Translate this page into:
Spectrum of malabsorption syndrome among adults & factors differentiating celiac disease & tropical malabsorption
Reprint requests: Dr Uday C. Ghoshal, Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226 014, India e-mail: udayghoshal@gmail.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Aetiology of malabsorption syndrome (MAS) differs in tropical and temperate countries over time; clinical and laboratory parameters may differentiate between various causes. This study was undertaken to investigate the spectrum of MAS among Indian adults and to find out the features that may help to differentiate between TM and celiac disease.
Methods:
Causes of MAS, and factors differentiating tropical malabsorption (TM) from celiac disease (CD) were determined in 275 patients.
Results:
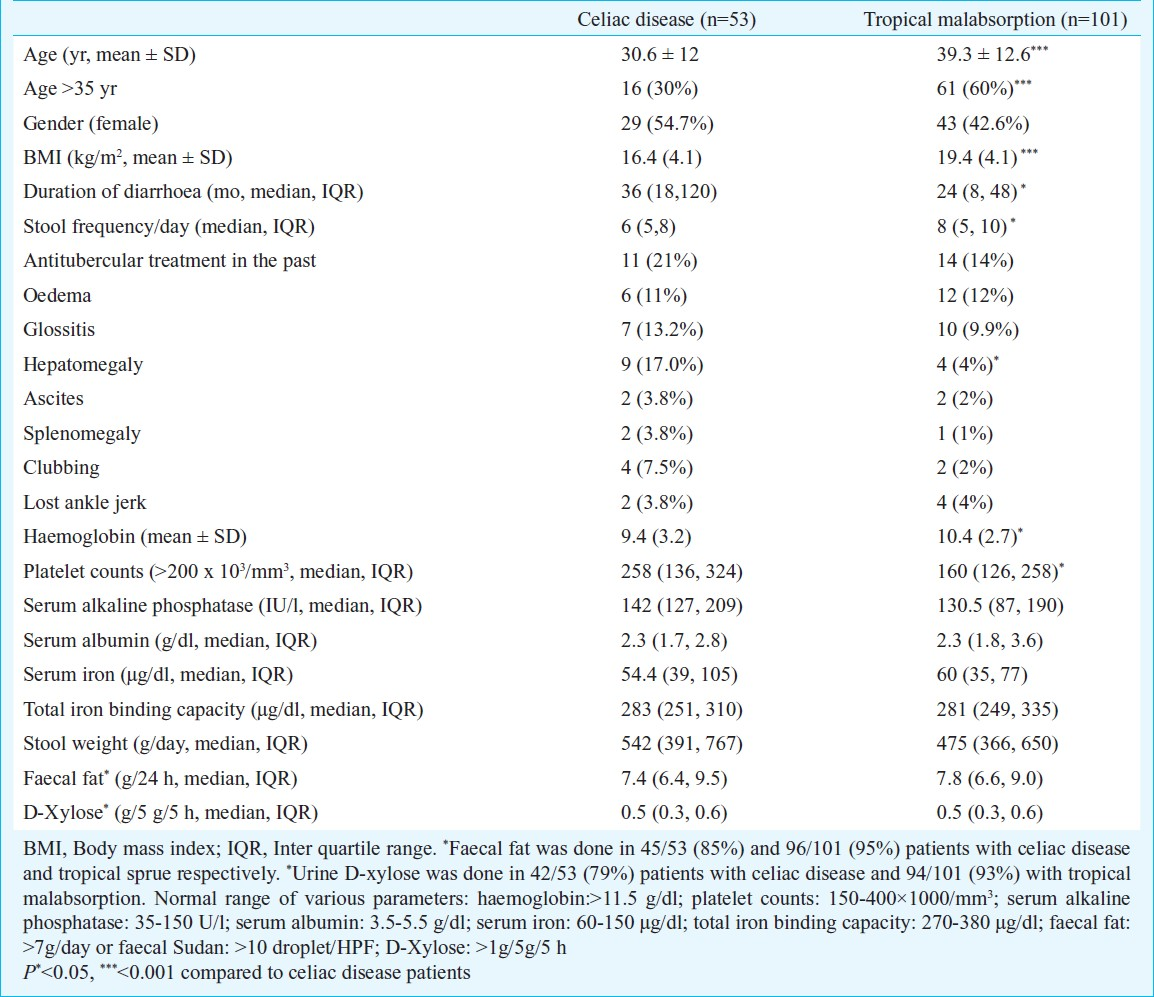
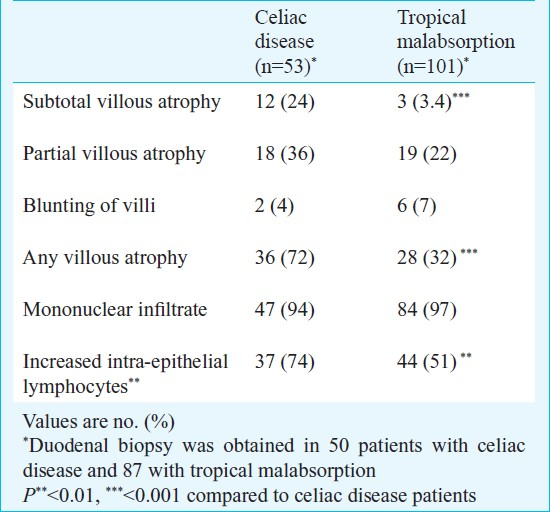
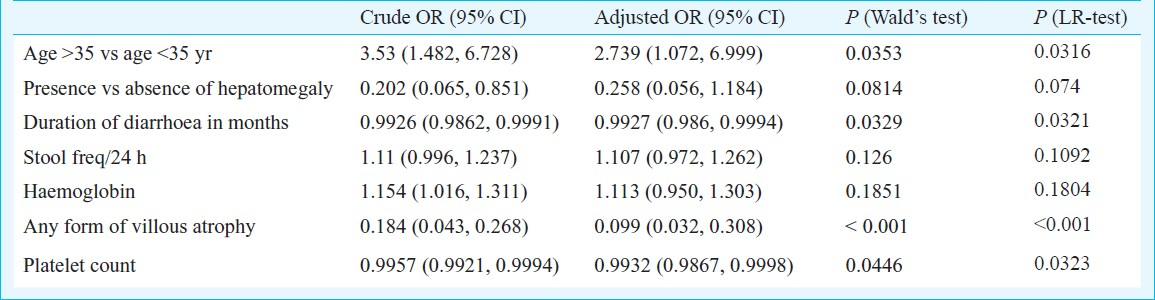
Using standard criteria, causes in 275 patients [age 37.5+13.2 yr, 170, (61.5%) male] were, TM 101 (37%), CD 53 (19%), small intestinal bacterial overgrowth 28 (10%), AIDS 15 (5.4%), giardiasis 13 (5%), hypogammaglobulinemia 12 (4%), intestinal tuberculosis 7 (2.5%), strongyloidiasis 6 (2%), immunoproliferative small intestinal disease 5 (2%), Crohn's disease 6 (2%), amyloidosis 4 (1.5%), intestinal lymphangiectasia 3 (1%) and unknown 22 (8%). On univariate analysis, patients with CD were younger than TM (30.6+12 vs. 39.3+12.6 yr, P<0.001), had lower body weight (41.3+11.8 vs. 49.9+11.2 kg, P<0.001), longer diarrhoea duration (median 36 inter-quartile range 17.8-120 vs. 24-months, 8-48, P<0.01), lower stool frequency (6/day, 5-8 vs. 8, 5-10, P<0.05), lower haemoglobin (9.4+3.2 vs. 10.4+2.7 g/dl, P<0.05), higher platelet count (2,58,000, range 1,35,500-3,23,500 vs. 1,60,000, 1,26,000-2,58,000/mm3, P<0.05), and more often had hepatomegaly (9/53, 17% vs. 4/101, 4%, P<0.01), and subtotal or partial villous atrophy (36/50, 72% vs. 28/87, 32%, P<0.001). Younger age (<35 yr), longer diarrhoea duration, higher platelet count and villous atrophy were significant on multivariate analysis.
