Translate this page into:
Beneficial effect of Lisosan G on cultured human microvascular endothelial cells exposed to oxidised low density lipoprotein
Reprint requests: Dr Vincenzo Longo, Institute of Agricultural Biology & Biotechnology, CNR, Pisa, Via Moruzzi 1 56100 Pisa, Italy e-mail: v.longo@ibba.cnr.it
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Nutritional compounds which display anti-inflammatory and antioxidant effects have specific applications in preventing oxidative stress and endothelial dysfunction. In this study we evaluated the effect of Lisosan G (powder of Triticum sativum grains) on human microvascular endothelial cells (HMEC-1) exposed to oxidized low density lipoprotein (ox-LDL).
Methods:
The protective effects of Lisosan G were evaluated on human microvascular endothelial cells exposed to ox-LDL. Intercellular adhesion molecular-1 (ICAM-1), endothelin-1 (ET-1), and interleukin-6 (IL-6) concentrations and the expression of the respective genes were evaluated in response to incubation with ox-LDL, after co-incubation with ox-LDL and Lisosan G or exposed to Lisosan G alone. The analysis of LOX-1 gene was performed with RT-PCR semi quantitative method. The degree of oxidation induced in relation to control, was established by measurement of malondialdehyde (MDA) production.
Results:
The incubation with ox-LDL induced a significant increase in ICAM-1, IL-6 and ET-1 levels compared to the basal condition (P<0.01, P<0.05, and P<0.01, respectively), while in presence of Lisosan G, ICAM-1 levels showed a significant reduction both compared to the cultures treated with ox-LDL and control (P<0.01). IL-6 levels did not show any difference; ET-1 levels showed a partial reduction after co-treatment with Lisosan G, and also with Lisosan G alone, reduced the concentration below control (P<0.01). The modulation of these markers was confirmed by RT-PCR analysis. An association between MDA formation and the three markers production was observed. Semi-quantitative analysis of LOX-1 gene expression showed a significant up-regulation only after ox-LDL exposure.
Interpretation & conclusions:
The results demonstrate that Lisosan G may have an important role in the prevention of microcirculatory dysfunction.
Keywords
Adhesion molecules
endothelins
endothelium
inflammation
lipoproteins
oxidative stress
Oxidant by-products of normal metabolism cause extensive damage to DNA, protein, and lipid. Many clinical and experimental studies support a direct role of microcirculatory dysfunction in the genesis of target organ damage during oxidative stress and hypercholesterolaemia1. Due to a chronically enhanced oxidative stress, in diabetes and hypertension oxidised low density lipoprotein (ox-LDL) is formed in large quantity, and is also characterized by abnormalities in microcirculatory function2.
The influence of both native and oxidized LDL on the release of potent vasoactive substances - such as nitric oxide (NO) and endothelin-1 (ET-1) by the endothelium is potentially relevant both in initiating and maintaining abnormal tissue perfusion3. OxLDL can induce NO synthesis also by acting as an inflammatory stimulus4, that is, by triggering interleukin-6 (IL-6)-mediated inducible nitric oxide synthase (iNOS) synthesis and activation4. Intracellularly generated oxygen-derived free radicals5 such as superoxide anions (O2-), hydroxyl radicals (OH·) and hydrogen peroxide (H2O2) are shown to play a role in endothelial dysfunction in hypertension and atherosclerosis promoting intercellular adhesion molecule-1 (ICAM-1) expression in endothelial cells and ICAM-1 dependent adhesion of monocytes6. Modulation of the expression of these adhesion molecules by free radicals may, therefore, be an important mechanism in initiating atherosclerosis7.
ET-1 is a potent vasoconstrictor peptide synthesized by endothelial cells which plays a significant role in the regulation of vascular function and structure because it is a strong regulator of mitogenesis and able to stimulate the macrophages to synthesize monocytes chemoattractant protein8. Information on the mechanisms through which native and Ox-LDL interact with the endothelium is limited to large vessels; in these cells, the acute effect of Ox-LDL appears to be largely, though not entirely, determined by the interaction with the lectin-like Ox-LDL receptor (LOX1-R)9. However, other mechanisms could be involved, since both modified apolipoprotein B and lipid moieties such as isoprostanes present in oxidized LDL can interact with other receptors present in endothelial cells, such as the scavenger receptor or the thromboxane A2 receptor10 whose role in modulating the synthesis of vasoactive products is unknown.
