Translate this page into:
Prevention of non-communicable diseases requires a life course approach: A case study from Kerala
+For correspondence: sivasct@hotmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Introduction
Kerala is the most advanced Indian State in terms of epidemiological transition and has the highest prevalence of most of the non-communicable diseases (NCD) and risk factors12. It is the diabetic capital for India with a prevalence of 14.8 per cent in the age group of 15-64 yr and the age adjusted cardiovascular mortality is twice that of the United States34. The men: women ratio of acute coronary syndrome (ACS) admissions in Kerala decreased from 23:1 in 1967 to 4:1 in 2007 indicating an increase of ACS among women56. Similarly, age-adjusted breast cancer incidence has shown an increasing trend in pre-menopausal women7. As this could be a harbinger of what will happen in the future to the rest of India and similar developing countries, it is important to understand the NCDs and their risk factors in this south Indian State.
Onset of risk factors is early in life
In Kerala, NCD risk factors start early in life. Despite good maternal and child health care services, Kerala reported 16.1 per cent low birth weight babies and 26.5 per cent childhood stunting below the age of three years in 2005-20068. Kerala also has the highest prevalence of overweight and obese women in the reproductive age group in India8. In a community based study, all the 2.9 per cent people detected with diabetes in the age group of 15-24 yr were women2. Normal weight children in Kerala were reported to have the highest mean systolic and diastolic blood pressure globally9. More than 50 per cent of children at 16 yr had high density lipoprotein (HDL) cholesterol less than normal (45 mg/dl)10.
Obesogenic environment in Kerala
Kerala with its high population density of 859 people per square kilometers ranks low in agricultural productivity and compared to the rest of India, consumes double the marketed products high in salt, sugar and saturated fat11. The majority of these marketed products are also rich in trans-fats12. The unique secular nature of this Indian State encourages participation in religious and family functions where energy dense fried foods, rich in sugar, salt and meat products, are offered free and consumed in large amounts13. Only 54.8 per cent of Kerala consume green leafy vegetables more than once a week while 82.8 per cent of the people consume at least one non-vegetarian dish a day14. The nutrition transition in Kerala over the last three decades is characterized by a positive energy balance driven by marketed products15. Per capita calorie consumption in Kerala increased from 1600 Kcals to more than 2200 Kcals per day over this same period, when energy needs steadily declined because of mechanization at the work place and increasing sedentary lifestyle15. Kerala now leads all the Indian States in consumer product consumption (television, motor vehicles, etc.)16. Control of infectious diseases (e.g. acute diarrhoeal diseases and vaccine preventable diseases) reduced the energy cost of infections15. In Kerala (being in the tropical equatorial zone) less energy is needed to maintain body temperature. The decline in total fertility rate from 2.27 in the year 1962 to 1.7 in 2003 further increased the positive energy balance in women17.
In a statewide study among 2.3 million school children aged 10-15 yr, where only 11.5 per cent of girls could finish the recommended health related physical fitness test compared to 16.58 per cent in boys18. The high prevalence of cardio-metabolic risk factors in women in the reproductive age group is detrimental to their future health as well as to their children because of the in utero programming of adult onset diseases19. Vitamin D deficiency is reported to be universal in Kerala and India20. The need for exposure of 40 per cent of body to the sun for two hours daily to maintain adequate vitamin D levels is not easy because of the socio-cultural practice of covering almost the entire body with clothes and restricting outdoor physical activity in girls21. These factors have contributed to a double jeopardy of vitamin D deficiency and declining bone (osteopenia) and muscle mass (sarcopenia)21.
The pathway leading to a vicious cycle of high NCD risk factors
Survival of low birth weight (LBW) babies in Kerala is substantially higher compared to the rest of India15. Infant mortality rates in Kerala were the lowest in India. It reached a level of 10-15 per 1000 live births in the early 1990s and has remained in that range over the past 20 years22. The LBW babies were exposed to the obesogenic environment and were often overprotected by their educated parents who fed them more energy rich foods and restricted physical activity. LBW babies, at birth are known to have less beta cell potential, muscle mass, nephron numbers, and more endothelial dysfunction and higher proportion of body fat making them more susceptible to NCD risk factors23.