Interpretation & conclusions:
TM and CD are common causes of MAS among Indian adults. Younger age (<35 yr), longer diarrhoea duration, higher platelet count and villous atrophy were found to be associated with CD.
Keywords
Chronic diarrhoea
Crohn's disease
small intestinal bacterial overgrowth
small intestinal diseases
tropical enteropathy
tropical sprue
Malabsorption syndrome (MAS) is a common condition in gastroenterology practice in tropics including India1. Aetiology of MAS in tropical areas differs from that in temperate countries and can be expected to vary over time1. In the past, tropical malabsorption (TM), popularly known as tropical sprue, was a common cause of MAS in India. Epidemics of TM have been described in southern Indian villages in the past2. Sporadic cases of TM have been described from other tropical countries such as Pakistan3, Thailand4 and Malaysia5 and even in temperate region such as Puerto Rico6 and Britain7. It is believed that, in recent years, with improvement socio-economic status and sanitary conditions and increasing use of antibiotics, frequency of TM may have declined even in tropical countries in spite of contradictory evidence1. Moreover, there could be considerable overlap between post-infectious MAS, which is a subgroup of TM, and post-infectious irritable bowel syndrome (IBS)8, a common condition in temperate countries9. Celiac disease (CD), once thought to be uncommon in tropical countries including India, is being reported frequently as a cause of MAS among children and adults10. Data on spectrum of MAS in Indian adults are however, scanty and contradictory10–12.