Nutritional compounds which display anti-inflammatory and antioxidant effects have specific applications in preventing oxidative stress induced injury which characterizes their pathogenesis11. Polyphenolic constituents of red wine known for its anti-atherogenic properties, are thought to be beneficial in reducing the incidence of cardiovascular diseases (CVD) for example, resveratrol appears to be a natural antioxidant that enhances cholesterol efflux. These properties make it a potential natural antioxidant that could be used to prevent and treat cardiovascular disease12. Resveratrol restored endothelial function in type 2 diabetes by inhibiting TNFα-induced activation of NAD(P)H oxidase and preserving eNOS phosphorylation, suggesting the potential for new treatment approaches to promote vascular health in metabolic diseases13. Antioxidant defenses against this damage include ascorbate, tocopherol, and carotenoids.
In our laboratory, it has been shown that the powder of grain of Triticum sativum (Lisosan G), used as nutritional supplement, did not interfere with the phase 1 and 2 drug metabolizing enzymes and had hepatoprotective effects in rats intoxicated by carbon-tetrachloride14. In addition, it has shown a radical scavenger activity may be due to the presence of antioxidant molecules in this compound. Lisosan G is a good source of vitamins, oligoelements, polyunsaturated fatty acids. On the basis of these results, it was suggested that Lisosan G might be co-administrated during drug therapy14. Recently we have shown a protective effect of Lisosan G against the cisplatin induced toxicity. It has been suggested that the protective effect of Lisosan G could be associated mainly with the attenuation of the oxidative stress and the preservation in antioxidant enzymes15.
The present study was undertaken to evaluate the protective effects of Lisosan G on human microvascular endothelial cells (HMEC-1) exposed to ox-LDL. We also compared the protective mechanism of Lisosan G in copper-dependent LDL oxidation.
Material & Methods
The study was performed in the laboratories of the Institute of Agricultural Biology and Biotechnology, CNR, Pisa, Italy.
Cell cultures: HMEC-1 was kindly provided by Prof. E W Ades (Center for Disease Control, Atlanta, USA). Primary cells were immortalized by transfection with PBR-322-based plasmid containing the coding region for the simian virus 40 large T16. Cells were cultured in M-199 medium (Sigma Life Sciences, USA) supplemented with 10 per cent (v/v) foetal bovine serum, 1 per cent glutamine, 1 per cent antibiotics, 1 per cent endothelial growth factor (EGF; Sigma Chemical Co., USA) and 0.5 per cent hydrocortisone, in a 95 per cent O2, 5 per cent CO2 atmosphere and maintained at a density of 6×105 cells/ml by sub-culturing, every 4-5 days, a 1:2-1:3 dilution of cell suspension in fresh medium (cell viability was >95% as determined by trypan blue exclusion).
For all experiments, cells (at the 7th-8th passage) were plated in 60 × 15 mm dishes and allowed to reach 70 per cent confluency. In order to minimize interferences with the assays, 48 h before any treatment cells were incubated with M 199 medium without phenol red and supplemented with antibiotics only.
To evaluate the effect of Lisosan G was a gift by Agrisan Company, Pistoia, Italy on cells viability, HMEC-1 were incubated for 24 h at different doses (0, 0.07, 0.7, 1.4 mg/ml) of Lisosan G. The highest dose showing no effect on cell viability was used in the experiments (cell viability was >95% as determined by trypan blue exclusion). The powder of Lisosan G was sonicated in water and after centrifugation the supernatant was added to the medium 1 h before the treatment with ox-LDL.
ICAM-1, ET-1, and IL-6 concentration in the medium and the expression of the respective genes of HMEC-1 were measured in response to incubation with 200 μg/ml of ox-LDL or with co-incubation of Lisosan G, or with Lisosan G alone.
