Translate this page into:
A ten year analysis of multi-drug resistant blood stream infections caused by Escherichia coli & Klebsiella pneumoniae in a tertiary care hospital
Reprint requests: Dr C. Wattal, Chairman, Department of Clinical Microbiology, Sir Ganga Ram Hospital, Rajinder Nagar, New Delhi 110 060, India e-mail: chandwattal@sgrh.com, chand_wattal@yahoo.com
-
Received: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background & objectives:
Extensive use of antibiotics has added to the escalation of antibiotic resistance. This study was undertaken to evaluate the association, if any between antibiotic use and resistance in a hospital setting, and also detect the predominant mechanism of antibiotic resistance in Escherichia coli and Klebsiella pneumoniae over a period of 10 years.
Methods:
In a retrospective study of 10 years, a total of 77,618 blood culture samples from 2000 to 2009 from indoor patients were screened and those yielding E. coli and K. pneumoniae were included in the study. Antibiotic susceptibility records as well as the percentage of ESBL producers were noted. A total of 423 isolates of 2009 were also screened for AmpC and carbapenemase production. Antibiotic consumption data of 10 years were analysed.
Results:
ESBL producing E. coli increased from 40 per cent in 2002 to 61 per cent in 2009, similarly there was a significant (P<0.05) rise in resistance to cefotaxime (75 to 97%), piperacillin-tazobactum (55- 84%) and carbapenem (2.4-52%) in K. pneumoniae. A significant (P<0.05) association was observed between resistance and consumption of carbapenem and piperacillin and tazobactum consumption in K. pneumonia.
Interpretation & conclusions:
Our study demonstrated a rise in consumption and resistance to broad spectrum antimicrobial agents and also established an association between consumption and resistance to these antibiotics. Over a period of 10 years, the emergence of pan-resistance in K. pneumoniae could be due to the production of carbapenemases whereas ESBL production was the common mechanism of resistance in E. coli. This study warrants a directed effort towards continued surveillance and antibiotic stewardship to minimize selection pressure and spread.
Keywords
Antibiotic resistance
blood stream infection
Escherichia coli
Klebsiella pneumoniae
The emergence of antibiotic resistance is a global public health problem. Gram-negative bacterial resistance is of particular importance as there is a dearth of novel antibiotics directed against these organisms. The clinical utility of carbapenems, the agents of last resort against multi-drug resistant Enterobacteriaceae is under threat with the growing incidence of pan resistant isolates12. Studies on the trends of antimicrobial consumption and resistance as well as the common mechanisms of resistance of multi-drug resistant Escherichia coli and Klebsiella pneumonia are scanty. Moreover, the organisms encountered in various hospitals around the country is far from uniform34. The emergence of multi-drug resistant and pan-resistant E. coli and K. pneumoniae and the lack of consistent data prompted us to conduct this study to demonstrate a relationship if any, between antimicrobial use and resistance over a period of ten years with reference to the common mechanism of resistance in these isolates in a tertiary care hospital in north India.
Material & Methods
This retrospective study was undertaken in a 650 bedded tertiary care hospital with an active transplant programme at New Delhi, India, to evaluate the emergence of antibiotic resistance in E. coli and K. pneumoniae over a period of ten years (2000-2009). The antibiotic consumption rate was also analysed. A total of 77,618 consecutive blood culture samples from in-patients admitted during the study period were evaluated and those yielding E. coli and K. pneumoniae were included in the study. All repeat isolates were excluded using speed-miner Hospital Information System (HIS) (Australia).
Blood culture isolates and susceptibility testing: BactT Alert 3D (bioMerieux, France) automated system was used to culture all the blood samples received. Blood culture bottles were incubated for seven days before being reported negative. Identification and antibiotic susceptibility testing of all these isolates were done using routine biochemical tests and standard Kirby-Bauer method for antibiotic susceptibility5 and subsequently from 2002 using VITEK 1 and VITEK - II from 2005 (bioMerieux, France) and interpreted as per CLSI guidelines6. Blood culture samples yielding E. coli and K. pneumonia were only included in the study. E. coli and K. pneumoniae were screened and confirmed for extended spectrum β-lactamase (ESBL) activity as per CLSI guidelines6. Besides the above method, antibiotic susceptibility was done subsequently by Vitek-2 which also confirmed the presence of ESBL.