It is difficult to differentiate between celiac disease and TM. Response to antibiotics, a criterion used to diagnose TM, may be misleading as patients with celiac disease may have secondary small intestinal bacterial overgrowth (SIBO) that at least temporarily may respond clinically to treatment with antibiotics1113. Thus, it has been proposed that celiac disease should not only be diagnosed using conventional criteria1314, and a serological test should be performed. Hence, there is a need to determine demographic, clinical and laboratory parameters that may help to differentiate TM from celiac disease in adults with MAS in tropical countries. This may help clinicians to assess the probability of celiac disease in a given patient with serological tests and empirical institution of gluten free diet in patients with high probability of the disease even in tropical countries. This study was thus aimed to assess (i) the spectrum of MAS among Indian adults, and (ii) features that may help to differentiate TM and celiac disease among them.
Material & Methods
Consecutive patients with MAS attending the Luminal Gastroenterology Clinic of the Department of Gastroenterology at Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, a tertiary referral center in north India, during a 10 yr period (from April 2000 to March 2010) were included. Patients were evaluated using a standard protocol, which was approved by the Institutional Ethics Committee.
Protocol for evaluation for MAS: Urine D-xylose, quantitative faecal fat measurement or faecal Sudan stain and duodenal biopsy were done to investigate MAS. Patients with abnormal results in at least two of three tests [urine D-xylose <1.0g/5g/5h, (faecal fat >7g/day or faecal Sudan stain >10 droplet/high power field) and any degree of villous atrophy on duodenal histology] were included in the study. Patients with abnormal results on one of the three tests and evidence supporting a specific cause of MAS were also included. Investigations for aetiology and complications of MAS followed a standard protocol. These included: (i) stool microscopy with various staining methods, (ii) haemogram, (iii) blood biochemistry, (iv) serological tests [human immunodeficiency virus (Enzyme-immunoassay, XIV chex, Qualigenes Diagnostics, Bangalore and Comb AIDS, Span Diagnostics, Surat, India)], (v) anti-endomysial antibody test (indirect immunofluorescence assay, Binding Site, UK), (vi) quantitative estimation of immunoglobulins (IgA, IgG and IgM) levels in serum, (vii) small bowel barium series, (viii) endoscopic duodenal or jejunal biopsies, which was interpreted by an experienced pathologist using a standard grading system15, (ix) glucose hydrogen breath test (using 100 g glucose and a technique that has been described previously to diagnose SIBO)13. Abdominal ultrasonography, bone marrow biopsy, and colonoscopy were done when deemed necessary on clinical grounds.
Tests for absorption:
D-xylose test - Amount of D-xylose excreted in urine during a 5 h period following ingestion of 5 g of D-xylose was estimated using a colorimetric method. Excretion of < 1.0 g D-xylose was considered abnormal16.
Estimation of faecal fat - Faecal fat was estimated by Van de Kamer's technique after a three day fat load (75 g/day). Daily stool collection was done during the next three days, during which fat loading was continued. Mean daily stool weight and mean daily fat excretion was calculated. Faecal fat excretion >7 g/day was considered abnormal. Faecal fat was also tested by microscopic examination of the spot stool specimen stained with Sudan III stain. Faecal Sudan >10 droplets per high power field was considered as abnormal.
Criteria for diagnosis: Celiac disease: European Society of Pediatric Gastroenterology and Nutrition criteria14, giardiasis and strongyloidiasis: demonstration on stool microscopy and/or duodenal biopsy; Crohn's disease and intestinal tuberculosis: standard criteria described previously17; SIBO: positive glucose hydrogen breath test (GHBT); Immunoproliferative small intestinal disease (IPSID), lymphangiectasia and amyloidosis: classical histological features; hypogammaglobulinemia: low level of one or more immunoglobulins (IgG, IgM or IgA) in serum; acquired immunodeficiency syndrome (AIDS): anti-HIV antibodies by two enzyme immunoassays and CD4+ T cell count <200/ml; TM: absence of any specific cause for MAS using various tests listed above, and persistent response to treatment with antibiotics and folic acid. Patients in whom diagnosis could not be made despite complete work-up and inadequate response to treatment for TM and/or inadequate follow up were classified in idiopathic group.