LDL isolation and oxidized LDL preparation: To isolate LDL, blood (40 ml) was collected in tubes containing EDTA (1 mg/ml) from 10 healthy volunteers recruited from laboratory staff of our institute and immediately centrifuged at 1207 g at 4°C. All the aliquots were pooled and LDL (d=1.019-1.063) was isolated by ultracentrifugation at 158000 g, at 4°C (OPTIMA L-90 K, Beckman, CA, USA) in NaBr solutions with EDTA to avoid oxidation during isolation. All solutions were degassed, and samples were kept at 4°C in a dark environment. To remove EDTA, the LDL fraction was gel-filtered on a Sephadex column (Econo-Pac 10 DG columns; Bio-Rad, CA, USA) and eluted in 1 M PBS buffer (pH 7.4).
The oxidation of LDL solution (200 μg/ml) was performed after incubation with 10 μM CuSO4 in M-199 medium at 37°C 24 h. After the challenge, CuSO4 was removed by double filtration (Centricon Plus-20; Millipore Corp, Bradford, MA, USA). Immediately Ox-LDL solution was used for 24-h incubation of 70 per cent confluent monolayers of HMEC-1 placed in 6-well dishes containing 3 ml of medium and approximately 105 cell each.
The extent of oxidation was estimated by measuring the concentration of malondialdehyde (MDA) (as thiobarbituric acid-reactive substances, expressed as nmole MDA per mg LDL protein)17. Medium concentrations of ET-1 and interleukin-6 (IL-6) were evaluated by two different kit of ELISA technique employing a solid-phase sandwich, enzyme-linked immuno-sorbent assay (Cayman, Ann Arbor MI, USA; Biosource International, Inc. Camarillo, California, USA). Medium concentration of ICAM-1 was evaluated with ELISA method (Bender MedSystem Vienna, Austria, Europe).
All analysis was done in duplicate, and concentrations were normalized to 105 cells by counting.
Reverse transcription polymerase chain reaction (RT-PCR) for LOX-1 gene: RNA extraction was performed with Micro-to-Midi Total RNA Purification System (Invitrogen Life technologies, USA). After removing medium, an RNA lysis solution was added to dishes, and distributed to the entire surface. Cell lysates were then transferred to tubes, and passed through a 21-gauge needle attached to a 1 ml syringe, 3-4 times. After adding 70 per cent ethanol, samples were applied to an RNA Spin Cartridge, and centrifuged at 12,000 g for 15 sec at 25°C. After washing with buffers, RNase-free water was added to the columns to collect RNA. In a 0.5-ml tube, 1 μl random primer (50 ng/μl) (Random primers are oligodeoxyribonucleotides, mostly hexamers, suitable for DNA synthesis), 1 μl RNA (10 pg/μl), and 2 μl of 10 mM dNTP Mix (Invitrogen Life technology, USA) was adjusted to 12 μl with diethylpyrocarbonate (DEPC) water. RNA was denaturated by incubating the solution at 65°C for 5 min and then placed on ice. The 5X cDNA synthesis Mix was prepared on ice: 4 μl of buffer, 1 μl of 0.1 M DTT, 1 μl water, 1 μl Ribonuclease (RNase) inhibitor (RNaseOUT) (40 U/μl) and 1 μl ThermoScript RT (15 U/μl) (Invitrogen Life Tecnology, USA). RT-PCR condition and primers utilized in our study are previously reported18–20.
Determination of peroxidation products - LDL solutions: LDL aliquots (50 μg protein/ml) were incubated with Cu2+ at 37 °C using a Perkin Elmer spectrophotometer (PE-Lambda Bio2, England) equipped with a Peltier-thermostatted 8-position cuvette holder. Cu++-mediated LDL oxidation was monitored at 234 nm every 1.5 min for 2 h at 37 °C by the kinetic profiles of conjugated dienes (CD). It was characterized in terms of lag time (t lag), which reflects the protective effect of endogenous antioxidants and formation and breakdown of reactive intermediates of hydroperoxide1819. For three experiment conducted, t lag was calculated graphically from the intercept of lines drawn through the linear portions of the lag phase and the propagation phase. Cu2+-mediated LDL oxidation was initiated in a buffer solution PH = 7.4, with 0.2 mM CuSO4. The kinetic profiles of conjugated dienes were characterized by the respective tlag. Lisosan-G concentrations analyzed were: 20, 40, 60, 80 μg/ml. These concentrations were compared with a solution of vitamin C 0.2 μg/ml.
