Translate this page into:
A study on surgical site infections after trauma surgeries in a tertiary care hospital in north India
† For correspondence: purvamathur@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Surgical site infections (SSIs) are one of the major causes of morbidity and mortality in developing countries despite recent advances in aseptic techniques. Globally, surgical site infection rates have been reported in a range from 2.5 to 41.9 per cent123456. In the United States, SSIs accounted for 17 per cent of all HAIs among hospitalized patients in 20027. Similar rates have been reported from the National Healthcare Safety Network (NHSN) hospitals in 2006-2008 (16,147 SSI following 849,659 operative procedures) with an overall rate of 1.9 per cent8. In a 7-year study conducted in the US, the overall rate of surgical site infection after open reduction and internal fixation of tibial plateau fractures was 7.8 per cent9 and traumatic vascular surgery SSI was reported to occur in 5-10 per cent of such patients10. In another study conducted on trauma patients who underwent exploratory laparotomy after abdominal injury, 13.8 per cent experienced deep incisional and organ/intra-abdominal SSIs11.
For the purpose of surveillance, Centers for Disease Control and Prevention (CDC) have set definite criteria. A SSI was defined as purulent drainage (category 1); a positive aseptically collected culture (category 2); at least one sign of inflammation with opening of the incision and absence of a negative culture (category 3); or physician diagnosis of infection (category 4). For CDC category 4, carefully noted details of those cases should be taken to discriminate situations of (i) definite cellulites that was treated with antibiotics (previously included but now excluded as per 2010 reporting instructions); or (ii) other scenarios that would fit the 2010 criteria for category 4 SSI (e.g. wound was opened, culture was negative, and cellulites was also present)121314. Clinically, infections are categorized into those that affect superficial tissues (skin and subcutaneous layer) of the incision and those that affect the deeper tissues (deep incisional or organ-space) according to the CDC definitions1215. A time period of 30 days has been taken after surgery for an infection to be called SSI in cases with no implants but it can extend up to one year in patients with implants12. Data regarding SSI from developing countries are scarce especially those developing post discharge from hospitals and hence this study was conducted in a level I trauma centre of north India.
During May 2011 to September 2012, a total of 5,620 surgical cases were admitted for trauma in Jai Prakash Narayan Apex Trauma Centre, All India Institute of Medical Sciences, New Delhi, and all those patients who had undergone surgical interventions were followed up. Of these, 2767 were found to be possible candidates for SSI and were intensively followed. Appropriate samples representative of the suspected site of infection were taken in relation to the wound for microbiological cultures and sensitivity with repeat samples taken after one week and later. The sample processing for diagnosis of bacterial and fungal pathogens was done by standard methods1617. The bacterial isolates were identified by the VITEK 2® compact system (BioMérieux, Lyon, France). The antimicrobial susceptibility testing was done by the disc diffusion method, according to the Clinical Laboratory Standards Institute (CLSI) guidelines1819 and the VITEK 2 system. Antimicrobial sensitivity pattern and change of flora along with change in sensitivity were noted and followed.
A total of 107 patients were found to have SSIs among the total 2,767 patients. Of the 107 confirmed cases of SSIs, 96 (89.7%) were males. The mean age was 25.8 ± 5 yr with a range of 4-42 yr. Among the confirmed SSI cases, 91 (85%) were pure surgical patients where interventions were done and the remaining 16 (15%) had other interventions like orthopaedic manipulations or neurosurgical procedures besides major surgical procedures. Of the 2767 patients 948 (34%) were admitted to the surgical ICUs, 1012 (37%) were admitted to the general surgery wards and the remaining 807 (29%) were from the follow up OPD. It was observed that 40 (37.4%) of the 107 the patients who later developed SSIs were from surgical ICUs, 54 (50.5%) from the other general surgery wards and the remaining 13 (12.1%) were detected during follow up in the OPD after discharge from the hospital. So, a total of 4.2 per cent of surgical ICU patients, 5.3 per cent of general surgical ward patients and 2 per cent of the follow up patients developed SSIs.
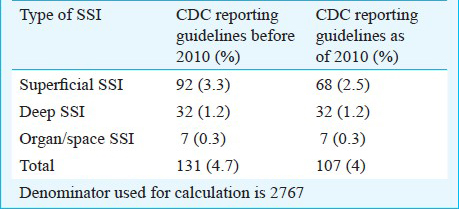
The rate of SSI among the trauma patients admitted for surgical interventions was 4 per cent (107/2767) per patient. During the study, there were many cases (150, 5.4%) of pure cellulitis which were treated with antibiotics. After the CDC criteria modifications in 2010, all such cases were excluded from SSI1213. Table I shows the comparative difference in the rate of SSIs after using the modified criteria and type of SSI.