Treatment and follow up: In addition to nutritional and supportive measures, specific treatment included gluten-free diet, antibiotics, nitroimidazole, azathioprine and/or corticosteroids, ATT, medium chain triglycerides, highly active anti-retroviral therapy, albendazole, tetracycline and anti-malignant chemotherapy as indicated for CD, SIBO, giardiasis, Crohn's disease, tuberculosis, lymphangiectasia, AIDS, strongyloidiasis and IPSID, respectively. Patients with TM were treated with tetracycline (500 mg thrice daily for one month and 500 mg twice daily for another one month) and folic acid (10 mg daily for at least 6 month). Non-responsive patients with TM and SIBO, were treated with ciprofloxacin or norfloxacin or rifaximin. The parameters evaluated for response during follow up visits were reduction in stool frequency, increase in body weight, improvement in haemoglobin and serum albumin, normalization of urinary excretion of D-xylose and duodenal histology.
Statistical analysis: Data were checked for normal distribution using Shapiro-Wilk test. Differences between non-parametric unpaired continuous and categorical variables were analyzed using Wilcoxon rank sum test and Chi-square test with Yates’ correction as applicable, respectively. Parametric continuous data were analyzed using unpaired t test. Receiver-operating characteristic (ROC) curves were generated to determine the best cut-off values of parameters that best differentiated celiac disease from TM. Parameters found significant by univariate analysis were analyzed using a step-wise logistic regression method. Statistical analysis was done using R and Epicalc software version R2.9.0 (R development core team, Vienna, Austria).
Results
Patients: Of the 296 patients screened, 275 [age 37.5 ± 13.2 yr, male 167 (61%)] were included in the study; the other 21 were excluded as they did not fulfill the inclusion criteria for MAS. Of these 275, 19 (7%) patients were in the age group between 12-18 yr.
Results of investigations for mucosal malabsorption: Urine D-xylose: Urinary excretion of D-xylose, performed in 233/275 (85%) patients, was 0.53 + 0.30 g/5 g/5 h. It was abnormal in 212 of 233 (91%) patients with MAS.
Faecal fat and faecal Sudan: The mean faecal fat excretion, estimated in 167 of 275 (61%) patients, was 8.4 ± 3.4 g/day. It was abnormal in 120 of 167 (72%) patients. The median faecal fat excretion by Sudan stain, evaluated in 209 of 275 (76%) patients, was 17 (range 3 - 50) droplets/HPF. It was abnormal in 168 of 209 (80.4%) patients.