Statistical analysis: One-way ANOVA with Dunnet's post hoc test was used to evaluate the modulation of endothelial vasoactive products in HMEC-1 cells treated with ox-LDL or ox-LDL plus Lisosan G or only Lisosan-G. The same analysis was performed to establish difference among Cu++ -mediated LDL oxidation and with or without Lisosan G concentrations or in presence of vitamin C. Linear regression analysis was conducted to establish the association between each markers and MDA production.
Results
In a preliminary study, HMEC-1 were treated with different doses of Lisosan G (0, 0.07, 0.7, and 1.4 mg/ml) to find the optimal experimental dose to avoid cytotoxicity (data not shown). There was no difference among the doses, except a slight reduction of cells viability at the higher dose, consequently 0.7 mg/ml of Lisosan G was used in further experiments.
The induced oxidative stress by ox-LDL (200 μg/ml) in HMEC-1 cells, was quantified by MDA formation (1.05 nmole MDA/mg protein). The MDA production was significantly higher than control (P<0.001) in the cell treated with ox-LDL (Fig. 1).
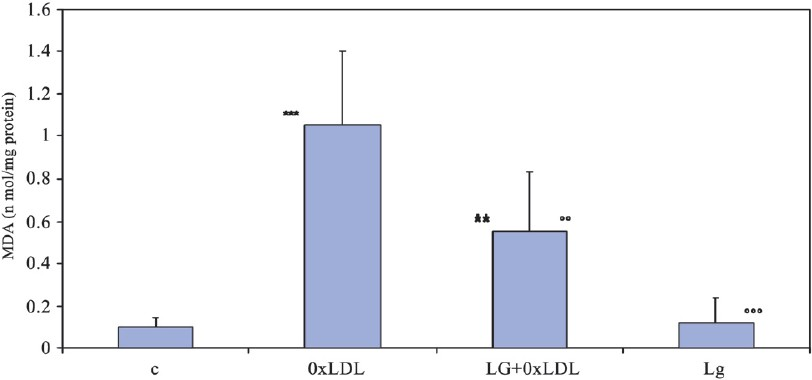
- MDA production in presence or absence of ox-LDL and Lisosan G. **P<0.01; ***P<0.001 compared to control; °°P<0.01, °°°P<0.01 compared to ox-LDL.
The incubation with ox-LDL induced an increment of ICAM-1 medium concentration compared to the basal condition (P<0.01), while in presence of Lisosan G a significant reduction was observed compared to cultures treated with ox-LDL and control (P<0.01) (Fig. 2).
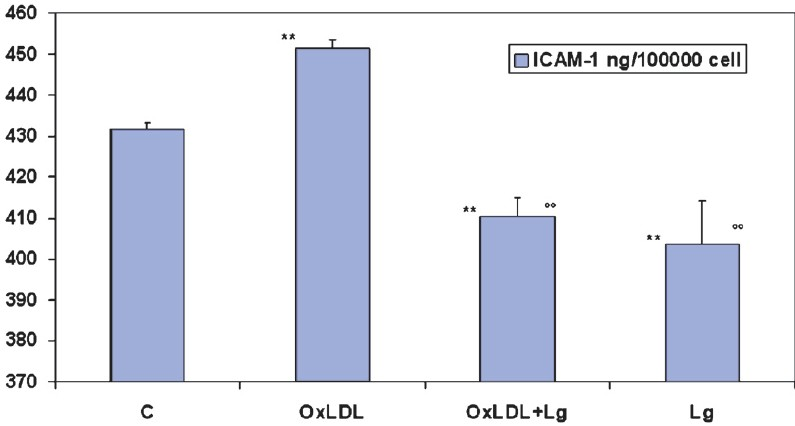
- Effect of oxLDL on endothelial ICAM-1 production. Lisosan G shows a significant reduction of ICAM-1 medium concentration (ELISA method). **P<0.01 compared to control; °°P<0.01 compared to ox-LDL incubation.