The restriction of outdoor physical activity in girls and women decreases endogenous vitamin D synthesis and imparts a low body skeletal muscle mass and high fat body composition. Skeletal muscle constitutes the best insulin sensitive tissues in the body24. This has resulted in increasing metabolic risk factors in women in the reproductive age group through increasing blood pressure, dysglycemia and declining vitamin D levels. Like maternal dysglycemia, micronutrient and vitamin deficiency is a documented precursor of adult onset diseases in the offspring as demonstrated by follow up studies in south India2526. Some normal weight children, when abnormally programmed in utero due to maternal dysmetabolism, are predisposed to developing NCD risk factors in later life at a rate similar to that of LBW babies19. Persistence of high level childhood stunting, irrespective of positive energy balance in the society, is an important indicator that factors other than undernutrition, like maternal dys-metabolism could be responsible for the abnormal growth pattern of children in Kerala8151923. This Kerala case study is a good illustration of how the early onset of NCD risk factors in the reproductive age group adversely affects the health status of women and their children. Low birth weight babies are thin, not because of lack of fat, but because of less skeletal muscle27. Encouraging sun exposure and adequate physical activity in adolescent girls is the best prescription to break this vicious cycle of maternal dysmetabolism predisposing to early onset of NCD risk factors in their children22. The interaction of nutrition and physical activity along the life course of metabolic endocrine programming is depicted in the Figure. The six major factors which can tip the balance towards sarcopenia (less skeletal muscle) and metabolic syndrome are early life programming, puberty, pregnancy, inflammation/drugs, menopause, and old age. The five major outcomes in the spectrum are represented along the dotted like labelled with bold italic letters. The best adapted people are the aboriginal people followed by athletes, and then the obese metabolically healthy people. But the majority of the population moves to metabolic syndrome, and those who are abnormally programmed in early life evolve into metabolically obese normal weight individuals.
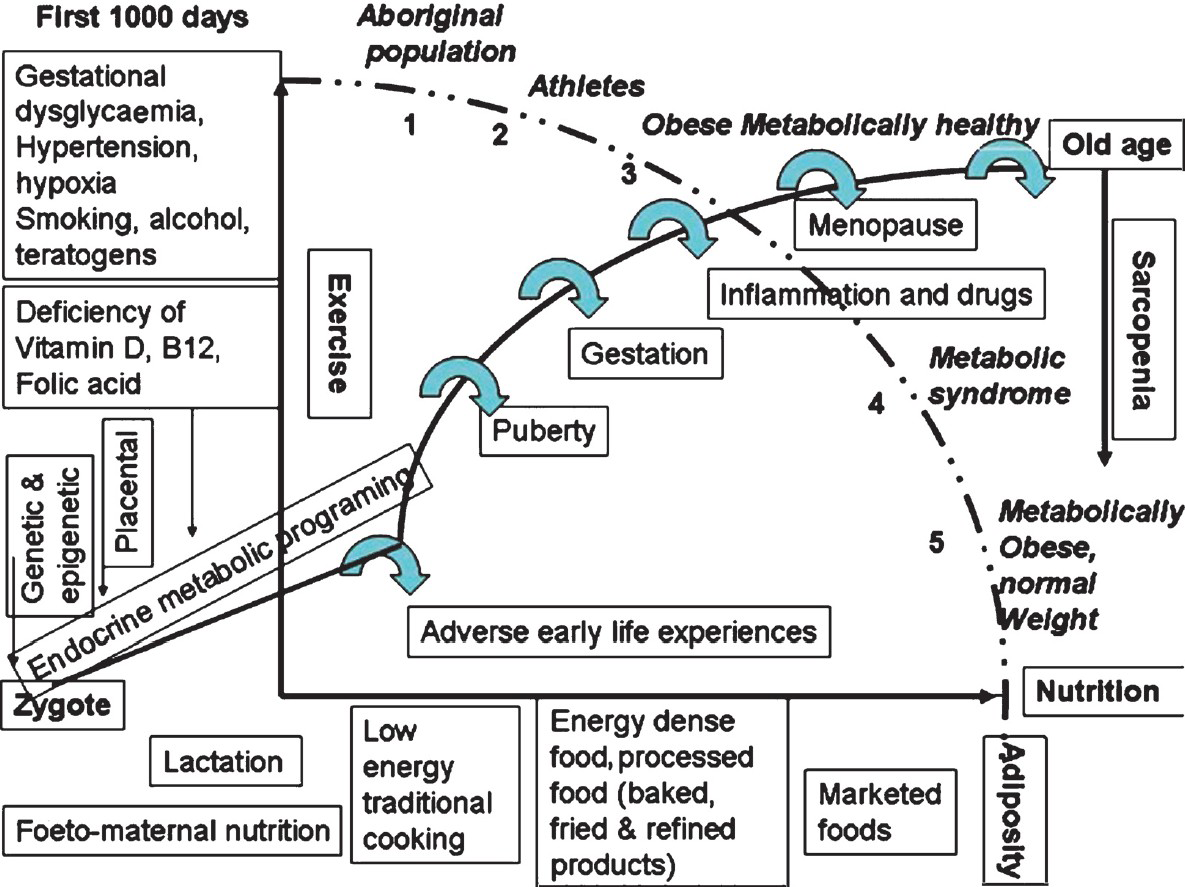
