Translate this page into:
Trend of immunization & gap in vaccine doses as observed in National Family Health Survey rounds in India
#Equal contribution
For correspondence: Dr Kirtan Rana, Department of Community Medicine, Gian Sagar Medical College & Hospital, Patiala 140 401, Punjab, India e-mail: ranakirtan006@gmail.com
-
Received: ,
Accepted: ,
Abstract
Background & objectives
Immunization is an efficient and cost-effective way of lowering the infectious disease related morbidity and mortality in the community. The current study reviewed the trend of immunization, gaps in doses of vaccine given at the same time and gaps between the doses of same vaccine from National Family Health Survey (NFHS 1-5) rounds.
Methods
The current study extracted data from all five NFHS rounds conducted from 1992-93 to 2019-21. The study analyzed the State-wise and demography-wise distribution of trends of immunization from NFHS-1 to NFHS-5. State wise distribution of change in vaccination coverage between NFHS-4 and 5 was analyzed. The study also assessed the State-wise trends of fully vaccinated and unvaccinated children from NFHS 1-5.
Results
The northeastern States had maximum gap between the vaccination given at birth i.e., 47.3 per cent between BCG and Hepatitis B, and 32.8 per cent between BCG and birth dose of OPV in Manipur in NFHS -5. A gradual rise in the percentage of male (40.2%) and female (41.9%) childrens’ vaccination was found across the NFHS rounds with reduction in gap between the male and female vaccination from NFHS-1 (2.6%) to NFHS-5 (0.9%). The percentage of vaccination decreased proportionately with birth order. The vaccination coverage has increased in both urban and rural population, but the rise was higher in rural (45.9%) areas than urban (24.8%). An increase in percentage of fully vaccinated children by 41.2 per cent and decrease in percentage of non-vaccinated children by 26.4 per cent was observed from NFHS-1 to NFHS-5.
Interpretation & conclusions
Our analysis clearly suggests that immunization coverage has improved over a period of time but the variability in vaccine coverage across States and gap in vaccine doses needs attention of the policy makers to cover this for achieving our national immunization goals.
Keywords
BCG
measles
rubella
NFHS
vaccine dose gap
children
coverage
immunization
missed dose
vaccine
Immunization is one of the vital components of public health and for disease prevention. It is an efficient and cost- effective way of lowering the infectious disease related morbidity and mortality whilst improving the quality of life (QOL) in the community1. A variety of diseases that once contributed to substantial morbidity and mortality have been controlled and eradicated due to various immunization initiatives by the Government2,3. In order to reduce the morbidity, mortality and disability among children, the Government of India (GoI) launched the Expanded Programme on Immunization (EPI) in 1978 to prevent children from six serious preventable diseases namely diphtheria, pertussis and tetanus (DPT), tuberculosis, poliomyelitis and measles4. In order to fill up the deficit pockets, the GoI launched Mission Indradhanush in December 2014 to increase the proportion of immunization of under-vaccinated and unvaccinated children which was later on revamped into Intensified Mission Indradhanush (IMI) in 2017 and IMI 2.0 in 2019 as part of an extensive effort to speed up the progress5,6. Among other efforts, immunization services are strengthened by adopting robust record-keeping system like vaccination cards and, mother and child protection (MCP) cards. Additional efforts in this direction include improvement of vaccination supply chain networks across the nation by a cutting-edge technological innovation named the electronic Vaccination Intelligence Network (eVIN)7-9.
The variations in vaccination coverage are influenced by a variety of parameters, including the child’s gender and birth order, maternal age and education, the geographical location, the place of residence (rural or urban), etc10,11. Other obstacles to immunization are shortage of trained personnel, especially in remote and inaccessible locations, ineffective maintenance of cold chain, subpar communication and surveillance, and, inadequate laboratory network12. Lack of awareness and parental vaccine hesitancy are also causes for concern, influenced by a variety of cultural, personal, and vaccine-related factors such as rumours and concerns about the cost, benefit, and safety of immunization13. Despite the efforts and the advances made, immunization coverage still seems to be below the fixed target levels as it is influenced by many sociocultural and demographic factors. Another important aspect of the immunization in Sustainable development goals (SDG) is to reach the ‘zero dose’ children which means those children who have not received any routine vaccination.
National Family Health Survey (NFHS) was started in India in 1992 which collected information on vital parameters including the immunization coverage with some behaviour related questions ( https://www.nfhsiips.in/nfhsuser/index.php#). The NFHS-4 was conducted in 2015-16 after which the world faced COVID-19 pandemic 2020. The COVID-19 pandemic affected healthcare in its routine care services including immunization services. Although it was claimed that the routine immunization services didn’t suffer much during COVID-19 pandemic from the Government’s side, but various other factors may have affected the utilization rates such as lockdown in the area, availability of means of transport, information about immunization during COVID-19. So far in India, five NFHS surveys have been conducted (latest, 5th NFHS in 2019-21) which have captured vital information regarding immunization and used as a basis for revamping many existing policies related to health based on the reports generated14-18.
