Translate this page into:
Tobacco cessation outcomes in a cohort of patients attending a chest medicine outpatient clinic in Bangalore city, southern India
Reprint requests: Dr Prem K. Mony, Associate Professor, Division of Epidemiology, St John's Research Institute, 100 feet road, Koramangala, Bangalore 560 034, India e-mail: prem_mony@sjri.res.in
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Nicotine dependence is a widely prevalent and harmful chronic addictive disorder. Quitting tobacco use is however, uncommon in India. We present long-term treatment outcomes of out-patient, tobacco cessation treatments from a specialty clinic setting in southern India.
Methods:
Patients seen in a tobacco cessation clinic were characterized for tobacco use, nicotine dependence and motivation for quitting and offered pharmacologic/non-pharmacologic treatment. They were subsequently contacted telephonically at a mean (±standard deviation) of 24 (±9.1) months to assess tobacco cessation outcome defined as ‘point prevalence of 1-month abstinence’ by self-reporting.
Results:
The mean age of participants was 48.0 ±14.0 yr. Tobacco use distribution was: beedis only (22%), cigarettes only (49%), beedis and cigarettes (18%), chewing only (2%), and smoking and chewing (9%). Two-thirds had high level of nicotine dependence. Of the 189 patients enrolled, only 15 per cent attended follow up clinics. Only 106 (56%) patients were successfully contacted telephonically and 83 (44%) were lost to follow up. Self-reported point prevalence abstinence was 5 per cent by ‘intent-to-treat’ analysis and 10 per cent by ‘responder’ analysis. Two clinical parameters – high level of nicotine dependence [estimated by the heaviness of smoking index (HSI)] and the absence of vascular or other chronic disease were found to be associated with successful quitting; these were however, not significant on multivariate analysis.
Interpretation & conclusions:
Our study has identified low quit-rates in a cohort of patients attending a hospital-based tobacco cessation clinic. In the absence of clear-cut predictors of cessation with low quit-rates, there should be continued efforts to improve cessation outcomes and identify predictors for action.
Keywords
Abstinence
cessation
clinic
India
long-term
outcome
tobacco
Nicotine dependence is known to be widely prevalent, harmful and yet neglected by clinicians and researchers alike in developing countries1. Nicotine dependence is a chronic remitting and relapsing addictive disorder. While a certain proportion of tobacco users may quit without assistance2, some require assistance with cessation, and for this sub-group of users, tobacco cessation treatments are available34. Several tobacco cessation clinics in diverse settings are functioning in India to help people to quit tobacco use. It is known that the epidemiology of tobacco use is atypical in India. Approximately 50 per cent of tobacco use is in the form of smokeless tobacco, 30 per cent as beedi smoking and 20 per cent as cigarette smoking5. Further, the average age of initiation of tobacco use is later than in industrialized countries with peak usage rates in those in their 40s and 50s compared to younger adults in industrialized countries5678. While Indians smoke less than Caucasians per day910 probably due to differences in nicotine metabolism11, quitting tobacco use is very uncommon in India512. Information on long-term quit-rates from longitudinal studies are also limited in India131415. Hence, research is needed to optimize treatment strategies16 in the under-studied group of Asian Indians1117. We had earlier characterized the baseline clinico-epidemiological profile of attendees at a tobacco cessation clinic located within the chest medicine department of a tertiary care hospital in Bangalore, south India18. Here, we present the long-term treatment outcomes of out-patient, clinic-based tobacco cessation treatments for patients in a specialty clinic setting in urban south India.
Material & Methods
Participants: The baseline characteristics of the patients attending the Tobacco Cessation Clinic in St John's Medical College Hospital, a tertiary-care, teaching hospital in Bangalore, Karnataka, India, are described elsewhere18. Briefly, this outpatient tobacco cessation clinic was located within the Chest Medicine department and was a collaborative effort between the departments of Chest Medicine and Psychiatry.