The rate of SSIs was analysed depending on the patient's duration of hospital stay and the specific surgical procedure(s) which was undertaken for type of surgical trauma. Of the 107 patients who developed SSIs, 10 (9.3%) had pure limb trauma either upper limbs or lower limbs and such patients had a mean duration of 11 days (6-15 days) of in-hospital stay, five (4.7%) had pure abdominal trauma and its related surgery and they had a mean duration of 31 days (25-36 days) of in-hospital stay. Twenty four (22.4%) had thoracic trauma and they had a mean duration of 40 days (32-48 days), whereas 65 (60%) had multiple trauma which was treated surgically and they stayed in the hospital for a mean duration of 46 days (36-56). Those patients who had multiple injuries and had undergone numerous surgical interventions along with other surgical modalities like orthopaedic or neurosurgical intervention [3, (2.8%)] had a mean duration of 51.5 days (41-62) of hospital stay. As per definition12, the patients were grouped into three different categories. Those developing infection within 30 days of surgery during in-hospital stay [68 (64%)], those developing SSI after 30 days of surgery during in-hospital stay [26 (24.3%)], and those who developed SSI after discharge from the hospital with duration of more than 30 days of surgery but within one year [13 (12.1%)]. In this category, an extra 12.1 per cent of the patients developing SSIs during follow up were detected.
A total of 286 isolates were obtained from the culture of samples of the confirmed SSI cases. Gram-negative bacteria predominated over the Gram-positives. Acinetobacter spp. (84) predominated among the Gram-negative bacteria (Table II). More than 90 per cent of the isolates were found to be multi drug resistant (MDR). However, among the Gram-positives, no resistance to vancomycin and teichoplanin was observed.
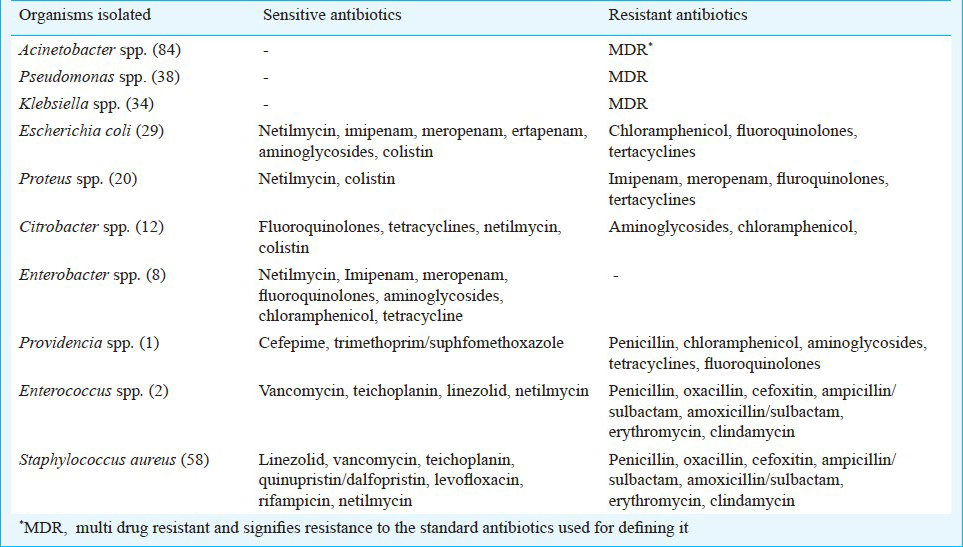
All 107 patients with SSIs all were on parenteral antibiotics at the beginning of admission due to the nature of the trauma and later as a pre-operative prophylaxis according to the hospital empiric antibiotic regime. For the Gram-positive bacteria (like Staphylococcus aureus) glycopeptides / linezolid were used. For the Gram-negative bacteria (Acinetobacter baumannii, Klebsiella Pneumonia, etc.), parenteral 3rd generation cephalosporins or aminoglycosides or metronidazole were used or specific antibiotic like colistin depending on the sensitivity pattern of the culture report. Table III shows the details of the outcomes of these SSI patients. The SSI rate in trauma patients who had undergone surgical intervention(s) was 4 per cent. This was lower than that reported in many other studies2021.