Carbapenemase detection: All isolates of E. coli and K. pneumoniae in the year 2009 (423 isolates) were tested for the presence of carbapenemases using the modified Hodge test (MHT) as per the CLSI guidelines7. K. pneumoniae ATCC® BAA-1705 and ATCC® BAA- 1706 were used as positive and negative controls, respectively. Since MHT is a phenotypic screen for the presence of carbapenemase and does not differentiate between Class A KPC (K. pneumonia carbapenemase) and Class B MBL (metallo-β-lactamases), which are encountered in these isolates, all isolates were also screened for MBL production by using imepenem - EDTA combined disc diffusion test and MBL E-test (AB Biodisk, Solna, Sweden) method8.
AmpC screening: Since 2009 onwards all isolates were screened for Amp C β- lactamases. Though there are no CLSI guidelines for their detection, screening for AmpC was done using AmpC disc test method. This is a reliable, sensitive and economically viable method for diagnosing AmpC production in the laboratory9. All 423 isolates of 2009 were screened for AmpC production.
Antibiotic consumption data: The monthly antibiotic issued to the inpatients was obtained from HIS (Hospital Information System). The consumption of the antibiotics was finally expressed as number of DDDs (daily defined dosages)/100 days10. The following antibiotics were studied using the Anatomical Therapeutic Chemical (ATC) classification: cefotaxime (JOIDD01), amikacin (JOIGB06), ciprofloxacin (JOIMA02), piperacillin-tazobactum (JOICR05) and imipenem (JOIDH51) representing the third generation cephalosporins (3GC), aminoglycosides, fluoroquinolones, β-lactam and β-lactamase combination and carbapenems, respectively10. Antibiotic resistance data were analysed using a FoxPro based indigenously designed program till 2006 and after that speedminer program of HIS was used. The data were analysed in relation with antimicrobial resistance over a period of 10 years.
Statistical analysis: The data for each antibiotic prescription and resistance were first analyzed individually for studying the trend over time using the function Y=aebt. Taking log on both sides, log(y) = log (a) + b t, where b stands for the percentage growth rate per year. The growth rate was tested for its significance using t-test. The relationship between antibiotic resistance and consumption was further established using linear regression by fitting the linear function Y= a + bx, where x is the antibiotic consumption and y is the antibiotic resistance. Here b indicates the change in antibiotic resistance for each unit change in antibiotic consumption.
Results
A total of 77,618 blood samples were screened over a period of 10 years, of which 13153 samples (16.9%) were culture positive. Of these positive samples, 43.9 per cent (5,784 isolates) were positive for Gram negative bacilli. Amongst the Gram-negative isolates, 21.9 per cent isolates of K. pneumoniae (1271) and 19.06 per cent (1103) of E. coli were the most common Enterobacteriaceae isolated. The change in isolation rate of both K. pneumoniae and E. coli bacteraemia over a period of 10 years was 2.59 and 17.6 per cent, respectively which was statistically significant (P<0.05) (Table I). E. coli was the predominant organism till 2006 and was subsequently replaced by K. pneumoniae (Table I).
