Translate this page into:
Early diagnosis of typhoid fever by nested PCR for flagellin gene of Salmonella enterica serotype Typhi
Reprint requests: Dr B.N. Harish, Professor, Department of Microbiology, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry 605 006, India e-mail: drbnharish@yahoo.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Typhoid fever caused by Salmonella Typhi continues to be a major health problem in spite of the use of antibiotics and the development of newer antibacterial drugs. Inability to make an early laboratory diagnosis and resort to empirical therapy, often lead to increased morbidity and mortality in cases of typhoid fever. This study was aimed to optimize a nested PCR for early diagnosis of typhoid fever and using it as a diagnostic tool in culture negative cases of suspected typhoid fever.
Methods:
Eighty patients with clinical diagnosis of typhoid fever and 40 controls were included in the study. The blood samples collected were subjected to culture, Widal and nested PCR targeting the flagellin gene of S. Typhi.
Results:
The sensitivity of PCR on blood was found to be 100 per cent whereas the specificity was 76.9 per cent. The positive predictive value (PPV) of PCR was calculated to be 76.9 per cent with an accuracy of 86 per cent. None of the 40 control samples gave a positive PCR.
Interpretation & conclusions:
Due to its high sensitivity and specificity nested PCR can be used as a useful tool to diagnose clinically suspected, culture negative cases of typhoid fever.
Keywords
Flagellin gene
nested PCR
Salmonella Typhi
Typhoid fever has a global presence. Worldover 17 million people are affected annually by typhoid fever and 600,000 succumb to it1. In India, the incidence of culture proven typhoid fever is 980 cases/100,000 population/year2. The clinical diagnosis of typhoid fever has been a medical challenge due to its similarities to other febrile illnesses. The outcome of blood culture is limited by the previous use of antibiotics and a low bacterial load3. Widal test, the commonly used serological test is positive only in the later part of the disease. Moreover, its interpretation in endemic areas is fraught with its own disadvantages.
PCR is a sensitive and specific method used for the diagnosis of a number of infectious diseases. In typhoid fever it can be an effective tool because it can be used even in cases where antibiotic therapy has been started or the pathogen load is very low. A nested PCR makes the detection more sensitive and is able to detect the presence of even 3-5 bacilli4. Therefore, an attempt was made to optimize nested PCR in our laboratory and the possibility of using it as a diagnostic tool in culture negative cases of typhoid fever was explored.
Material & Methods
This study was carried out between August 2007 and July 2009 on blood samples from patients hospitalized in Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER) Hospital and Government General Hospital, Puducherry. Eighty consecutive patients both sexes and all age groups with clinical diagnosis of typhoid fever were included in the study. This was based on information from previous studies to decide the sample size.
The control group (n=40) matched for age and sex consisted of 30 individuals with no history of fever or any Gram negative bacterial infection in the recent past. It also included two patients whose blood culture had grown Escherichia coli, two patients with Klebsiella pneumoniae septicaemia, and three patients each whose blood culture had grown S. Paratyphi A and Group B Salmonella.
Blood samples from these patients, 30 healthy individuals and 10 with septicaemia, were included to ensure the specificity of nested PCR. Samples from this group were collected for PCR after taking informed consent. Patients with fever who were positive by other febrile agglutination test i.e. standard agglutination test (SAT) for Brucellosis and Microscopic Agglutination Test (MAT) for leptospirosis were excluded from the study. Pure cultures of Salmonella Typhi H901, maintained in our laboratory were used for the standardization of PCR. Ethical committee approval was obtained for the study.
Ethics committee of JIPMER approved the study protocol.
Isolation of S. Typhi from blood culture: A biphasic medium consisting of brain heart infusion (BHI) agar and BHI broth with sodium polyanethol sulphonate as an anticoagulant was used for blood cultures. Blood (5 ml) was inoculated in 50 ml of this media. The bottles were screened daily for growth. Any colony obtained on subculture was identified by standard means5. The identification was confirmed by using Salmonella Polyvalent O, O9 and dH antisera (Denka Seiken Co Ltd, UK).