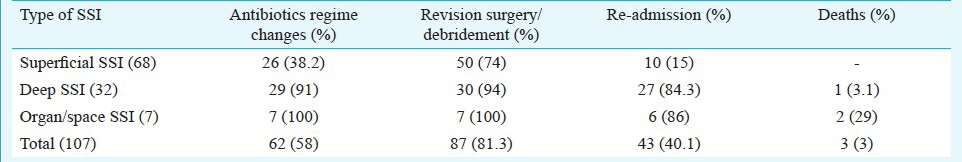
A predominance of superficial SSIs (2.5%) was seen over deep and organ/space SSIs in our study, a finding similar to other studies2021. Inclusion of SSIs detected on re-admission increased the identification of deep or organ-space infections (particularly in categories with relatively shorter median length of hospital stay) from 24-36 to 51-60 per cent22.
We have also tried to see the trend of SSIs before and after the implementation of an active surveillance programme and after changes in hand hygiene policy23. It was seen that the rate of SSIs for a duration of six months before this programme was 11.4 per cent. After that, the rate had dropped down to 8.5 per cent within the first six months (May-October 2011) of the study.
This study provides data on SSIs from a level 1 trauma centre in India which will also help in proper implementation of antibiotic stewardship, use of proper treatment protocol and proper aseptic precautions in such situations.
Acknowledgment
The authors thank All India Institute of Medical Sciences, New Delhi, for supporting this study by providing the required infrastructure and necessary material.
References
- Prevalence and predictors of SSI in Tbilisi Republic of Georgia. J Hosp Infect. 2007;66:160-6.
- [Google Scholar]
- Postoperative wound infections. The influence of ultraviolet infections of the operating room and of various other factors. Ann Surg. 1964;160:1-192.
- [Google Scholar]
- The epidemiology of wound infection. A 10 year prospective Study of 62,939 wounds. Surg Clin North Am. 1980;60:27-40.
- [Google Scholar]
- Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Reports. 2007;122:160-6.
- [Google Scholar]
- Improving risk-adjusted measures of surgical site information for the National Healthcare Safety Network. Infect Control Hosp Epidemiol. 2011;32:970-86.
- [Google Scholar]
- Surgical site infection after open reduction and internal fixation of tibial plateau fractures. Eur J Orthop Surg Traumatol. 2013;24:797-803.
- [Google Scholar]
- Vascular surgical site infection: risk factors and preventive measures. Semin Vasc Surg. 2008;21:119-23.
- [Google Scholar]
- Surgical site infection in abdominal trauma patients: risk prediction and performance of the NNIS and SENIC indexes. Can J Surg. 2011;54:17-24.
- [Google Scholar]
- Centers for Disease Control and Prevention. Surgical site infection event SSIS. Guidelines and procedures for monitoring SSI. Available from: http://www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf
- [Google Scholar]
- Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27:97-132.
- [Google Scholar]
- Surgical site infection after breast surgery: Impact of 2010 CDC reporting guidelines. Ann Surg Oncol. 2012;19:4099-103.
- [Google Scholar]
- CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Am J Infect Control. 1992;20:271-4.
- [Google Scholar]
- Tests for the identification of bacteria. In: Collee JG, Fraser AG, Marmion BP, Simmons A, eds. Mackie and McCartney practical medical microbiology (14th ed). New York: Churchill Livingstone; 1996. p. :131-45.
- [Google Scholar]
- Performance standards for antimicrobial susceptibility testing; twentieth informational supplement (June 2010 update). Clinical and Laboratory Standards Institute (CLSI) document. Pennsylvania, USA: CLSI; 2010. p. :M100S20.
- [Google Scholar]
- Performance standards for antimicrobial susceptibility testing; Twenty-second informational supplement. Clinical and Laboratory Standard Institute (CLSI) document. Pennsylvania, USA: CLSI; 2012. p. :M100S22.
- [Google Scholar]
- Post-discharge surgical site infection surveillance in a hospital in Brazil. Am J Surg. 2007;193:266-8.
- [Google Scholar]
- Impact of intraoperative behavior on surgical site infections. Am J Surg. 2009;198:157-62.
- [Google Scholar]
- Surveillance of surgical site infections in NHS hospitals in England, 2010/2011. London: Health Protection Agency, December 2011. Available from: www.hpa.org.uk
- [Google Scholar]
- Hand hygiene in developing nations: experience in a busy level-1 trauma center in India. Am J Infect Control. 2011;39:705-6.
- [Google Scholar]