- Body response to obesogenic environment across the life cycle. The dark line connecting the zygote to old-age represents the endocrine metabolic programming. The X axis represents the various sources of nutrition. Exercise the major modulator of response after the first 1000 days is represented in the Y axis. The six major factors favouring sarcopenia (less skeletal muscle) are depicted by broad curved arrows. The five major outcomes are labelled along the dotted line with bold italic letters. Adverse early life programming manifests as metabolically obese normal weight individuals (5).
Future directions
NCD prevention should be paid particular attention in adolescents to achieve a balanced body growth and composition focusing on physical activity and a healthy diet. The mother and child health programmes need to be redefined to achieve a healthy mother with good body composition and metabolic milieu. Women's heart is more vulnerable to behavioural risk factors such as tobacco, alcohol and physical inactivity which formed the basis for the “Go Red for Women” by the American Heart Association28. Although this campaign started in the west for adult women, it is also pertinent for women in the reproductive age group in places such as Kerala. The fruits of better women's education in Kerala that paved the way for the Kerala model of “good health at low cost” need to be expanded to include physical activity and a healthy diet22. Another factor that might arise at a later time is tobacco use. Although current tobacco consumption is negligible among adolescent girls in Kerala, control programmes are essential to prevent the initiation of this unhealthy practice. The Political Declaration of the UN High Level Meeting on NCDs in September 2011 provides an excellent opportunity to address these issues29. Since a life course approach is required for the prevention and control of NCDs, healthy diet, physical activity and tobacco control may need to be integrated into the already existing maternal and child health programmes.
Acknowledgment
The first author (SS) was mentored in non communicable disease epidemiology at the Rollins School of Public Health under a grant number 1 D43 HD065249 from the Fogarty International Center and the Eunice Kennedy Shriver National Institute of Child Health and Human Development at the National Institutes of Health.
References
- Lumping and splitting: the health policy agenda in India. Health Policy Plann. 2003;18:249-60.
- [Google Scholar]
- Risk factor profile for chronic non-communicable diseases: results of a community-based study in Kerala, India. Indian J Med Res. 2010;131:53-63.
- [Google Scholar]
- Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125:217-30.
- [Google Scholar]
- All-cause mortality and cardiovascular mortality in Kerala State of India: Results from a 5-year follow-up of 161 942 rural community dwelling adults. Asia Pac J Public Health. 2010;23:896-903.
