 2010;375:555-62.
- [Google Scholar]
- A qualitative exploration of emergency contraception users’ willingness to select the copper IUD. Contraception. 2012;85:32-5.
- [Google Scholar]
- Efficacy and safety of a levonorgestrel enteric-coated tablet as an over-the-counter drug foremergency contraception: a Phase IV clinical trial. Hum Reprod. 2011;26:2316-21.
- [Google Scholar]
- Selective progesterone receptor modulators and progesterone antagonists: mechanisms of action and clinical applications. Hum Reprod Update. 2005;11:293-307.
- [Google Scholar]
- Ulipristal acetate and its role in emergency contraception: a comment. Expert Opin Pharmacother. 2012;13:1821-3.
- [Google Scholar]
- National Family Health Survey 3 (2005-6) Available from: http://www.rchiips.org/nfhs/pdf/India.pdf
- [Google Scholar]
- Mechanisms of action of mifepristone and levonorgestrel when used for emergency contraception. Hum Reprod Update. 2004;10:341-8.
- [Google Scholar]
- The effect of levonorgestrel administered in large doses at different stages of the cycle on ovarian fuction and endometrial morphology. Contraception. 1989;39:275-87.
- [Google Scholar]
- World Health Organisation. Medical eligibility criteria for contraceptive use. (4th ed). Geneva: WHO; 2009.
- [Google Scholar]
- Metoclopramide pretreatment attenuates emergency contraceptive-associated nausea. Am J Obstet Gynecol. 2003;188:330-3.
- [Google Scholar]
- Comparison of three single doses of mifepristone as emergency contraception: a randomised trial. Task Force on Postovulatory Methods of Fertility Regulation. Lancet. 1999;353:697-702.
- [Google Scholar]
- Pregnancy outcome after levonorgestrel-only emergency contraception failure: a prospective cohort study. Hum Reprod. 2009;24:1605-11.
- [Google Scholar]
- Pregnancy outcome after exposure to oral contraceptives during the periconceptional period. Hum Exp Toxicol. 2008;27:307-13.
- [Google Scholar]
- Ectopic gestation following emergency contraception with levonorgestrel. Eur J Contracept Reprod Health Care. 2003;8:225-8.
- [Google Scholar]
- Ectopic pregnancy after levonorgestrel emergency contraception. Contraception. 2011;83:281-3.
- [Google Scholar]
- Ectopic pregnancy that occurred after failure of levonorgestrel emergency contraception. Contraception. 2011;84:206-7.
- [Google Scholar]
- Ectopic pregnancy following emergency contraception with ethinyloestradiol-levonorgestrel: a case report. Eur J Contracept Reprod Health Care. 2007;12:184-6.
- [Google Scholar]
- Repeated use of pre- and postcoital hormonal contraception for prevention of pregnancy. Cochrane Database Syst Rev 2010:CD007595.
- [Google Scholar]
- Repeated use of pre- and postcoital hormonal contraception for prevention of pregnancy. Cochrane Database Syst Rev. 2014;9:CD007595.
- [Google Scholar]
- U.S. women's one-year contraceptive use patterns, 2004 Perspect Sex Reprod Health. . 2007;39:48-55.
- [Google Scholar]
- Emergency contraceptive use among 5677 women seeking abortion in Shanghai, China. Hum Reprod. 2009;24:1612-8.
- [Google Scholar]
- A repeated survey of sexual behavior among female university students in Sweden. Acta Obstet Gynecol Scand. 2012;91:215-9.
- [Google Scholar]