IL-6 medium concentration increased after treatment with ox-LDL compared to basal condition (P<0.05), while the treatment with Lisosan G incubated with ox-LDL or alone did not show any difference suggesting a protective effect (Fig. 3). The analysis of ET-1 medium concentration showed a significant increase after ox-LDL treatment compared to control (P<0.01), but reduced after co-treatment with Lisosan-G (Fig. 3). The treatment with Lisosan G alone reduced the concentration below the basal condition (Fig. 3).
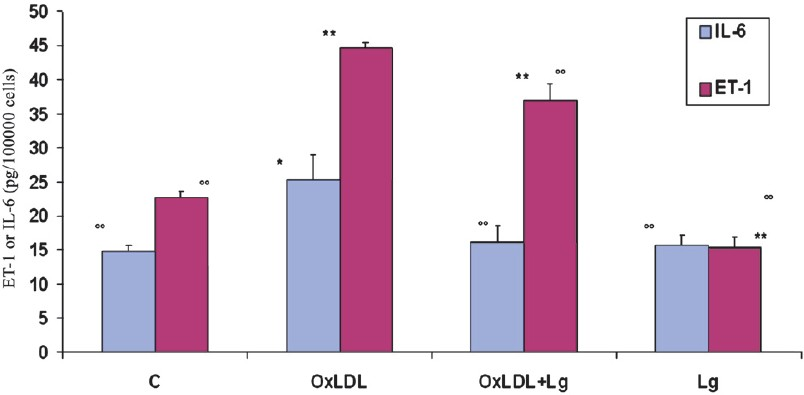
- Effect of ox-LDL on endothelial IL-6 and ET-1 production. These markers were significantly reduced after the incubation with Lisosan G. *P<0.05, **P<0.01 compared to control; °°P<0.01 compared to ox-LDL incubation.
Semi-quantitative analysis of LOX-1 gene expression showed a significant upregulation only after ox-LDL exposure (Fig. 4). Linear regression analysis conducted between MDA concentration and production of ICAM-1, IL-6 and ET-1 in the group of cells exposed to ox-LDL with or without Lisosan-G, showed an association especially in the first two cases, respectively (P<0.01, R2= 0.28; P<0.01, R2= 0.0055; P<0.06, R2= 0.40).
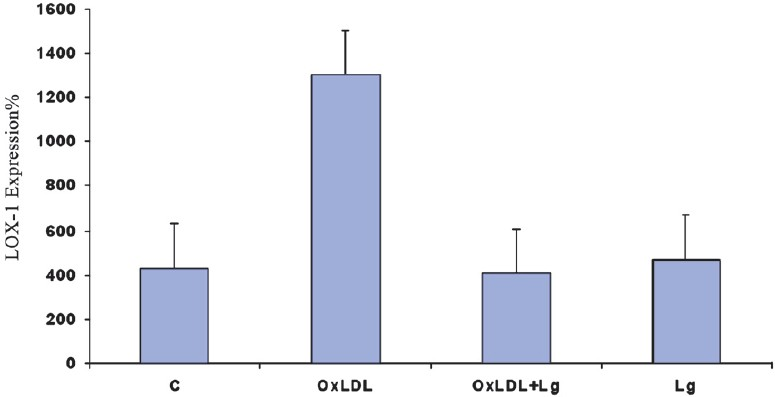
- Semi-quantitative RT-PCR analysis of LOX-1 gene after endothelial incubation with ox-LDL and Lisosan G.