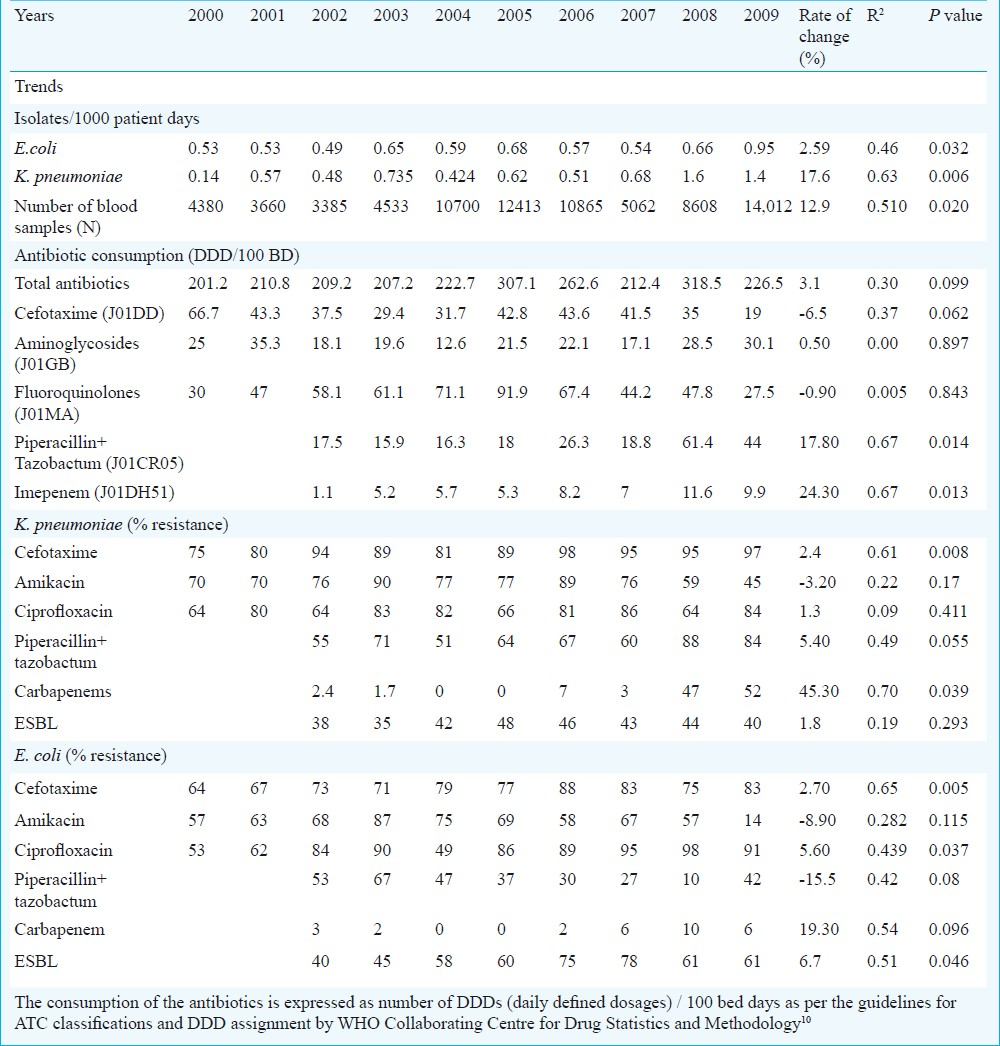
In K. pneumoniae there was a significant increase in resistance to cefotaxime, carbapenems and piperacillin-tazobactum over the years. On the other hand, significant antibiotic resistance in E. coli was observed to cefotaxime and ciprofloxacin (Table I). Tigecycline was introduced in the hospital formulary from 2007 and in the same year a resistance of 14 per cent was observed which further increased to 20 per cent in 2009 in K. pneumoniae. However, in E. coli the resistance to tigecycline remained 1.7 per cent in 2008 and increased marginally to 3 per cent in 2009. All the isolates remained sensitive to colistin.
There was a significant (P<0.05) rise in ESBL producers in E. coli from 40 to 61 per cent over a period of 10 years and the rate of change was 6.7 per cent. No such change was observed in K. pneumoniae during the study period. However, a decrease in ESBL producers in K. pneumoniae was noticed from 2006 onwards though not statistically significant (Table I).