Results of histopathological examination of duodenal biopsy: Duodenal biopsy was obtained in 226 (82%) patients with MAS; 17 (7.5%) had subtotal villous atrophy, 58 (25.7%) had partial villous atrophy, 45 (20%) had blunting of villi and one patient had normal villi; 217 (96%) had increased mononuclear infiltrate and 126 (55.8%) had increased intraepithelial lymphocytes (Fig. A–D).
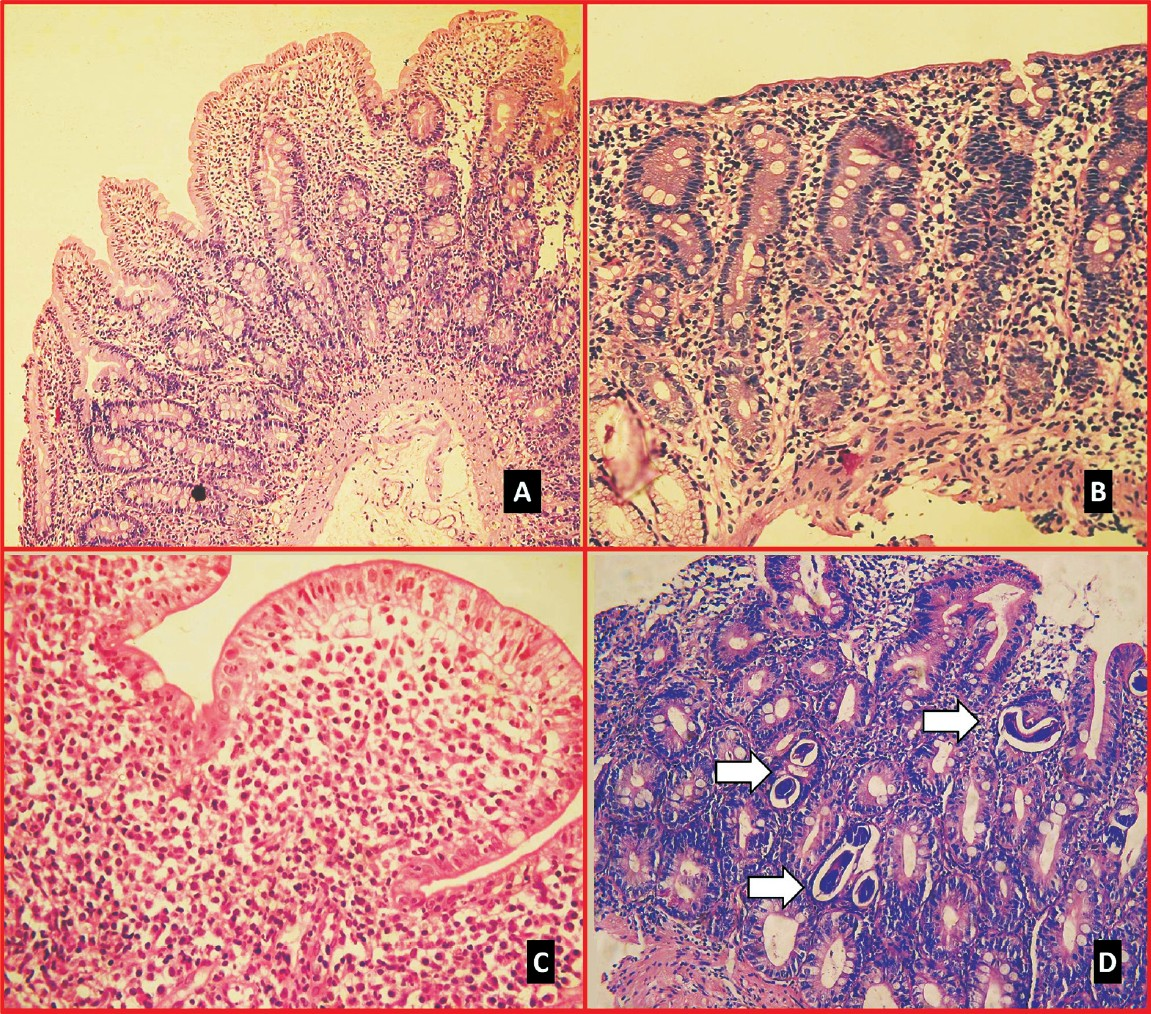
- Histological examination of duodenal biopsies in patients with malabsorption syndrome. (A) Patient with tropical malabsorption showing blunting of villi with increased mononuclear infiltrate in lamina propria, (B) subtotal villous atrophy with crypt hyperplasia in a patient with celiac disease, (C) dense dysplastic lymphomononucler infiltrate with blunting of villi in a patient with immunoproliferative small intestinal disease, (D) larvae of Strongyloides embedded in the mucosa (haematoxylin-eosin).
Of the 275 patients, 148 (54%) had abnormal results in all the three tests (urine D-xylose, faecal fat either by Sudan or by Van de Kamer's method and duodenal biopsy) and 94 (34%) had two of these tests abnormal; of them, urine D-xylose and faecal fat were abnormal in 25 (26%), faecal fat and duodenal biopsy were abnormal in 36 (38.2%) and urine D-xylose and duodenal biopsy were abnormal in 33 (35.1%) patients. Of the remaining 33 (12%) patients with only one of these three tests abnormal, included eight patients with SIBO (by GHBT), one with strongyloidiasis on stool microscopy, six with celiac disease with positive result on anti-endomysial antibody and subtotal or partial villous atrophy on duodenal biopsy, six with TM responding to treatment with tetracycline and folate, one intestinal tuberculosis with ileo-colic fistula on small bowel barium series responding to ATT, four with AIDS, two with IPSID on duodenal biopsy, two with histologically confirmed amyloidosis and three with Crohn's disease diagnosed on imaging, endoscopy, histology and treatment response.
Aetiology of MAS
Giardiasis: Of the 13 (5%) patients with giardiasis [median age 42 yr, range 11-53 yr, 10 (77%) male], 4, 7 and 2 were diagnosed using stool microscopy, histopathology and both tests, respectively. One patient had low level of serum IgA. All the patients responded to treatment with a nitroimidazole.
Intestinal tuberculosis: Of the seven (2.5%) patients with intestinal tuberculosis, [median age 39 yr, range 23-67 yr, 5 (71.4%) male], three had acid fast bacilli (AFB) on microscopic examination of smear, one grew AFB on culture and showed its DNA by polymerase chain reaction. Three other patients had features of ileo-cecal tuberculosis on small bowel barium series including ileo-colic fistula in one and jejunal stricture in another, multiple abdominal lymphadenopathy on computerized tomography scan and positive Mantoux test. All the patients responded to ATT.