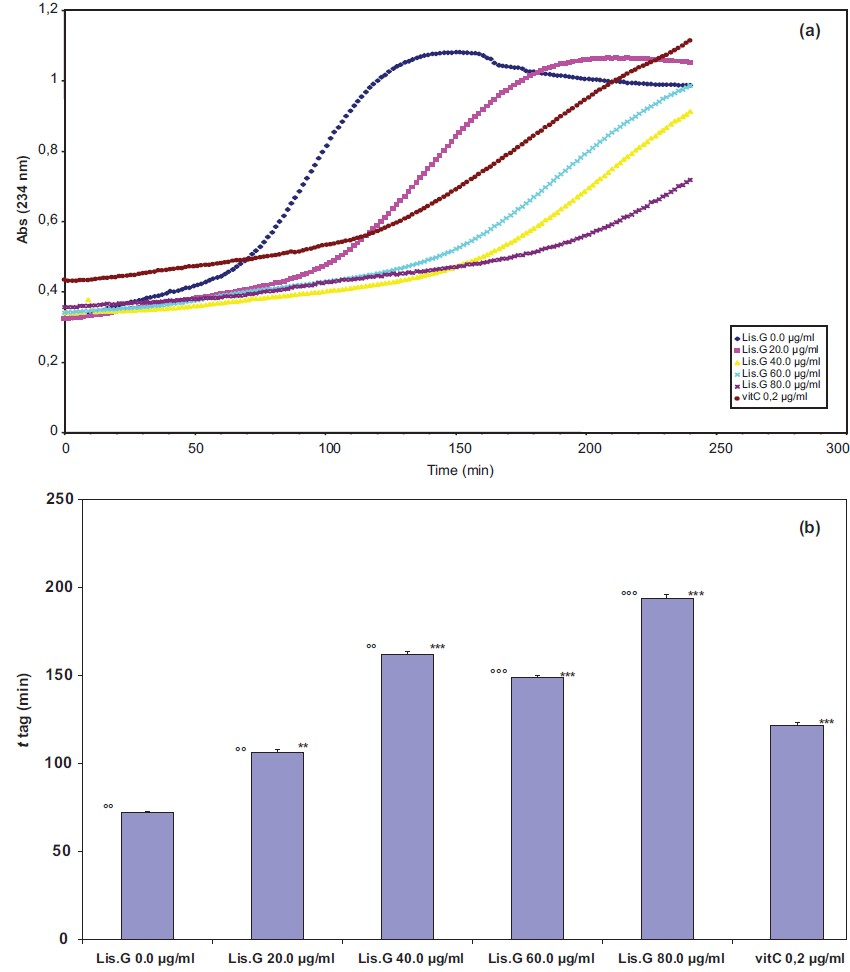
The analysis of the effect of Lisosan G on Cu++-mediated LDL oxidation is reported in Fig. 5.
-
(a): Kinetic curves of Cu++-induced LDL oxidation absence and in the presence of increasing doses of Lisosan G or in presence of vitamin C. (b) tlag increase in relation with the enhancement of Lisosan G dose. t lag of vitamin C was confronted. P**<0.01, **<0.001 compared to control; °°P<0.01 compared to
tlag of vitamin C X 0.2 μg/ml; °°°P<0.01 compared to tlag of vitamin C 0.2 μg/ml.
The calculated t lag, shows a significant increment in relation with the dose of Lisosan G. The effect of vitamin C (0.2 μg/ml), used as a positive control, showed a significant higher t lag respect to Lisosan (G 20 μg/ml), but significantly reduced respect to the other levels of Lisosan G.
Discussion
It is now well established that adhesion of monocytes to the endothelium is one of the earliest cellular events in atherogenesis. Several mechanisms promote cell-cell interaction between monocytes and endothelial cells. Our study demonstrated that ICAM-1 was basically expressed by HMEC-1 cells. Further, the inflammation process initiated by ox-LDL on cultured HMEC-1 cells has been shown to promote significantly the expression of adhesion molecule ICAM-120. In our study, ox-LDL induced significantly the expression of ET-1 (2-fold the control), IL-6 and LOX-1 (3-fold) compared to control. Similar results have been shown earlier2123.
The exposure to Lisosan-G not only reduced the effect of ox-LDL on ICAM-1 production, but also showed a significant reduction in ICAM-1 compared to control. This suggests the role of this natural compound to prevent the early events of atherosclerosis or microcirculatory dysfunction. Lisosan G co-incubated with ox-LDL partially reduced the increment of ET-1 suggesting that this effect seems not to be linked exclusively to the oxidation, but also to the presence of LDL, as described earlier by Lubrano et al21.