- [Google Scholar]
- Acute myocardial infarction in north Kerala - a 20 year hospital based study. Indian Heart J. 1991;43:93-6.
- [Google Scholar]
- The clinical spectrum of acute coronary syndromes: experience from a major center in Kerala. J Assoc Physicians India. 2009;57:377-83.
- [Google Scholar]
- An epidemiological assessment of increasing incidence and trends in breast cancer in Mumbai and other sites in India, during the last two decades. Asian Pac J Cancer Prev. 2003;4:51-6.
- [Google Scholar]
- International institute for population studies (IIPS) and ORC macro 2006. National Family Health Survey 3 (NFHS-3) India, Kerala report 2005-2006. Available from: http://hetv.org/india/nfhs/nfhs3/NFHS-3-Kerala-state-report.pdf
- [Google Scholar]
- Markers of fetal onset adult diseases: a comparison among low birthweight and normal birthweight adolescents. Indian Pediatr. 2009;46(Suppl):s43-7.
- [Google Scholar]
- Broadening waist line of Keralites, the diet link. Chapter 30. In: Kartha CC, ed. Kerala Fifty Years and Beyond. Trivandrum: Gautha Books; 2007. p. :307-44.
- [Google Scholar]
- Trans fats - sources, health risks and alternative approach - A review. J Food Sci Technol. 2011;48:534-41.
- [Google Scholar]
- Correlation of regional cardiovascular disease mortality in India with lifestyle and nutritional factors. Int J Cardiol. 2006;108:291-300.
- [Google Scholar]
- “Eating, eating is always there”: food, consumerism and cardiovascular disease. Some evidence from Kerala, south India. Anthropol Med. 2010;17:261-75.
- [Google Scholar]
- Health Transition in Kerala (working paper). 1999 Working paper 10: Kerala research program on local level development. 1999. 1- 44 (Centre for development studies, Thiruvananthapuram, India. Available from: http://www.cds.ac.in/krpcds/publication/panikar.html
- [Google Scholar]
- National Sample Survey Organization (NSSO) In: Key Indicators of household consumer expenditure in India 2009-10. New Delhi: Ministry of Statistics and Program Implementation, Government of India; 2011.
- [Google Scholar]
- Kerala State Sports Council report to the government on total physical fitness program test results on school children. Free e-book. Available from: http://ebookbrowse.com/tpfp-reportenglish-pdf-d62129176
- [Google Scholar]
- Influence of maternal dysmetabolic conditions during pregnancy on cardiovascular disease. J Cardiovasc Transl Res. 2009;2:277-85.
- [Google Scholar]
- Vitamin D status in India - its implications and remedial measures. J Assoc Physicians India. 2009;57:40-8.
- [Google Scholar]
- Effects of sports training & nutrition on bone mineral density in young Indian healthy females. Indian J Med Res. 2011;134:307-13.
- [Google Scholar]
- A critical evaluation of the fetal origins hypothesis and its implications for developing countries. J Nutr. 2004;134:191-3.
- [Google Scholar]
- Evolution, body composition, insulin receptor competition, and insulin resistance. Prev Med. 2009;49:283-5.
- [Google Scholar]
- Maternal vitamin D status during pregnancy and body composition and cardiovascular risk markers in Indian children: the Mysore Parthenon Study. Am J Clin Nutr. 2011;93:628-35.
- [Google Scholar]
- Low plasma vitamin B12 in pregnancy is associated with gestational “diabesity” and later diabetes. Diabetologia. 2009;52:2350-8.
- [Google Scholar]
- Neonatal anthropometry: the thin-fat Indian baby. The Pune Maternal Nutrition Study. Int J Obes Relat Metab Disord. 2003;27:173-80.
- [Google Scholar]
- UN high-level meeting on non-communicable diseases: addressing four questions. Lancet. 2011;378:449-55.
- [Google Scholar]