Widal test: The Widal test was performed within 24 h of collection of samples. A dilution of >1 in 80 for TO and >1 in 160 for TH was considered suggestive of typhoid fever6.
Polymerase chain reaction: PCR was done on whole blood taken from 80 patients in the study group and 40 healthy individuals and 10 with infection in control group. Pure cultures of Salmonella Typhi H901 were used for the standardization of PCR. These were subcultured on nutrient agar and were verified by biochemical and serological tests7.
DNA was extracted from the culture by the colony PCR method8. A single colony of the organism was suspended in 100 μl of Milli Q water in a micro centrifuge tube and boiled at 100°C for 5 min. Following this it was centrifuged at 9,500 g for 5 min. The supernatant was decanted and used as a template for PCR6.
Extraction of DNA from blood samples was done by a method described earlier4 with several modifications. One ml of blood containing 20 mM potassium EDTA as anticoagulant was centrifuged at 9,500 g for 5 min. One ml of lysis buffer (0.2% Triton X100 in Tris HCl, pH 8.0) was added to the pellet. The mixture was gently aspirated several times to effect haemolysis. The tube was centrifuged at 12879 g for 6 min, the supernatant was discarded, and the procedure was repeated several times till a clear white pellet was observed. The pellet was washed twice with distilled water. After the removal of the supernatant, the pellet was resuspended in 20-30 μl of distilled water. The tubes were sealed, kept in boiling water for 20 min, and brought back to room temperature before being used as a template for PCR4.
Nested PCR protocol: Primers targeting the flagellin gene of Salmonella Typhi were used910 after verifying against the database in the GenBank [GenBank accession no.(AC): L21912]. Oligonucleotides ST1 (5’- TATGCCGCTACATATGATGAG -3’) and ST2 (5’-TTAACGCAGTAAAGAGAG-3’), which were used for regular PCR to amplify a 497 bp fragment, corresponded to nucleotides 1024-1044 and 1504-1521, respectively, in the flagellin gene of S. Typhi. For nested PCR, oligonucleotides ST3 (5’- ACTGCTAAAACCACTACT -3’) and ST4 (5’-TGGAGACTTCGGTTGCGTAG-3’) were used to amplify a 366 bp fragment corresponding to nucleotide 1060-1077 and 1407-1426 [(AC): L21912]. For regular PCR, a 25 μl amplification mixture containing 10μl of commercial master mix (Bangalore Genei, Bangalore), 7 μl of MilliQ water, 2 μl ST1 and 2 μl ST2 primers with 4 μl of the extracted DNA were used. The reaction was carried out in an Eppendorf Mastercycler (Eppendorf, Germany). The reaction mixture was subjected to 40 cycles of 2 min each at 94°C for denaturation followed by annealing at 57°C for 1 min 15 sec and elongation at 72°C for 1 min. A final elongation for 7 min was done at 72°C. For nested PCR, a 25 μl amplification mixture containing 10 μl of commercial master mix (Bangalore Genei, Bangalore), 7 μl of MilliQ water, 2 μl ST3 and 2 μl ST4 primers with 4 μl of the 1 in 5 diluted amplified product from the regular PCR was used. Amplification conditions were similar to the first round PCR with the exception that annealing was done at a higher temperature at 68°C for 1 min 15 sec.
Following PCR, the products were loaded onto agarose gels. A reaction mixture of 6 μl was fractionated electrophoretically at 80V for 1 h in a 2.5 per cent agarose gel containing 0.5 μg of ethidium bromide. Electrophoresis was performed in an electrophoresis unit (Pharmacia Biotech, Sweden). A positive control representing at least 5 bacteria/ml and a negative control without any DNA were also included in each lot4. A 100 bp DNA ladder (Fermentas, Germany) was included to determine the size of the fragments. All gels were documented using a gel documentation system. (Vilber Lourmat, France).
Nested PCR amplicon sequencing to confirm the identity of the flagellin (fliC) gene of S. Typhi: The nested PCR amplicon was sequenced to confirm the identity of the flagellin (fliC) gene of S. Typhi. The sequencing was carried out commercially (Cistron Bioscience, Sequencer-Applied Biosystems, Chennai, India).