Except for ET-1, since the regulation of ICAM-1, IL-6 expression by ox-LDL appears to be the result of the redox activity of ox-LDL induced by oxygen free radicals present in the cellular environment. As a result, the rescue of oxygen free radicals by Lisosan G, during the 1 h pre-exposure period, could reduce the extension of the cellular oxidative stress induced by ox-LDL. Consequently, the levels of ICAM-1 and IL-6 in the medium were decreased at control level or below. The decrease in oxidative stress induced by Lisosan G was also shown by the significant reduction of MDA concentration, that is directly associated especially with the production of ICAM-1 and IL-6. These results were confirmed by PCR analysis for ICAM-1, IL-6 expression, and prepo-ET-1 mRNA. As previously reported the ET-1 biosynthesis is mediated by membrane-bound Zn2+- metalloproteases, endothelin-converting enzymes (ECE-1), which catalyze in vitro and in vivo the biotransformation of the inactive big endothelin to the biologically active ET-124. Elevated levels of this hormone have been implicated in the development of various pathophysiological disorders including hypertension, atherosclerosis and congestive heart failure25.
LOX-1 was initially identified as the major receptor for ox-LDL in endothelial cells and was later found to have an inducible expression in macrophages and smooth muscle cell2627. LOX-1 activation by ox-LDL binding stimulates intracellular signalling, gene expression and production of superoxide radicals2829. In vivo, its expression is enhanced in pro-atherogenic settings including hypertension, hyperlipidaemia, diabetes, and atherosclerosis.
It has been shown that solubile form of LOX-1 correlated with oxidative stress markers in stable coronary artery disease30. Our results showed that Lisosan G can inhibit the upregulation of LOX1 in endothelial cells. Lisosan G showed a strong ability to inhibit Cu++-induced lipid peroxidation in humans LDL suggesting strong antioxidant properties.
In conclusion, our results demonstrate that Lisosan G may be considered a potential candidate in the prevention of atherosclerosis and microcirculatory dysfunction reducing the oxidative/inflammatory process. Further, Lisosan G could be an important food supplement to prevent the damaging effect induced by oxidative stress on endothelial cells. Additional in vivo studies need to be carried out to confirm the beneficial effects of Lisosan G against endothelial cells damage.
Acknowledgment
The authors acknowledge Agrisan Company [Larciano (PT), Italy] for supplying Lisosan G.
References
- Microvascular disease relevance in the hypertension syndrome. Clin Hemorheol Microcirc. 2003;29:295-300.
- [Google Scholar]
- Is hypertension a tissue perfusion disorder.Implications for renal and myocardial perfusion? J Hypertens. 2006;24(Suppl):S10-6.
- [Google Scholar]
- Effect of ascorbic acid on microcirculation in patients with Type II diabetes: a randomized placebo-controlled cross-over study. Clin Sci (Lond). 2005;108:507-13.
- [Google Scholar]
- Oxidised lipoproteins may promote inflammation through the selective delay of engulfment but not binding of apoptotic cells by macrophages. Atherosclerosis. 2003;171:21-9.
- [Google Scholar]
- Theodore Cooper memorial Lecture. Hypertension and the pathogenesis of atherosclerosis. Oxidative stress and the mediation of arterial inflammatory response: a new perspective. Hypertension. 1995;25:155-61.
- [Google Scholar]
- Endothelial activation by hydrogen peroxide.Selective increases of intercellular adhesion molecule-1 and major histocompatibility complex class I. Am J Pathol. 1993;142:1598-607.
- [Google Scholar]
- Oxygen radicals as second messangers for expression of the monocyte chemoattractant protein, JE/MCP-1, and the monocyte colony-stimulating factors, CSF-1, in response to tumor necrosis factor-alpha and immunoglobulin G. J Clin Invest. 1993;92:1564-71.
- [Google Scholar]
- Monocyte chemoattractant protein-1 induces scavenger receptor expression and monocyte differentiation into foam cells. Biochem Biophys Res Comm. 2003;305:380-5.
- [Google Scholar]
- The binding of oxidized low density lipoprotein (ox-LDL) to ox-LDL receptor-1 reduces the intracellular concentration of nitric oxide in endothelial cells through an increased production of superoxide. J Biol Chem. 2001;276:13750-5.