A structured validated questionnaire was administered to all attendees to obtain information on socio-demographic characteristics and tobacco-use details such as age at initiation, past quit attempts and current use per day among smokers and chewers (smokeless tobacco users). Nicotine dependence was assessed by a revised version of the Fagerström Test for Nicotine Dependence (FTND) among smokers19 and among smokeless tobacco users (FTND-ST)20. Heaviness of Smoking Index (HSI), the sum of two of the six items of the FTND was also computed, as it is thought to reflect dependence and work as well as the FTND21. Information on self-use of other addictive substances (e.g. alcohol) and family history of tobacco use were collected; presence of medical co-morbidities was also documented. All patients were interviewed and categorized into one of five ‘stages of readiness to change’: (i) Pre-contemplation stage: with no intention to quit tobacco; (ii) Contemplation stage: awareness that smoking is a problem but with ambivalence about the perspective of changing and hence no quit date planned; (iii) Preparation stage: 6-month intention to quit; (iv) Action stage: has quit in the last 1-month or 1-month intention to quit, and (v) Maintenance stage: has quit for more than 1 month13; (stages 3 and 4 were merged as ‘intention-to-quit’ for analysis, since there was no one who had quit in the last 1 month). Subsequently, the patients in early stages of readiness to change (Stage 1-3) underwent motivational interviewing (MI) to help resolve the ambivalence related to tobacco use and change the behavioural stage14. Based on grade of nicotine dependence, motivational stage and presence of co-morbidities, treatment modalities were offered: behavioural counselling for all patients and pharmacologic therapy for a subset of patients. Nicotine replacement therapy (NRT), bupropion sustained release (SR) and varenicline were offered as first-line pharmacotherapies, whereas nortriptyline and clonidine were the second-line treatments22.
The baseline clinico-epidemiologic characteristics of 189 patients recruited during the period August 2007 to July 2009 were characterized18. About 95 per cent of patients were referral patients from other departments of the hospital; only 5 per cent were ‘walk-in’ patients attempting to quit tobacco use. Most patients were smokers (98%) and males (97%). Distribution by type of tobacco use was into one of the five categories: beedis only (22%), cigarettes only (49%), beedis and cigarettes (18%), chewing only (2%) and smoking and chewing (9%). Most patients were married (88%) and predominantly urban (69%). About 62 per cent had completed at least eight years of schooling. The mean (±SD) age of attendees was 48.0 (±14.0) yr; exclusive cigarette smokers (44.9±13.9 yr) were younger than exclusive beedi smokers (56.4±11.3 yr) (P< 0.001). An overwhelming majority of attendees were daily users of tobacco. The mean age at initiation was 18.8 (±5.5), 20.8 (±8.5) and 25.8 (±11.3) yr for beedi smokers, cigarette smokers and chewers, respectively. About four-fifths (79%) of tobacco-users reported a family member using tobacco. About 52 per cent reported concomitant alcohol use. Overall tobacco consumption in terms of number of beedis and cigarettes smoked per day was 20±10 and 15±11, respectively; tobacco was reported to be chewed about 12±24 times per day. About 43 per cent of patients had attempted quitting earlier, with no difference by type of tobacco user.
Commonly documented medical co-morbidities included: chronic respiratory disease (44%), hypertension (23%), diabetes (12%), tuberculosis (9%), myocardial infarction (2%), stroke (1%), sexual dysfunction (1%) and cancer (0.5%). Two-thirds of smokers reported high levels of nicotine dependence [FTND score > 5/10 or Heaviness of Smoking Index (HSI) score ≥ 4/6]. Overall mean dependence score was 5.8±2.5. At baseline, distribution by patients’ motivational stage-of-change was: pre-contemplation (14%), contemplation (48%), preparation/action (37%) and maintenance (1%)18.
Treatment categories: All patients received an intensive intervention of ‘disease-specific, front-loaded counselling’ followed by advice to re-visit the clinic on a regular basis at 2, 4, 6 and 12 wk and at 9 and 12 months. Treatment modalities started were: counselling alone (41%), nicotine replacement therapy (NRT) with chewing gums (34%), medication alone (13%), and NRT + medication (12%)18.