Statistical analysis: Fisher's exact test was used to find the significance of study parameters on categorical scale between two groups. Two-tailed P values were calculated using the Fisher's test. Diagnostic statistics viz. sensitivity, specificity, positive and negative predictive values (PPV, NPV) and accuracy have been computed to find the association of PCR and Widal test in relation to blood culture as gold standard. The Statistical software SPSS 15.0 (SPSS Inc, Chicago, III), Stata 8.0 (StataCorp, College Station, Tex), MedCalc 9.0.1 (MedCalc Software bvba, Mariakerke, Belgium), Graphpad and Systat 11.0 were used for the analysis of the data.
Results
Among the 80 patients included in this study, blood cultures of 40 patients grew S. Typhi. In the remaining 50 per cent, a clinical suspicion of typhoid fever could not be confirmed in the absence of a positive culture report. The nested PCR done on blood samples of 80 patients for flagellin gene of S. Typhi was positive in 52 patients. A 366 bp amplified product was detected at the end of nested PCR. The blood samples from the control group consisting of 30 healthy individuals were negative for flagellin gene by PCR. Nested PCR performed on blood samples from two patients positive for E. coli culture, two for K. pneumoniae septicaemia, and three patients each with S. Paratyphi A and Group B Salmonella was also negative. Negative test results in blood culture and PCR were obtained in 28 patients.
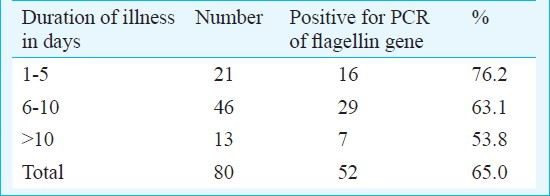
The nested PCR for flagellin gene of S. Typhi gave a sensitivity of 100 per cent and a specificity of 76.9 per cent. The positive predictive value (PPV) of PCR was calculated to be 76.9 per cent with an accuracy of 86 per cent. The results by PCR were statistically significant (P<0.001) (Table I). PCR could diagnose additional 28.2 per cent of cases as compared to blood culture. The PCR showed a positivity of 76 per cent in the first week of illness and 54 per cent in the second week (Table II).
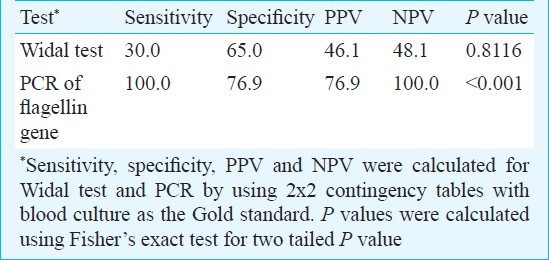
Widal showed a sensitivity of 30 per cent and a specificity of 65 per cent (Table I). It was positive in 9 cases where both blood culture and PCR were negative. A repeat Widal done in these cases showed negative results.
Discussion
As blood culture is considered the gold standard for diagnosis of typhoid fever, the standardized nested PCR for flagellin gene of S. Typhi was evaluated against blood culture. Blood culture has a sensitivity of 45-70 per cent in the first week of illness11. Most other studies have reported a sensitivity of blood culture for S. Typhi ranging from 45-70 per cent11.
In this study, nested PCR for flagellin gene of S. Typhi gave a sensitivity of 100 per cent and a specificity of 76.9 per cent. Earlier studies done on PCR for flagellin gene of S. Typhi have reported a sensitivity and specificity to a similar effect (100% sensitivity and 97% specificity)12.
With nested PCR, 12 patients with typhoid fever could be diagnosed whose blood cultures were sterile. Thus PCR could diagnose additional 28.2 per cent of cases as compared to blood culture. However, due to the lack of a standard test against which the results of PCR could be compared, the validity of the test was not established.
