Translate this page into:
A preliminary study on virulence factors & antimicrobial resistance in extra-intestinal pathogenic Escherichia coli (ExPEC) in Bangladesh
*For correspondence: fakruddinmurad@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Escherichia coli is a commensal organism inhabiting human and animal intestinal tract and can cause a variety of extra-intestinal infections when enters into unnatural sites1. The ability of E. coli to cause extra-intestinal infections depends largely on several virulence factors which help to survive under adverse conditions2. E. coli strains that induce extra-intestinal infections are termed as extra-intestinal pathogenic E. coli (ExPEC)3. In terms of morbidity and mortality, ExPEC has a great impact on public health, with an economic cost of several billion dollars annually4. Production of enterotoxins, haemolysins, colicins, haemagglutinins, proteases, colonization factors, cell surface hydrophobicity, etc. are some of the virulence-associated factors of E. coli5.
As E. coli infection involving the urinary tract, peritoneum, blood and meninges occur frequently in our country, a comprehensive study on the virulence factors of these bacterial strains is urgently required. The treatment of E. coli infections is increasingly becoming difficult due to development of resistance against antibiotics6. Therefore, it is necessary to know the antibiotic susceptibility pattern of pathogenic E. coli to select the correct antibiotic(s) for the proper treatment of the infections1. Identification of virulence factors is important in understanding bacterial pathogenesis and their interactions with the host, which may also serve as novel targets in drug and vaccine development2. Capacity of E. coli to produce multiple virulence factors may conbtribute to its pathogenicity in extra-intestinal infections1. These virulence factors enable some members of the normal flora to elicit an infection by overcoming the host defence mechanisms7. Here we report virulence factors and antimicrobial resistance in E. coli isolates obtained from extra-intestinal sites of infected patients in Bangladesh.
The study was carried out in the microbiology laboratory of Bangladesh Council of Scientific & Industrial Research (BCSIR) Laboratories, Chittagong, Bangladesh from March to November 2011. E. coli strains isolates from patients with septicemia, UTI, meningitis, peritonitis and abscess were included in this study. All the strains were previously isolated and presumptively identified in Chittagong Medical College Hospital, Bangladesh and their identity were confirmed in the microbiology laboratory of BCSIR, Chittagong.
A total of 65 clinical isolates of E. coli, of which 25 were from infected urine patients, 12 from peritoneal fluid of peritonitis patients, 12 from blood of septicemia patients, 10 from pus and 6 from cerebrospinal fluid (CSF) of meningitis patients were included in the study. E. coli (n=15) isolated from stool of healthy individuals (staff and attendants) were included as control. All the isolates were identified and determination of virulence properties such as haemolytic activity, colicin production, haemagglutination, mannose sensitivity, mesurement of cell surface hydrophobicity and protease production was performed according to standard procedure89. Antibiotic susceptibility against some common antibiotics (tetracycline, streptomycin, cephotaxime, ceftriaxone, trimethoprim-sulfamethoxazole, ampicillin, chloramphenicol, ceftazidime, gentamycin, penicillin, nitrofurantoin, cefradine polymixin B and nalidaxic acid)9 was also performed10.
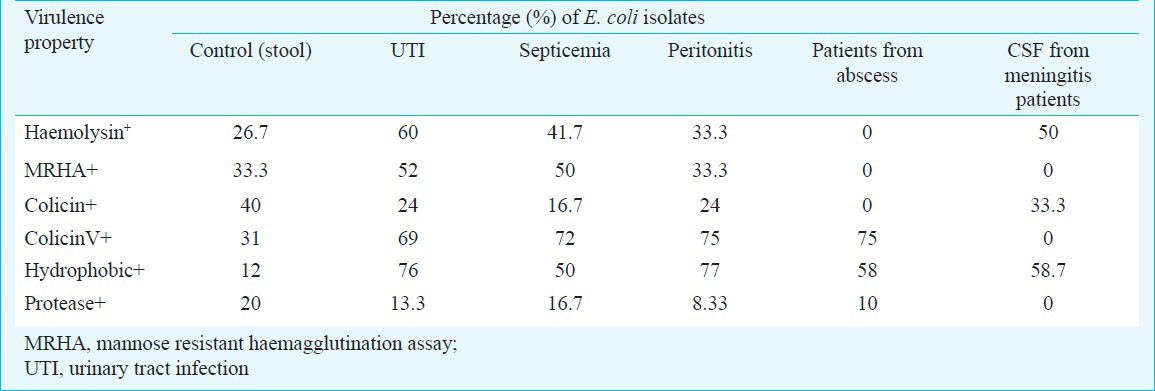
Of the 65 extra-intestinal E. coli isolates tested, 44.6 per cent were haemolytic. Of the 25 E. coli isolates from urine, 15 (60%) were haemolytic indicating the importance of haemolysin in the pathogenesis of urinary tract infection7. Haemolytic E. coli isolates may also at an advantage in producing septicemia as in this study 41.6 per cent (5/12) of the septicemic E. coli isolates were haemolytic. Nine (9) isolates from pus (4) and peritoneal fluid (5) were also haemolytic indicating that these may contribute to tissue injury1. Among the extra-intestinal pathogenic E. coli isolates, only the urinary and blood isolates produced colicin V. Six (24%) urinary and two (16.7%) blood isolates showed colicin V activity. None of the E. coli isolates from peritoneal fluid gave positive reaction in mannose resistant haemagglutination (MRHA) assay7. Possession of mannose resistant haemagglutinin was found significant in the urinary isolates. Surface hydrophobicity is an important virulence factor of E. coli that causes extra-intestinal infections. E. coli isolates with salt aggregation test (SAT) value ≤2.0 M were described as hydrophobic while those with ≥3.0 M as less hydrophobic. Source-wise analysis of the clinical isolates of E. coli indicated that the urinary and the peritoneal isolates were the most hydrophobic as shown earlier11. Blood isolates had relatively high SAT values justifying the minor role of cell surface hydrophobicity in pathogenesis of septicemia. All MRHA positive E. coli isolates had SAT value ≤1.0 M. In this study both clinical (6) or faecal (3) isolates of E. coli produced extracellular protease and hence it can be presumed to be a minor virulence factor for E. coli infection. Some of the extra-intestinal E. coli isolates did not possess any of the virulence factors studied yet caused infections. May be these isolates induced infections in immuno-compromised hosts or these might possess properties different from those included in this study. Distribution of virulence phenotypes in the extra-intestinal E. coli isolates are shown in the Table.