India has set a target for reducing neonatal mortality below 12 per 1000 live births and under-5 mortality below 25 per 1000 live births by the year 2030 as per SDG target 3.219. A constant monitoring and evaluation of any programme is critical in finding out the scope and level of services being indented under that programme. The current study assessed the difference in vaccination coverage which are given at the same time in NFHS-5 and difference in coverage of similar vaccine between NFHS-4 and NFHS-5. The study also assessed the coverage of immunization in rural and urban area wise, male and female wise and vaccine coverage based on birth order from NFHS-1 to NFHS-5.
Material & Methods
The current study was a secondary data analysis of India’s five NFHS surveys conducted from 1992-93 to 2019-2114-18. The survey included people from different age groups and gender covering all States and Union Territories of India. The NFHS survey uses a stratified two stage sampling technique for recruiting participants. The data was collected from primary sampling units (PSUs) in rural areas and census enumeration blocks (CEBs) in urban areas. The detailed methodology of NFHS can be read from the NFHS reports.
The current study extracted State-wise information on immunization rates in NFHS-4, NFHS-5 for vaccination of children in their first year of life, demographic distribution of immunization at the national level, residence wise immunization status at national level, immunization rate based on birth order for children between 12 to 23 months of age as presented in the NFHS-4 and NFHS-5 reports.
The NFHS-1 included survey for BCG (Bacillus Calmette-Guérin), DPT, polio and measles14. The NFHS-2 and NFHS-3 collected additional information on polio dose at birth (polio 0) besides what was in NFHS-115,16. The NFHS-4 collected information on hepatitis B (Hep B) vaccine in addition to vaccines-BCG, DPT, polio and measles17. The NFHS-5 collected information on BCG, hepatitis, pentavalent/DPT, polio, measles/measles, mumps, and rubella (MMR)/measles and rubella (MR)/measles-containing vaccine (MCV)18.
Chhattisgarh, Jharkhand, Uttaranchal, and Tripura were included from NFHS-3 onwards while Andaman and Nicobar, Chandigarh, Dadra and Nagar Haveli, Lakshadweep, Pondicherry, Telangana and Daman and Diu were included from NFHS-4 onwards17. Union Territory of Jammu and Kashmir and Ladakh were included only in the last survey, although in previous surveys these were considered together as Jammu and Kashmir State18. Nagaland was not part of NFHS-316.
Statistical Analysis
The data was entered and analyzed in the Microsoft excel. The study calculated the difference between vaccinations with a tendency to be administered at the same time. Absolute differences were calculated between the various vaccines given to children and status of fully vaccinated and no vaccination between NFHS-4 and NFHS-5.
Results
The northeastern States (Manipur, Meghalaya, Nagaland, Tripura, Assam, and Mizoram) had maximum gap between the vaccination given at birth i.e., BCG and OPV (oral polio vaccine) (32.8%, 30.5%, 26%, 24.8%, 22%, 18.4%, respectively) and BCG and Hep B (47.3%, 42.8%, 44.7%, 33.5%, 38.6% and 23.6%, respectively) as observed in NFHS-5. The maximum difference observed between pentavalent and polio vaccine was in its third dose in Andhra Pradesh (13.5%) and Tripura (12.5%) while the lowest was in Manipur (-1.7%) and Nagaland (-1.7%) in its first dose in NFHS-5. The maximum difference in coverage of pentavalent first to the third dose was observed in Nagaland (12.5%) and Manipur (11.9%), for polio vaccine first to the third dose was observed in Nagaland (20.5%) and Manipur (19.5%), for Hep B first to the third dose was observed in Nagaland (14.6%) and Meghalaya (11.9%) in NFHS-5 as presented in Table I.