Follow up, classification of treatment outcomes and data analysis: All 189 tobacco users were contacted by a research assistant through telephone during October 2010 for their current tobacco use. ‘Loss to follow up’ was defined as failure to establish contact by telephone. This yielded proportion lost to follow up as also the reasons for loss to follow up. Mean duration of follow up was recorded for all patients. Of the 189 patients enrolled in the clinic, 106 (56%) were successfully contacted telephonically and 83 (44%) were lost to follow up [54 (28.5%) had disconnected cellphone service/ported to another service provider, 28 (15%) had no documented phone details and 1(0.5%) had expired]. Mean duration of follow up was 24 ±9.1 months-yielding 4536 person-months of follow up for the baseline set of 189 patients and 2544 person-months of follow up for the subset of 106 patients successfully contacted by telephone.
Cessation outcome was defined as ‘point prevalence of 1-month abstinence’ by telephonic self-reporting. This was calculated by ‘intent-to-treat analysis’ for all baseline patients initiated on treatment (n=189) as well as by ‘responder analysis’ for all patients successfully contacted over telephone. Patients lost to follow up were assumed to be continuing to use tobacco.
Informed consent was obtained from all clinic attendees and ethical approval for the study protocol was obtained from the St John's Institutional Ethics Review Board.
Data were analyzed using SPSS-PC (version 13.0 (Chicago: SPSS Inc; USA). Descriptive statistics along with inferential testing using Chi-square tests were used for the outcomes of interest; significance was set at a P< 0.05. Parameters with P< 0.10 were included in a multivariate logistic regression analysis model for quitting.
Results
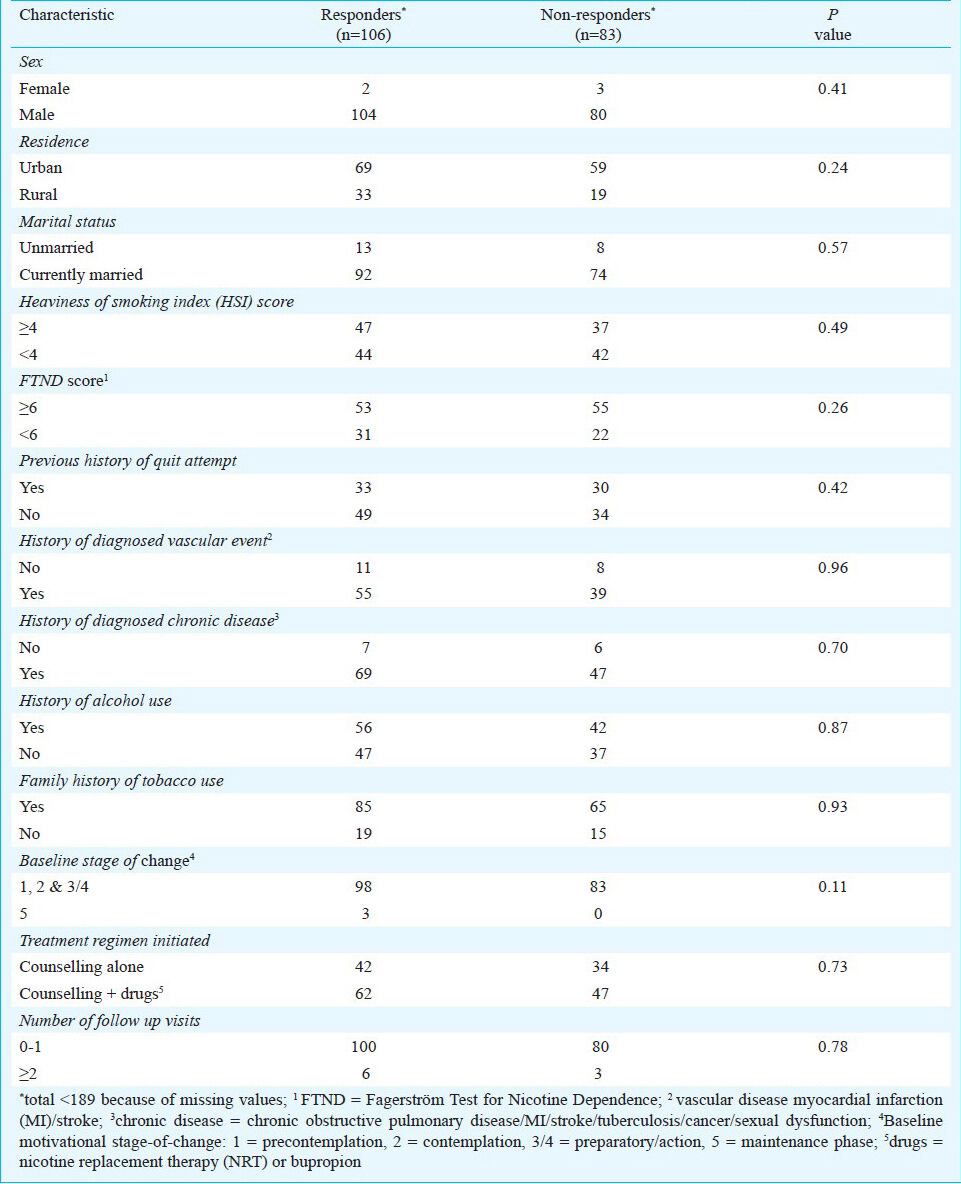
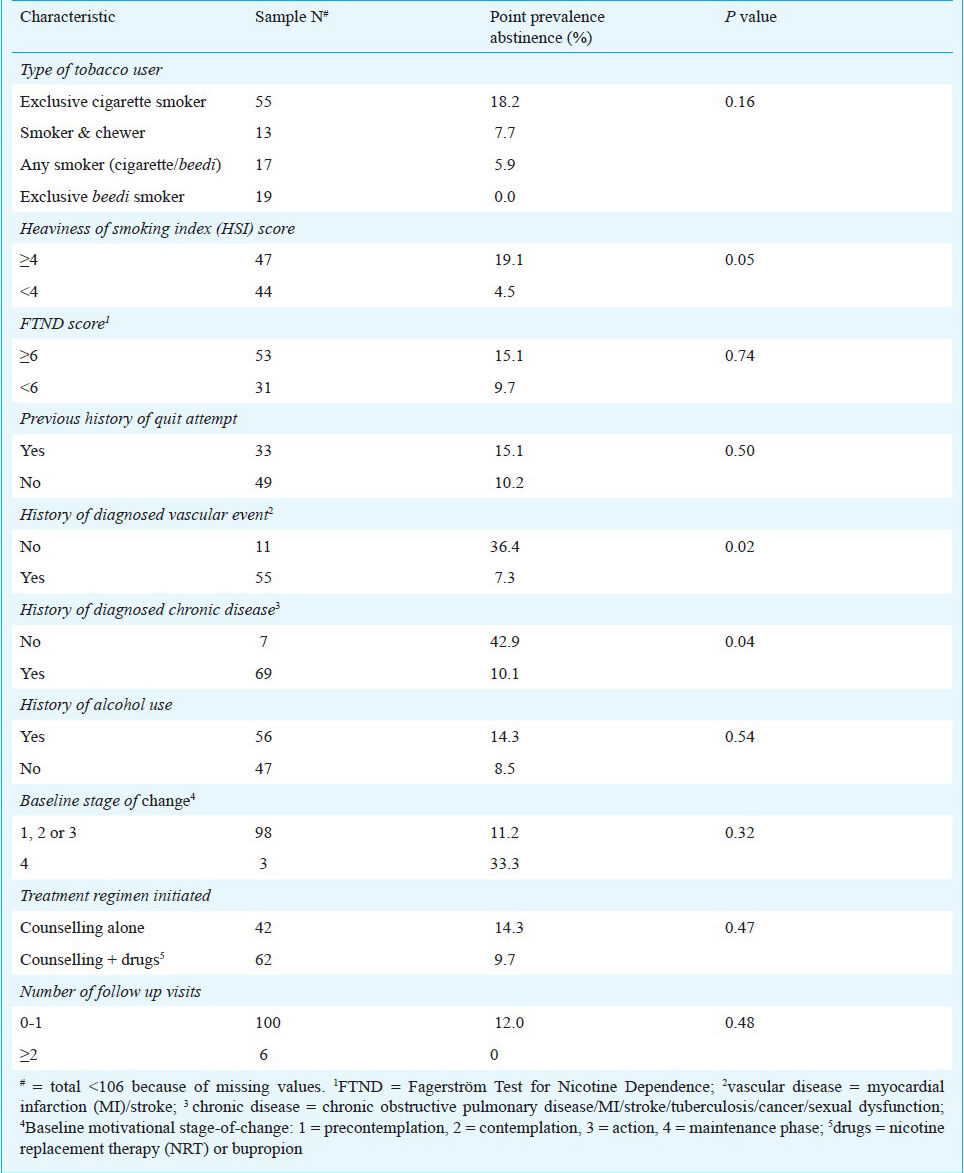