Strongyloidiasis: Of the six (2%) patients with strongyloidiasis [median age 30 yr, range 18-70 yr, 5 (83%) male], larvae of strongyloides were detected on microscopic examination of stool or histopathological examination of duodenal biopsy in three each (Fig. D). Two of them were receiving corticosteroids and one had hypogammaglobulinemia. Peripheral blood eosinophilia was absent in four patients. Two patients died of septicemia. Two other patients with AIDS also had larvae of strongyloides on stool microscopy.
Acquired immunodeficiency syndrome (AIDS): Fifteen (5.4%) patients (median age 36 yr, range 30-57 yr) had AIDS. Patients with AIDS were more often male than those with MAS due to other causes [13/15 (87%) vs. 154/260 (59%), P<0.03). Patients with AIDS (n=15) and intestinal lymphangiectasia (n=2) had lower absolute lymphocyte count than MAS due to other causes (median 1296/mm3, range 360-2520 vs. 1775/mm3, range 176-6120, P<0.01). Stool microscopy revealed larvae of strongyloides in two, Isospora belli cyst in one, eggs of ascaris in one, both Hymenolepis nana and Cryptosporidium in one. Four patients had history of sexual promiscuity, four had undergone prior surgery and three had history of blood transfusion.
Intestinal lymphangiectasia: Three patients with intestinal lymphangiectasia were diagnosed on duodenal biopsy and responded to treatment with median chain triglycerides.
IPSID and hypogammaglobulinemia: Five (2%) patients (age 33 yr, range 27-38 yr, all male) were diagnosed IPSID on duodenal biopsy (Fig. C). All presented with chronic small bowel diarrhoea and weight loss. Three patients had been treated with ATT in the past by community physician. One patient had a mass in the right iliac fossa and two had digital clubbing. Three (60%) patients had SIBO on glucose hydrogen breath test and one had Giardia on stool microscopy. Three patients had increased level of serum alkaline phosphatase [median 130 (range 63 to 420 U/l)]. Three patients were successfully treated with tetracycline alone for early disease. Of the other two with advanced disease, one died of explosive diarrhoea and shock while receiving anti-cancer chemotherapy and the other declined further treatment.
Amyloidosis: Of the 275 patients with MAS, four (1.5%) (median age 47 yr, range 23 to 61 yr, three male) had presence of amyloid on rectal biopsy (n=2), duodenal biopsy (n=1) or abdominal fat pad aspirate (n=1) using Congo red staining.
Crohn's disease: Of the 275 patients with MAS, six (2%) [median age 36 yr (range 22 to 53 yr), 5 male] had Crohn's disease. Two of them had ileo-colic fistula. Two patients had been treated with ATT in the past. Two patients had SIBO on GHBT. Five patients responded to treatment and one died of sepsis.
Tropical malabsorption and celiac disease: Tropical malabsorption (n=101) was the commonest cause of MAS followed by celiac disease (n=53). Forty of 49 patients (82%) with celiac disease, who underwent test for anti-endomysial antibody, had positive result. Of the remaining nine patients, three had low level of serum IgA, one had anti-tTG antibody and other had anti-gliadin antibody in serum. The clinical and demographic details of TM and celiac disease patients are shown in Table I. On univariate analysis, patients with celiac disease were younger than TM, had lower body weight (41.3+11.8 vs. 48.9+11.2 kg, P<0.001) though height was comparable (156.9 ± 11.9 vs. 158.5 ± 9.6 cm), longer diarrhoea duration, lower stool frequency, lower haemoglobin levels, higher platelet count, hepatomegaly, subtotal or partial villous atrophy or blunted villi (Tables I and II). The best cut-off value of age that differentiated TM from celiac disease was 35 yr (area under curve 0.68, sensitivity 70%, specificity 61%). The best cut-off value of haemoglobin that differentiated TM from celiac disease was 10 g/dl (area under curve 0.62, sensitivity 63%, specificity 56%) and that of platelet count was 200 × 103/mm3 (area under curve 0.62, sensitivity 62%, specificity 77%). Patients with celiac disease more often had haemoglobin value less than 10 g/dl than those with TM [30 (57%) vs. 37 (37%), P=0.017] and had platelet count more than 200 × 103/mm3 [28 (53%) vs. 29 (29%), P=0.003]. However, only one patient with celiac disease had thrombocytosis (platelet count 600 × 103/mm3). Younger age (<35 yr), longer diarrhoea duration, higher platelet count and villous atrophy were significant on multivariate analysis (Table III). GHBT, performed in 52 (51.5%) of 101 patients with TM, revealed SIBO in 12 (23%) patients.
Two patients with strongyloidosis and one with IPSID died. Of the remaining patients, nine with idiopathic MAS did not respond to treatment. Frequency of recurrence after successful treatment was comparable among patients with celiac disease and TM (two patients each) during a follow up period of 12.5 ± 15.3 and 10.8 ± 14 months, respectively.