| NFHS | BCG-OPV (birth dose) | BCG-Hep B (birth dose) | Penta-Polio (1st dose) | Penta-Polio (2nd dose) | Penta-Polio (3rd dose) | Penta (1st-3rd) | Polio (1st-3rd) | Hep (1st-3rd) |
|---|---|---|---|---|---|---|---|---|
| India | 9.7 | 27.8 | 1.2 | 2.9 | 6.5 | 6.6 | 11.9 | 7.6 |
| Chandigarh | 3.2 | 9.5 | 0.7 | 4.1 | 7 | 5.5 | 11.8 | 5.6 |
| Delhi | 5.5 | 21.6 | 1.7 | 2.9 | 4.8 | 8.7 | 11.8 | 9.2 |
| Haryana | 9.6 | 28.3 | 3.8 | 5.9 | 8.1 | 5.3 | 9.6 | 6.3 |
| Himachal Pradesh | 2.4 | 5.8 | 1 | 1.3 | 6 | 1.9 | 6.9 | 1 |
| Jammu & Kashmir | 2.3 | 7 | 1.1 | 1.3 | 5.2 | 1.8 | 5.9 | 2.8 |
| Ladakh | 2.2 | 9.3 | 1.1 | 2.5 | 6.8 | 4.1 | 9.8 | 2.2 |
| Punjab | 2.7 | 9.5 | 0.3 | 3 | 8.8 | 5.2 | 13.7 | 6.6 |
| Rajasthan | 4.8 | 20.6 | -0.2 | 1.5 | 4.8 | 5.2 | 10.2 | 5.7 |
| Uttarakhand | 8.4 | 26.7 | 1.6 | 2.7 | 5.7 | 5.1 | 9.2 | 6.3 |
| Chhattisgarh | 5.8 | 25.8 | 0.6 | 2.2 | 3.3 | 7.7 | 10.4 | 8.1 |
| Madhya Pradesh | 4.1 | 13.5 | 1.6 | 3.6 | 6.5 | 6.1 | 11 | 7.9 |
| Uttar Pradesh | 15.9 | 42.8 | 2.6 | 4.2 | 7 | 9.6 | 14 | 10.3 |
| Bihar | 14.4 | 27.3 | 1.3 | 3.6 | 9.7 | 8.4 | 16.8 | 9.5 |
| Jharkhand | 17.7 | 33.7 | 3.9 | 5.3 | 9.3 | 6.5 | 11.9 | 7.5 |
| Odisha | 3.5 | 8.7 | 1 | 1.8 | 3.3 | 2.3 | 4.6 | 2.6 |
| West Bengal | 9.8 | 28.4 | 0.1 | 1 | 4.5 | 2.4 | 6.8 | 3.6 |
| Arunachal Pradesh | 11.6 | 22.8 | 6 | 7 | 8.6 | 9 | 11.6 | 10.5 |
| Assam | 22 | 38.6 | 1.6 | 3.1 | 9.1 | 8.2 | 15.7 | 10.7 |
| Manipur | 32.8 | 47.3 | -1.7 | -0.7 | 5.9 | 11.9 | 19.5 | 11.8 |
| Meghalaya | 30.5 | 42.8 | -1.9 | 1.1 | 5 | 8.7 | 15.6 | 11.9 |
| Mizoram | 18.4 | 23.6 | 3.6 | 4.2 | 4.7 | 4.6 | 5.7 | 4.1 |
| Nagaland | 26 | 44.7 | -1.7 | 1.3 | 6.3 | 12.5 | 20.5 | 14.6 |
| Sikkim | 4.4 | 9 | 1.9 | 1.9 | 4.3 | 1.8 | 4.2 | 5.2 |
| Tripura | 24.8 | 33.5 | 6.3 | 8.6 | 12.5 | 8.7 | 14.9 | 10.6 |
| Dadra and Nagar Haveli & Daman and Diu | 6.1 | 28.2 | -0.2 | -0.3 | 1.1 | 0.6 | 1.9 | 2.5 |
| Goa | 5.9 | 17.7 | 0 | -0.8 | 2.5 | 7.1 | 9.6 | 3.7 |
| Gujarat | 9.3 | 31.9 | -0.9 | 0.9 | 6.6 | 6.4 | 13.9 | 7.4 |
| Maharashtra | 7.5 | 43.3 | 0.4 | 2.2 | 4.6 | 8.8 | 13 | 10.4 |
| Andaman and Nicobar Islands | 5.7 | 38.7 | 1.7 | 8 | 11.9 | 5 | 15.2 | 6.7 |
| Andhra Pradesh | 2.8 | 15.1 | 1.9 | 5 | 13.5 | 4.5 | 16.1 | 6.5 |
| Karnataka | 3.5 | 12.6 | 0.4 | 1.4 | 4.8 | 3.6 | 8 | 4.2 |
| Kerala | 5.1 | 16.2 | 0.6 | 2.2 | 1.8 | 9.9 | 11.1 | 10.7 |
| Lakshadweep | 0 | 0 | 0 | 2.5 | 4.9 | 0 | 4.9 | 0 |
| Puducherry | -3.4 | 15.3 | 1.5 | 2.2 | 5 | 7.1 | 10.6 | 7.4 |
| Tamil Nadu | 0.7 | 12.7 | 0.9 | 1.2 | 3.4 | 2.6 | 5.1 | 3.4 |
| Telangana | 5.4 | 19.6 | 2 | 4.4 | 7.7 | 3.2 | 8.9 | 4.1 |
NFHS, National Family Health Survey; BCG-OPV, Bacillus Calmette-Guerin-Oral polio vaccine; BCG-Hep, Bacillus Calmette-Guerin-Hepatitis