Differences in baseline socio-demographic and clinical characteristics between those who were successfully contacted by telephone and those who could not be contacted at the two-year follow up are depicted in Table I. There were no significant differences between the two groups. In our study, self-reported point prevalence abstinence was calculated to be 5 per cent by intent-to-treat analysis over 4536 person-months of follow up and 10 per cent by responder analysis over 2376 person-months of follow up. The self-reported point prevalence abstinence rates at 2 years by various pre-treatment characteristics are shown in Table II for the 106 responders. Those with high HSI score (≥ 4/6) at baseline were 5 times more likely to quit than those with HSI score < 4. Those with an established cardiovascular disease (e.g. myocardial infarction or stroke) or any tobacco-attributable chronic disease (cardiovascular disease, chronic obstructive airway disease, tuberculosis, cancer or sexual dysfunction) were 80-85 per cent less likely to quit compared to those without such a previously diagnosed co-morbidity. Both these findings were significant (P< 0.05). There was however, no significant association of abstinence with other baseline characteristics such as history of previous quit attempt, history of alcohol use, nicotine dependence by FTND score, motivational stage-of-change or type of treatment that was initiated. Only about 15 per cent of patients came for ≥ 2 repeat follow up visits to the clinic. The number of these follow up visits was also not associated with successful cessation. On multivariate analysis however, no parameter was found to be associated with quitting.
Discussion
This study reports on long-term follow up outcomes of patients enrolled for tobacco cessation in a clinic-setting in India. Physicians from various departments within the hospital referred an overwhelming majority of patients and very few were ‘walk-in’ patients seeking assistance with quitting. Nearly