- [Google Scholar]
- Alternative splicing produces a divergent cytoplasmic tail in the human endothelial thromboxane A2 receptor. J Biol Chem. 1995;270:7011.
- [Google Scholar]
- Relevance of nutritional antioxidants in metabolic syndrome, ageing and cancer: potential for therapeutic targeting. Infect Disord Drug Targets. 2009;9:400-14.
- [Google Scholar]
- A new insight into resveratrol as an atheroprotective compound: Inhibition of lipid peroxidation and enhancement of cholesterol efflux. Atherosclerosis. 2009;207:420-7.
- [Google Scholar]
- Resveratrol improves endothelial function: role of TNF{alpha} and vascular oxidative stress. Arterioscler Thromb Vasc Biol. 2009;29:1164-71.
- [Google Scholar]
- Effect of Lisosan G, a ground of grain, on the hepatic drug metabolizing enzymes and its protective role on carbon tetrachloride-induced hepatotoxicity. Biotechnol Lett. 2007;29:1155-9.
- [Google Scholar]
- Cisplatin induced toxicity in rat tissues: the protective effect of lisosan G. Food Chemi Toxicol. 2011;49:233-7.
- [Google Scholar]
- HMEC-1: establishment of an immortalized human microvascular endothelial cell line. J Invest Dermatol. 1992;99:683-90.
- [Google Scholar]
- Determination of aldehyde lipid peroxidation products: malonaldehyde and 4-hydroxinonenal. Meth Enzymol. 1990;186:407-21.
- [Google Scholar]
- Ginkgolide B suppresses intercellular adhesion molecule-1 expression via blocking nuclear factor-kappaB activation in human vascular endothelial cells stimulated by oxidized low-density lipoprotein. J Pharmacol Sci. 2009;110:362-9.
- [Google Scholar]
- Role of thromboxane A2 receptor on the effects of oxidized LDL on microvascular endothelium nitric oxide, endothelin-1, and IL-6 production. Microcirculation. 2008;15:543-53.
- [Google Scholar]
- Expression and localization of lectin-like oxidized low-density lipoprotein receptor-1 (LOX-1) in murine and human placentas. J Histochem Cytochem. 2008;56:773-84.
- [Google Scholar]
- The role of lipid peroxidation and antioxidants in oxidative modification of LDL. Free Radical Biol Med. 1992;13:341-90.
- [Google Scholar]
- Kinetic analysis of copper-induced peroxidation of LDL. Biochim Biophys Acta. 1998;1389:155-72.
- [Google Scholar]
- Antioxidant activity of plicatin B on cultured human microvascular endothelial cells exposed to H2O2. Drug Chem Toxicol. 2007;30:311-25.
- [Google Scholar]
- Endothelin converting enzyme: substrate specificity and inhibition by novel analogs of phosphoramidon. Biochem Biophys Res Commun. 1996;223:372-8.
- [Google Scholar]
- Pathophysiology of endothelin in the cardiovascular system. Annu Rev Physiol. 1999;61:391-415.
- [Google Scholar]
- An endothelial receptor for oxidized low-density lipoprotein. Nature. 1997;386:73-7.
- [Google Scholar]
- Identification of the lectin-like receptor for oxidized low-density lipoprotein in human macrophages and its potential role as a scavenger receptor. Biochem J. 1998;334:9-13.
- [Google Scholar]
- Modified low density lipoprotein and its constituents augment cytokine-activated vascular cell adhesion molecule-1 gene expression in human vascular endothelial cells. J Clin Invest. 1995;95:1262-70.
- [Google Scholar]
- Oxidized LDL regulates vascular endothelial growth factor expression in human macrophages and endothelial cells through activation of peroxisome proliferator-activated receptor-gamma. Arterioscler Thromb Vasc Biol. 2001;21:560-6.
- [Google Scholar]
- Serum soluble lectin-like oxidized low-density lipoprotein receptor-1 correlates with oxidative stress markers in stable coronary artery disease. Int J Cardiol Int J Cardiol. 2009;134:285-7.
- [Google Scholar]