Discussion
The present study showed that TM and celiac disease are common causes of MAS among Indian adults. Other causes included SIBO, AIDS, giardiasis, hypogammaglobulinemia, intestinal tuberculosis, strongyloidiasis, IPSID, Crohn's disease, amyloidosis and intestinal lymphangiectasia. In 8 per cent patients, the cause for MAS remained unknown.
Aetiological spectrum of MAS is expected to change in developing countries with time. Infective diseases and TM were believed to be common causes in the past, with non-infective causes such as celiac disease being rare in several tropical countries1. Epidemics of TM were reported from southern India2 and tropical countries including South East Asia18, Caribbean19, the Mexico20, the Middle East21, parts of Africa22, Hong Kong23 and Malawi24. The current data show that TM continues to be a major cause of sporadic MAS in Indian adults. This is in accordance with another study from southern India25. A study from north India has shown celiac disease to be a common cause of MAS in Indian adults and children26. In a recent study from Delhi10, though tropical sprue was one of the major causes of malabsorption, celiac disease was commoner. However, the difference in spectrum of MAS from the current study might be explained by age group of patients included and inclusion criteria in addition to geographical factors. The study from Delhi15 and the present study showed that celiac disease was more common among patients with malabsorption at younger age than those at older age. Hence, inclusion of a large proportion of young patients might explain high frequency of celiac disease in that study. In the present study, only 7 per cent patients were in the age group 12-18 yr, a proportion much lower than the Delhi study (30%)10. It is noteworthy that all these studies, including the present one are hospital-based study and, therefore, the findings cannot be generalized to the community.
There is a need to study the clinical and basic laboratory parameters to differentiate between celiac disease and TM as the two conditions clinically mimic closely. Celiac disease usually manifests at a younger age, and may present without diarrhoea but with atypical symptoms. Due to a lack of awareness among physicians about celiac disease in tropical countries, it may remain undiagnosed for a long period. On the other hand, TM is a disease among adults, may start acutely after an episode of gastrointestinal infection and may be partly treated with antibiotics before reaching a tertiary healthcare centre. Hence, patients with celiac disease are expected to have long-lasting clinical or subclinical MAS before being finally diagnosed as compared to patients with TM. Hence, our findings of younger age, lower body mass index, longer duration of diarrhoea, lower haemoglobin and more marked villous atrophy are quite expected.
The current study showed that platelet count was higher among patients with celiac disease than those with TM. Thrombocytosis, defined as a platelet count >600 × 103/μl, is common in patients with celiac disease and may result from inflammatory mediators or from reversible hyposplenism27. As high as 60 per cent patients with untreated celiac disease are reported to have thrombocytosis28. However, only one patient with celiac disease in the current series had platelet count 600×103/μl. This might be related to the fact that platelet count may be lower in Indian population29. Also, associated deficiency of folate and vitamin B12 due to malabsorption might have resulted in a lower platelet count30. Folate and vitamin B12 deficiency and megaloblastic anaemia are expected to be more common in patients with TM31 with consequent lower platelet count. By ROC curve, a cut-off value of platelet count more than 200×103/μl differentiated celiac disease and TM with 62 per cent sensitivity and 77 per cent specificity. The finding of this study suggests that there was an observed difference between celiac disease and TM during initial assessment.
Some causes of MAS detected in the present study are unusual in occurrence. Of the 13 patients with giardiasis, 12 were immunocompetent. Intestinal tuberculosis, though often associated with biochemical malabsorption, clinical malabsorption is uncommon32. Malabsorption in intestinal tuberculosis might result from associated SIBO, secondary amyloidosis, lymphatic blockage and diffuse mucosal disease33. Interestingly, half of the patients had MAS due to strongyloidiasis in absence of immunodeficiency and two-thirds did not have eosinophilia, a parameter by which clinicians suspect strongyloidiasis34. Absence of eosinophilia in hyperinfection with strongyloides has been reported35. Five patients had IPSID as a cause for MAS. This is in accordance with an earlier study from southern India in which 1.5 per cent patients with chronic diarrhoea and MAS had IPSID36. Hypogammaglobulinemic sprue was another cause of MAS that has been uncommonly reported from India37. Many of these unusual causes of MAS may not be suspected even in the tropics resulting in fatal outcome and inappropriate treatment with anti-tuberculosis treatment. Hence, awareness about these diseases is required before clinicians can suspect and diagnose these conditions.