half of our patients could not be tracked by telephone due to various reasons. It is important that this loss to telephonic follow up is differentiated from drop-out rate of clinic patients that was earlier defined as failure to return to the clinic for continued care13. Surprisingly, no drop-outs were noticed in another clinic-based setting in Delhi, northern India14. About one in four patients did not return for continued care at 2 weeks’ following treatment initiation in the earlier country-wide analysis of patients from 12 tobacco cessation clinics15.
In our study, self-reported point prevalence abstinence was found to be 5 per cent by intent-to-treat analysis and 10 per cent by responder analysis. In the nationwide analysis conducted earlier13, self-reported point prevalence abstinence at 6 wk of follow up was shown to be 16 per cent by intent-to-treat analysis over 10551 person-months follow up and 20 per cent by responder analysis over 7217 person-months of follow up. Subsequent followup at some of these clinics across the country showed quit-rates of 18 per cent at nine months15. Our two-year quit rates were slightly lower than the one-year quit rates observed by Garvey et al22 and much lower than the continuous abstinence rates of 22 per cent documented in a clinic setting in Delhi14. The recent 2009-2010 national level survey conducted as per Global Adult Tobacco Survey methodology, being a cross-sectional survey, did not obtain quit-rates but revealed quit-ratio (ratio of former smokers: current smokers expressed as a percentage) in India to be 12 per cent (and the lowest among the high-burden south and south-east Asian countries)23.
Our patients were about 10 years older than the average of 37 years seen elsewhere in India24 and in Turkey25; this could be one reason for the low quit-rate. Another reason could possibly be the poor adherence to treatment, especially in the first two weeks1326.