Most of the haemolysin and MRHA positive E. coli were also hydrophobic which is in accordance of earlier findings12. Though virulence of an organism cannot be accurately predicted on the basis of its measurable virulence phenotype, the expression of multiple virulence factors functions effectively or synergistically in overcoming normal host defences1. Forty one (63.07%) isolates were resistant to 2 or more of the most commonly used antibiotics, 55 (85%) was resistant to ampicillin, 44 (73%) were resistant to tetracycline, 50 (77%) to streptomycin, 44 (69%) to penicillin, while 38 (59.0%) and 29 (44.5%) isolates were resistant to sulphamethoxazole-trimethoprim and chloramphenicol, respectively. The third-generation cephalosporin (ceftriaxone, ceftazidime and cefotaxime) and polymyxin B were found to be most effective against ExPEC. Other drugs that appeared to be clinically useful were the first-generation cephalosporin (cephradine), nalidixic acid, gentamycin and nitrofurantoin. The presence of multidrug resistance may be related to the dissemination of antibiotic resistance among hospital isolates of E. coli.
From the data obtained in this study, it seemed probable that haemolysin production, MRHA of human type O erythrocytes and hydrophobic cell surface might be the important characteristics that enabled E. coli to cause extra-intestinal infections. Study on other characteristics, such as resistance to human serum, cytotoxin production, possession of aerobactin iron-acquisition system and adherence to uroepithelium might reveal the virulence determinants of the isolates that were otherwise negative for all the characteristics studied. Further study involving a large number of E. coli isolates obtained from patients with septicemia, peritonitis, abscess and meningitis would be necessary before any factor could be implicated for the virulence of E. coli infection at the extra-intestinal sites and also for better understanding of interaction of different virulence factors at molecular level.
References
- Virulence factors and drug resistance in Escherichia coli isolated from extra-intestinal infections. Indian J Med Microbiol. 2007;25:369-73.
- [Google Scholar]
- Extraintestinal infections due to Escherichia coli: An emerging issue. J Clin Diag Res. 2011;5:486-90.
- [Google Scholar]
- Proposal for a new inclusive designation for extraintestinal pathogenic isolates of Escherichia coli ExPEC. J Infect Dis. 2000;181:1753-4.
- [Google Scholar]
- Medical and economic impact of extraintestinal infections due to Escherichia coli: focus on an increasingly important endemic problem. Microbes Infect. 2003;5:449-56.
- [Google Scholar]
- Virulence factors, serotypes and antimicrobial suspectibility pattern of Escherichia coli in urinary tract infections. Al Ameen J Med Sci. 2009;2:47-51.
- [Google Scholar]
- Prevalence of ESBL producing gram negative bacteria in a tertiary care hospital. Indian J Med Res. 2002;115:153-7.
- [Google Scholar]
- Virulence factors of uropathogenic Escherichia coli. Int J Antimicob Agents. 2003;22:29-33.
- [Google Scholar]
- The comparison between virulence factors of Escherichia coli isolated from urinary tract infections and faecal flora. Res Pharm Sci. 2007;2:99-103.
- [Google Scholar]
- Comparison of virulence factors among clinical isolates of Pseudomonas aeruginosa producing and non-producing extended spectrum β-lactamases. Curr Res Bacteriol. 2011;4:85-93.
- [Google Scholar]
- Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966;45:493-6.
- [Google Scholar]
- Bacterial adherence and immune response in recurrent UTI. Int J Gynaecol Obstet. 2001;75:263-8.
- [Google Scholar]
- Serum resistance among Escherichia coli strains causing urinary tract infection in relation to O type and the carriage of haemolyisn, colicin and antibiotic resistance determinants. Infect Immun. 1982;35:270-5.
- [Google Scholar]