A retrospective analysis of the results of this study was done to determine the potential of nested PCR as an early diagnostic tool. In comparison to blood culture, PCR could diagnose 76.2 per cent of the cases during the initial 1-5 days of illness. Only 61.9 per cent of the blood cultures grew S. Typhi in this age group. For patients presenting with an illness of 6-10 days duration, PCR could detect 63.1 per cent of the cases as compared to the 45.6 per cent positive blood cultures.
Even in the later stages of the disease, the detection of cases by PCR was slightly higher than blood culture (53.8 vs 46.1%). These values, though statistically insignificant, show that PCR can be used as a diagnostic tool in any stage of the disease.
It is known that empirical antibiotic therapy affects the isolation rate of blood culture in typhoid fever13. However, a nested PCR can be used as an effective diagnostic test even when antibiotics have been started.
A comparison of blood culture and Widal test showed that of the 40 blood samples which had grown S. Typhi, only 18 were positive by Widal (45%). An early sampling in these cases detected the bacteria but the antibody response could not be picked up by Widal. Conversely, a “positive” Widal test may be seen in non-typhoidal patients and healthy controls from endemic areas. Studies have reported varied specificities ranging from 53 to 92 per cent14. Widal test not only fails to identify culture positive cases but also gives a number of false positive results. Widal showed a sensitivity of 30 per cent and a specificity of 65 per cent in the present study. It was positive in 9 cases where both blood culture and PCR were negative. The anti TO and anti TH antibody titres in these cases were elevated ranging from 1 in 160 through 1 in 640. Widal is considered a non specific test especially in endemic regions where the resident population already has antibodies against S. Typhi15. The present study was conducted in such an endemic region. Among the study group, 28 cases positive by blood culture were negative by Widal, showing the redundancy of a single Widal test result14.
In conclusion, due to its high sensitivity and specificity nested PCR can serve as a useful tool to diagnose clinically suspected, culture negative cases of typhoid fever.
References
- Antimicrobial resistance in typhoidal salmonellae. Indian J Med Microbiol. 2011;29:223-9.
- [Google Scholar]
- Putting typhoid vaccination on the global health agenda. N Engl J Med. 2007;357:1069-71.
- [Google Scholar]
- Relative efficacy of blood, urine, rectal swab, bone-marrow, and rose-spot cultures for recovery of Salmonella typhi in typhoid fever. Lancet. 1975;1:1211-3.
- [Google Scholar]
- Early detection of typhoid by polymerase chain reaction. Ann Saudi Med. 1999;19:337-40.
- [Google Scholar]
- Determination of baseline widal titers from Chandigarh. Indian J Med Microbiol. 2003;21:144.
- [Google Scholar]
- Tests for the identification of bacteria. In: Collee JG, Fraser AG, Marimion BP, eds. Mackie and McCartney practical medical microbiology (14th ed). London: Churchill Livingstone; 2011. p. :131-49.
- [Google Scholar]
- PCR-based restriction fragment length polymorphism typing of Helicobacter pylori. J Clin Microbiol. 1994;32:331-4.
- [Google Scholar]
- Detection of Salmonella typhi in the blood of patients with typhoid fever by polymerase chain reaction. J Clin Microbiol. 1993;31:1439-43.
- [Google Scholar]
- Unique sequences in region VI of the flagellin gene of Salmonella typhi. Mol Microbiol. 1989;3:1379-83.
- [Google Scholar]
- Evaluation and comparison of different blood culture techniques for bacteriological isolation of Salmonella typhi and Brucella abortus. J Clin Microbiol. 1995;33:868-71.
- [Google Scholar]
- Standardisation of polymerase chain reaction for the detection of Salmonella typhi in typhoid fever. J Clin Pathol. 1997;50:437-9.
- [Google Scholar]
- Relative efficacy of blood, urine, rectal swab, bone-marrow, and rose-spot cultures for recovery of Salmonella typhi in typhoid fever. Lancet. 1975;1:1211-3.
- [Google Scholar]
- The Widal test in the diagnosis of typhoid fever in the transvaal. S Afr Med J. 1981;59:851-4.
- [Google Scholar]
- Use of paired serum samples for serodiagnosis of typhoid fever. J Clin Microbiol. 2005;43:4889-90.
- [Google Scholar]