Though not significant on multivariate analysis, our study has highlighted certain correlates of successful point prevalence abstinence in this subset of patients – high level of nicotine dependence (estimated by the HSI) and the absence of vascular or other chronic diseases. It appears that those with high nicotine dependence but not with any overt chronic disease yet, were the sub-group of patients who benefited most from contact with a cessation clinic. FTND scores, history of alcohol consumption, previous quit attempt, duration of tobacco use, motivational stage-of-change and number of follow up visits did not appear to be predictive of successful abstinence. Type of treatment initiated, whether dichotomized into those on pharmacologic versus non-pharmacologic treatment, or by looking at four distinct treatment modalities, was also not found to be a significant predictor of outcome status. Elsewhere, lower nicotine dependence has been shown to be consistently predictive of successful quitting in clinic populations27 and in general populations28. The discrepancy between HSI and FTND was unexpected, it could possibly be because the latter may have inherent shortcomings and weak psychometric properties in some sub-populations29. While exclusive cigarette smokers were more likely to have reported quitting compared to other tobacco users, this was not found to be significant. Exclusive cigarette smokers may be an epidemiologically distinct subgroup in comparison to other smokers with regard to cessation outcomes.
We observed no difference in outcomes in our outpatient group receiving different treatment regimens similar to that noted in an extensive Cochrane review30. Others have however, documented higher quit rate among those on pharmacotherapy compared to those receiving only counselling1331. This may be due to varied clinical characteristics among patients at baseline with regard to severity of nicotine dependence and stages of motivation. Mishra et al32 also had noticed no significant differences in quit rates between those receiving pharmacologic and non-pharmacologic treatments in a campus intervention in Mumbai, western India32.
Our preliminary study had certain limitations. Firstly, the patients seen in our clinic were not representative of tobacco users in the country. They represent a sub-group of tobacco users, predominantly male smokers with moderate-to-high level of nicotine dependence and with clinical co-morbidities accessing health care services in a private, tertiary-care hospital located in an urban setting. Acknowledging this ‘selection bias’, our findings are mostly applicable to this subset of tobacco users. Secondly, there is a possibility of ‘information bias’, since cessation assessment was by self-reporting with no independent objective biochemical validation. Thirdly, only point prevalence abstinence was obtained for a duration of one month and not continuous abstinence for 6 or more months. It was also observed that there was no standard definition of abstinence in various studies in the country with abstinence duration ranging from 1 to 6 months of nil tobacco use. Lastly, failure to identify important predictors of quitting may have been limited by the small sample size and low quit-rates.
In summary, this preliminary study offers benchmarks for rates of long-term follow up and successful self-reported point prevalence abstinence in a specialty clinic out-patient setting. The patients attending this clinic were in the late 40s with two-thirds of them having high level of nicotine dependence. Though predictors of quitting have not been identified, some clinical correlates of quitting such as severity of nicotine dependence and presence of vascular or other chronic co-morbidities have been highlighted that may need to be corroborated from larger tobacco cessation centres in the country. Meanwhile, efforts at improving tobacco quit-rates and identifying predictors of quitting must continue.
Acknowledgment
The authors acknowledge the assistance of Shri Rajamani in data collection and data entry.
References
- Increasing the demand for and use of effective smoking-cessation treatments reaping the full health benefits of tobacco-control science and policy gains in our lifetime. Am J Prev Med. 2007;33(Suppl 6):S340-8.
- [Google Scholar]
- The global research neglect of unassisted smoking cessation: causes and consequences. PLoS Med. 2010;7:e1000216.
- [Google Scholar]
- U.S. DHHS (United States Department of Health and Human Services). Reducing tobacco use: A report of the Surgeon General. Atlanta (USA): U.S. DHHS, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2000.
- [Google Scholar]
- Tobacco Advertising and Promotion. In: Jha P, Chaloupka FJ, eds. Tobacco control in developing countries. Oxford (UK): Oxford University Press; 2000. p. :215-36.
- [Google Scholar]
- Global Adult Tobacco Survey (GATS). India report 2009-2010. Available from: http://www.who.int/tobacco/surveillance/gats_india/en/index.html
- [Google Scholar]
- Geographical epidemiology of cardiovascular disease in India: An exploratory study. MSc thesis (Publication No. MR67504) 2009. University of Toronto, Institute of Medical Sciences; Available from: https://tspace.library.utoronto.ca/bitstream/1807/18899/3/Mony_Prem%20kumar_200911_MSc_Thesis.pdf
- [Google Scholar]
- U.S. DHHS (United States Department of Health and Human Services). Results from the 2007 National Survey on Drug Use and Health: National Findings. Washington (DC): U.S. DHHS, US Government Printing Office; 2008.