The present study provides important data that may have implications on two conditions, namely TM and post-infectious irritable bowel syndrome (IBS). TM may provide useful models to study post-infectious IBS38. SIBO has been proposed as a condition overlapping both post-infectious IBS and TM38. Thus, our findings may serve as a useful reference point for future research in this area.
In conclusion, the present study show that TM and celiac disease are common causes of MAS among Indian adults. There were several other unusual causes, awareness about which is required before the clinicians can suspect and diagnose. On univariate analysis, patients with celiac disease were younger than TM, had lower body weight, longer diarrhoea duration, less frequent stool, lower haemoglobin, higher platelet count, frequent hepatomegaly and villous atrophy. Younger age (<35 yr), longer diarrhoea duration, higher platelet count and villous atrophy were associated with celiac disease on multivariate analysis.
References
- Etiological spectrum of sporadic malabsorption syndrome in northern Indian adults at a tertiary hospital. Indian J Gastroenterol. 2004;23:94-8.
- [Google Scholar]
- Epidemic tropical sprue and other epidemics of diarrhea in South Indian villages. Am J Clin Nutr. 1968;21:1077-87.
- [Google Scholar]
- Tropical sprue as the cause of chronic diarrhea after travel to Southeast Asia. Z Gastroenterol. 1998;36:897-900.
- [Google Scholar]
- Post-infective malabsorption in the temperate zone. Trans R Soc Trop Med Hyg. 1985;79:322-7.
- [Google Scholar]
- Bugs and irritable bowel syndrome: The good, the bad and the ugly. J Gastroenterol Hepatol. 2010;25:244-51.
- [Google Scholar]
- Current spectrum of malabsorption syndrome in adults in India. Indian J Gastroenterol. 2011;30:22-8.
- [Google Scholar]
- Spectrum and antibiotic sensitivity of bacteria contaminating the upper gut in patients with malabsorption syndrome from the tropics. BMC Gastroenterol. 2003;3:9.
- [Google Scholar]
- Spectrum of atypical celiac disease in North Indian children. Indian Pediatr. 2004;41:822-7.
- [Google Scholar]
- Partially responsive celiac disease resulting from small intestinal bacterial overgrowth and lactose intolerance. BMC Gastroenterol. 2004;4:10.
- [Google Scholar]
- No authors listed. Revised criteria for diagnosis of celiac disease. Report of working group of European Society of Pediatric Gastroenterology and Nutrition. Arch Dis Child. 1990;65:909-11.
- [Google Scholar]
- 1H NMR spectroscopic method for diagnosis of malabsorption syndrome: a pilot study. NMR Biomed. 2004;17:69-75.
- [Google Scholar]
- Crohn's disease in India: a multicenter study from a country where tuberculosis is endemic. Dig Dis Sci. 2009;54:1099-107.
- [Google Scholar]
- A randomized, double-blind, placebo-controlled trial of rifaximin, a nonabsorbable antibiotic, in the treatment of tropical enteropathy. Am J Gastroenterol. 2009;104:2326-33.
- [Google Scholar]
- Spectrum of malabsorption syndrome in India: Tropical sprue is still the leader. J Assoc Physicians India. 2011;59:420-2.
- [Google Scholar]
- Hyposplenism in celiac disease.Role of a gluten-free diet. Acta Gastroenterol Latinoam. 1991;21:17-21.
- [Google Scholar]
- Severe thrombocytopenia probably due to acute folic acid deficiency. Crit Care Med. 1979;7:297-300.
- [Google Scholar]
- A study of malabsorption in intestinal tuberculosis: stagnant loop syndrome. Am J Clin Nutr. 1980;33:244-50.
- [Google Scholar]
- Utility of hydrogen breath tests in diagnosis of small intestinal bacterial overgrowth in malabsorption syndrome and its relationship with oro-cecal transit time. Indian J Gastroenterol. 2006;25:6-10.
- [Google Scholar]
- Disseminated strongyloidiasis in immunocompromised patients - report of three cases. Int J Dermatol. 2009;48:975-8.
- [Google Scholar]
- Intestinal strongyloidiasis: a diagnosis frequently missed in the tropics. Trans R Soc Trop Med Hyg. 2009;103:242-6.
- [Google Scholar]
- Immunoproliferative small intestinal disease in South India: a clinical and immunomorphological study. J Gastroenterol Hepatol. 1998;13:1207-11.
- [Google Scholar]
- Hypogammaglobulinaemic sprue in tropics: Report of an Indian patient. J Trop Med Hyg. 1978;81:131-3.
- [Google Scholar]
- Post-infectious irritable bowel syndrome: the past, the present and the future. J Gastroenterol Hepatol. 2011;26(Suppl 3):94-101.
- [Google Scholar]