Due to the rise in carbapenem resistance, all the isolates of K. pneumoniae and E. coli were screened for carbapenemase and Amp C production from 2009 to determine the mechanism of resistance. A total of 423 isolates (167 E. coli and 256 K. pneumoniae) were screened. More than half of the total 256 isolates of K. pneumoniae (130 isolates, 51%) were MHT positive thus carbapenemase producers. Of these, carbapenemase producers in K. pneumoniae, 103 (79%) were MBL producers with MBL E-test and imepenem - EDTA combined disc test positive. In E. coli, of the total of 167 isolates, 25(15%) were MHT positive and thus carbapenemase producers. Of these, seven (28%) were MBL producers and were MBL E-test and combined disc test positive. The remaining 18 (72%) were all class A KPC producers i.e. these were only MHT positive and MBL E-test and combined disc test negative and were resistant to carbapenems. All the 423 isolates of 2009 were screened for AmpC production and 8 per cent of the isolates of both K. pneumoniae (20) and E. coli (13) were AmpC positive.
Though the total antibiotic consumption did not show a significant change over a period of 10 years but there was a significant increase in prescription of broad spectrum antibiotics like piperacillin and tazobactum (JOICR05) from 17.5 to 44 DDD/100 days and imepenem (JOIDH51) from 1.1 to 9.9 DDD/100 days (P<0.05) at the rate of 17.8 and 24.3 per cent, in 10 years, respectively (Table I).
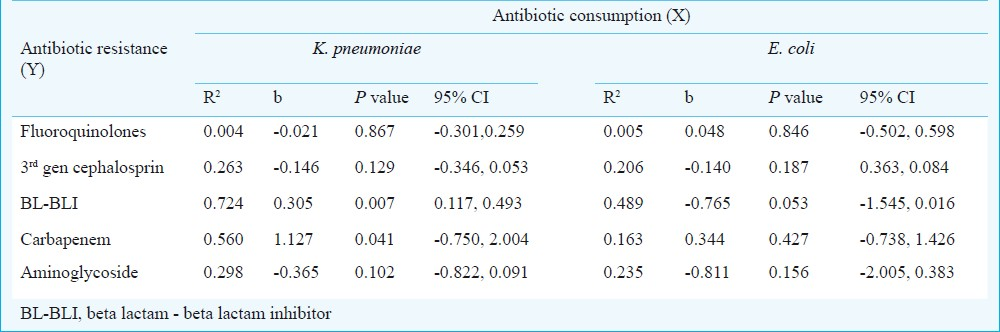
Table II demonstrates the linear regression analysis used to establish the strength of the relationship between consumption and its resistance. There was a significant association (P<0.05) between rise in antibiotic resistance and increase use of piperacillin- tazobactum combination (JOICR05) and carbapenem (JOIDH51) in K. pneumoniae.
Discussion
Our study highlights the extensive consumption of broad spectrum antimicrobial agents coupled with high resistance rates to these agents among the isolates surveyed. There was a significant rise in ESBL isolates with an increase in 3GC and quinolone resistance in E. coli. In K. pneumoniae, an increase in resistance to 3GC, piperacillin–tazobactum and carbapenem was observed. Increase in the incidence of multi-drug resistant E. coli has been reported in various studies11–13. In the SMART study conducted in Asia Pacific region, the ESBL rate in India amongst E. coli was also alarmingly high (79%)14.
A multi-centric study conducted in 2004-2006 reported the highest ESBL rates in K. pneumoniae from India (72%)15. In this study, the ESBL producers in K. pneumoniae also increased to a high of 74 per cent till 2005 but has shown a fall after that. Emergence of other mechanisms of resistance like AmpC and carbapenemase producers may have contributed to this phenomenon. It is a known fact that AmpC β-lactamases and carbapenemases when present along with ESBL may mask the phenotype of the latter1617.
The increasing resistance to piperacillin-tazobactum combination and carbapenems seen in K.pneumoniae in the study period may be attributed to presence of carbapenemase producing isolates. Though AmpC producers along with porin loss may contribute to carbapenem resistance also but in our experience 8 per cent of E. coli and K. pneumoniae that were AmpC producers were all carbapenem sensitive. Other studies from India also have reported AmpC prevalence of 8-43 per cent16.