- [Google Scholar]
- Age at initiation of tobacco use in India: a note of caution. Natl Med J India. 2011;24:247.
- [Google Scholar]
- CDC. Smoking & tobacco use: National Health Interview Surveys, Selected Years—United States, 1974–2006. Atlanta (USA): U.S. Centre for Disease Control; 2007.
- [Google Scholar]
- A nationally representative case–control study of smoking and death in India. N Engl J Med. 2008;358:1137-47.
- [Google Scholar]
- Tobacco use and dependence in Asian Americans: a review of the literature. Nicotine Tob Res. 2007;9:169-84.
- [Google Scholar]
- Poverty and chronic diseases in Asia: challenges and opportunities. CMAJ. 2007;177:1059-62.
- [Google Scholar]
- Indian experience with tobacco cessation. Report on tobacco control in India. 2004. New Delhi, India: Ministry of Health and Family Welfare, Government of India; :228-31. Available from: http://mohfw.nic.in/WriteReadData/l892s/911379183TobaccocontroinIndia_10Dec04.pdf
- [Google Scholar]
- Smoking cessation interventions and continuous abstinence rate at one year. Indian J Chest Dis Allied Sci. 2007;49:201-7.
- [Google Scholar]
- Initiating tobacco cessation services in India: challenges and opportunities. WHO South-East Asia J Public Health. 2012;1:159-68.
- [Google Scholar]
- Smoking cessation in patients with respiratory diseases: a high priority, integral component of therapy. Eur Respir J. 2007;29:390-417.
- [Google Scholar]
- Current developments in behavioral interventions for tobacco cessation. Curr Opin Psychiatry. 2010;23:151-6.
- [Google Scholar]
- Clinico-epidemiological profile of tobacco users attending a tobacco cessation clinic in a teaching hospital in Bangalore city. Lung India. 2012;29:137-42.
- [Google Scholar]
- The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86:1119-27.
- [Google Scholar]
- The Fagerström Test for Nicotine Dependence-Smokeless Tobacco (FTND-ST) Addict Behav. 2006;31:1716-21.
- [Google Scholar]
- Predicting smoking cessation with self-reported measures of nicotine dependence: FTQ, FTND, and HSI. Drug Alcohol Depend. 1994;34:211-6.
- [Google Scholar]
- Front-loaded versus weekly counseling for treatment of tobacco addiction. Nicotine Tob Res. 2012;14:578-85.
- [Google Scholar]
- Epidemiology of tobacco use, tobacco cessation and exposure to second-hand smoke in high-burden countries in south and southeast Asia. Singapore: Conference programme of the 15th World Conference on Tobacco or Health. March 20-24, 2012. Health Promotion Board; 2012.
- [Google Scholar]
- Clinic based cessation programs in India: The evidence and what it calls for. 2009. Mumbai, India: 14th World Conference on Tobacco or Health. March 8-12; Available from: http://www.14wctoh.org/abstract/abs_detail.asp?AbstractID=1026
- [Google Scholar]
- Adherence to treatment for tobacco dependence: association with smoking abstinence and predictors of adherence. Nicotine Tob Res. 2010;12:574-81.
- [Google Scholar]
- Factors associated with quitting smoking at a tobacco dependence treatment clinic. Am J Health Behav. 2006;30:400-12.
- [Google Scholar]
- Predictors of attempts to stop smoking and their success in adult general population samples: a systematic review. Addiction. 2011;106:2110-21.
- [Google Scholar]
- A review of the validity and reliability of smokeless tobacco dependence measures. Addict Behav. 2012;37:361-6.
- [Google Scholar]
- Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst Rev. 2007;3:CD001837.
- [Google Scholar]
- Clinical trial comparing nicotine replacement therapy (NRT) plus brief counselling, brief counselling alone, and minimal intervention on smoking cessation in hospital inpatients. Thorax. 2003;58:484-8.
- [Google Scholar]
- Call centre employees and tobacco dependence: making a difference. Indian J Cancer. 2010;47(Suppl 1):43-52.
- [Google Scholar]