Carbapenemases both class A and class B (KPC and MBL) have shown a worldwide dissemination and probably are the major contributors of carbapenem resistance18. These KPCs and MBLs were the main contributors of pan-resistance in our study. MBL producers amongst K. pneumoniae isolates is on the rise worldwide and in India19. In this study, it was interesting to note that though there was an increase in ESBL producers amongst E. coli, the antibiotic pressure due to increased use of piperacillin-tazobactum and carbapenems did not highlight pan-resistance in E. coli as was seen in K. pneumoniae. This phenomenon is difficult to explain. Probably a preferential selection of pan-resistant K.pneumoniae could have occurred as a result of fitness cost under antibiotic pressure. Further genotypic evaluation is needed to know whether the high prevalence of MBL in K. pneumoniae is due to the presence of blaNDM-1 which is now on the rise19. In a pilot study conducted at our hospital MDR K. pneumoniae were found to be blaNDM-1 positive using PCR method (unpublished).
Though there is a paucity of data on trends of antibiotic consumption from India, the available data suggest that it is higher than other developing nations of the world2021. Rates are further lower in developed nations22. Use of carbapenem and piperacillin- tazobactum has increased significantly in 10 years. A study done by our group earlier (1995-2001) showed a significant increase in consumption of 3GC23. Rise in 3GC resistance due to emergence of ESBL producers resulted in a shift to usage of piperacillin-tazobactum and carbapenems causing significant increasing consumption of these broad spectrum antibiotics in our study. Such increasing trend of carbepenem and piperacillin-tazobactum use was also seen in various studies conducted in hospitals world over112425.
The increase in antibiotic resistance is due to several factors but the major cause appears to be excessive use of antibiotics26. Our study showed a significant association between increased use and resistance to carbapenems and piperacillin and tazobactum combination in K. pneumoniae isolates as has been shown earlier1127.
Screening for carbapenemase activity by the laboratory is the first step towards early detection and continued surveillance of these pan-resistant isolates.
There are several limitations of this work. As this study is retrospective in nature, potential confounders such as changes in length of stay, shift of patients from the ICU to the ward and vice versa, case stratification, time of collection of blood samples could not be ascertained while observing the trends. Hence cases could not be differentiated from hospital acquired infections and otherwise. Genotypic identification of the common mechanisms of resistance in these MDR isolates of Enterobacteriaceae was also not done.
In conclusion, our study highlights alarming increase in resistance and antibiotic use and the emergence of MDR isolates amongst E. coli and K. pneumoniae, and emphasizes on prompt remedial actions to salvage the situation. Reducing consumption by judicious use is the first intervention in the direction of antibiotic surveillance. There is an urgent need for early detection of these isolates for better treatment outcomes.
Acknowledgment
The authors thank Prof. Peter M. Hawkey, Professor of Clinical & Public Health Bacteriology and Honorary Consultant Microbiologist, Health Protection Agency, Heart of England NHS Trust UK, for his valuable suggestions, and Ms. Parul Takkar Chugh for statistical analysis.
References
- Carbapenemases: a brief review for pediatric infectious disease specialists. Pediatr Infect Dis J. 2010;29:68-70.
- [Google Scholar]
- Carbapenemaseproducing Enterobacteriaceae, U.S. rivers. Emerg Infect Dis. 2005;11:260-4.
- [Google Scholar]
- Nosocomial bacteraemia in intensive care unit patients of a tertiary care centre. Indian J Med Res. 2005;122:305-8.
- [Google Scholar]
- Device-associated nosocomial infection rates in intensive care units of seven Indian cities. Findings of the International Nosocomial Infection Control Consortium (INICC) J Hosp Infect. 2007;67:168-74.
- [Google Scholar]
- Anti-microbial susceptibility testing. Clinical microbiology procedures handbook (2nd ed). Washington DC: AM Press; 2007.
- Clinical and Laboratory Standards Institute (CLSI). 2006. In: Performance standards for antimicrobial susceptibility testing. 16th Informational Supplement (M100-S16). Wayne, PA: CLSI; 2006.
- [Google Scholar]
- Clinical and Laboratory Standards Institute (CLSI). 2009. In: Performance standards for antimicrobial susceptibility testing, 19th Information Supplement (M100-S19). Wayne, PA: CLSI; 2009.
- [Google Scholar]
- Phenotypic detection of carbapenem-susceptible metallo-beta-lactamase-producing Gram-negative bacilli in the clinical laboratory. J Clin Microbiol. 2006;44:3139-44.
- [Google Scholar]
- Evaluation of methods for AmpC beta-lactamase in Gram negative clinical isolates from tertiary care hospitals. Indian J Med Microbiol. 2005;23:120-4.
- [Google Scholar]
- WHO Collaborating Centre for Drug Statistics Methodology. In: Guidelines for ATC Classifications and DDD Assignment. Oslo, Norway: WHO Collaborating Centre; 2002.
- [Google Scholar]
- BSAC Working Parties on Resistance Surveillance. Non-susceptibility trends among Enterobacteriaceae from bacteraemias in the UK and Ireland, 2001-06. J Antimicrob Chemother. 2008;62(Suppl 2):ii41-54.
- [Google Scholar]
- Dramatic increase of third-generation cephalosporin-resistant E. coli in German intensive care units: secular trends in antibiotic drug use and bacterial resistance, 2001 to 2008. Crit Care. 2010;14:R113.
- [Google Scholar]
- Emergence of high levels of extended-spectrum-ß-lactamase-producing gram-negative bacilli in the Asia-Pacific region: data from the Study for Monitoring Antimicrobial Resistance Trends (SMART) program, 2007. Antimicrob Agents Chemother. 2009;53:3280-4.
- [Google Scholar]
- Antimicrobial susceptibility among organisms from Asia/Pacific Rim, Europe and Latin and North America collected as part of TEST and the in vitro activity of tigecycline. J Antimicrob Chemother. 2007;60:1018-29.
- [Google Scholar]
- Detection of Amp C beta lactamases production in Escherichia coli & Klebsiella by an inhibitor based method. Indian J Med Res. 2007;126:220-3.
- [Google Scholar]
- Use of boronic acid disk tests to detect extended-spectrum beta-lactamases in clinical isolates of KPC carbapenemases-possessing Enterobacteriaceae. J Clin Microbiol. 2009;47:3420-6.
- [Google Scholar]
- The changing epidemiology of resistance. J Antimicrob Chemother. 2009;64(Suppl 1):i3-10.
- [Google Scholar]
- New Delhi Metallo-β lactamase (NDM-1) in Enterobacteriaceae: treatment options with carbapenems compromised. J Assoc Physicians India. 2010;58:147-9.
- [Google Scholar]
- Prescribing patterns of antibiotics and sensitivity patterns of common microorganisms in the internal medicine ward of a teaching hospital in Western Nepal : a prospective study. Ann Clin Microbiol Antimicrob. 2003;2:7.
- [Google Scholar]
- Trends in antimicrobial utilization in a university hospital, 1990-1996. Rev Saude Publica. 2002;36:553-8.
- [Google Scholar]
- Quantitative antibiotic use in hospitals: comparison of measurements, literature review, and recommendations for a standard of reporting. Infection. 2008;36:549-59.
- [Google Scholar]
- Prescription auditing and antimicrobial resistance at a tertiary care hospital at New Delhi, India. J Hosp Infect. 2005;59:156-8.
- [Google Scholar]
- Antibiotic consumption and development of resistance among Gram-negative bacilli in intensive care units in Oman. Ann Saudi Med. 2000;20:324-7.
- [Google Scholar]
- Control of extended-spectrum â-lactamase-producing Escherichia coli and Klebsiella pneumoniae in a children's hospital by changing antimicrobial agent usage policy. J Antimicrob Chemother. 2007;60:629-37.
- [Google Scholar]
- Methodology for surveillance of antimicrobials use among out-patients in Delhi. Indian J Med Res. 2009;129:555-60.
- [Google Scholar]
- High rates of resistance to piperacillin/tazobactum among Escherichia coli and Klebsiella pneumoniae strains isolated in a Greek hospital. Diagn Microbiol Infect Dis. 1997;29:39-41.
- [Google Scholar]