Table II presents the change in coverage of vaccination in different States between NFHS-4 and NFHS-5. Lakshadweep (-5.8%), Telangana (-3.9%) and Puducherry (-3.5%) observed maximum fall in BCG coverage while Telangana (-7.2%), Goa (-5.6%) and Lakshadweep (-4.2%) observed maximum fall in birth dose of OPV from NFHS-4 to NFHS-5. Lakshadweep (-5.8%), Sikkim (-3.8%) and Andhra Pradesh (-3.5%) observed maximum fall in first pentavalent/DPT dose, Lakshadweep (-5.8%), Punjab (-4.2%) and Chhattisgarh (-3%) observed maximum fall in second pentavalent/DPT dose while Chandigarh (-8%), Punjab (-6%), and Kerala (-4.5%) observed maximum fall in third pentavalent/DPT dose from NFHs-4 to NFHS-5. Lakshadweep (-7.5%), Sikkim (-5.7%) and Telangana (-5.4%) observed maximum fall in first polio dose, Lakshadweep (-10.5%), Punjab (-7.4%) and Kerala (-4.5%) observed maximum fall in second polio dose while Punjab (-14%), Puducherry (-8.1%) and Lakshadweep (-6%) observed maximum fall in third polio dose from NFHS-4 to NFHS-5. Chandigarh (-8%), Punjab (-5%) and Chhattisgarh (-3.7%) observed maximum fall in MR dose from NFHS-4 to NFHS-5. Punjab (-12.8%), Pondicherry (-8.9%) and Goa (-6.5%) observed maximum fall in number of fully vaccinated children from NFHS-4 to NFHS-5. Lakshadweep (5.8%), Telangana (4.3%) and Andhra Pradesh (2.4%) reported maximum rise in number of ‘no-vaccination or zero dose’ children between NFHS-4 and NFHS-5.
| NFHS | BCG | OPV (B) | Pentavalent (dose) | Polio (dose) | MR | FV | NV | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 | 2 | 3 | ||||||
| India | 3.3 | 6.4 | 4.1 | 5.7 | 8.6 | 1.6 | 2.5 | 7.7 | 6.8 | 14.6 | -2.4 |
| Chandigarh | 0.9 | 0.4 | -2.5 | -2.5 | -8 | 0 | -0.8 | 1.4 | -8 | 1.4 | -0.9 |
| Delhi | 1.7 | 7.4 | 0.4 | 1.4 | 0.2 | -2.2 | -2.1 | 1.2 | -1 | 7.2 | 0.4 |
| Haryana | 2.1 | 1.5 | 6.4 | 8.6 | 12.2 | 0 | 1.6 | 5.3 | 10.4 | 14.7 | -2.3 |
| Himachal Pradesh | 3.4 | 20 | 2.8 | 5.5 | 11.1 | 2.4 | 4.3 | 7.7 | 8.4 | 19.7 | -0.9 |
| Jammu & Kashmir | -0.5 | 0.1 | 0.5 | 2.4 | 4.7 | -0.8 | 1.1 | 3.8 | 5.5 | 11.1 | 0.8 |
| Punjab | -2.9 | -4.2 | -3 | -4.2 | -6 | -4.1 | -7.4 | -14 | -5 | -12.8 | 2 |
| Rajasthan | 6.8 | 14.5 | 8.5 | 11.5 | 17.8 | 6.9 | 9.9 | 19.2 | 13 | 25.7 | -4.8 |
| Uttarakhand | 2.4 | 13 | 4.1 | 7.8 | 9.8 | 2.8 | 7.7 | 16.1 | 10.5 | 23.5 | -1.6 |
| Chhattisgarh | -2 | 0 | -2.7 | -3 | -3.9 | -3.3 | -3.7 | 2.5 | -3.7 | 3.3 | 1.7 |
| Madhya Pradesh | 3.8 | 8.7 | 4.3 | 8 | 14.5 | 3.5 | 7.6 | 17.8 | 8.5 | 23.8 | -2.5 |
| Uttar Pradesh | 5.6 | 13.2 | 7.2 | 9.9 | 14.8 | 1.5 | 2.8 | 6 | 12.6 | 18.8 | -3.8 |
| Bihar | 3.9 | 4.8 | 3.4 | 3.7 | 5.1 | 2.4 | 2.2 | 2.6 | 6.3 | 9.3 | -3.3 |
| Jharkhand | -0.8 | 7.2 | -1 | 0.6 | 3.7 | -4.2 | -3.5 | 2.9 | 4.3 | 12.2 | 0.9 |
| Odisha | 3.2 | 4.8 | 4.2 | 4.4 | 5.8 | 3 | 3.6 | 8.9 | 8 | 12.1 | -3.7 |
| West Bengal | 1.1 | 6.9 | 1.1 | 1.6 | 2.6 | 0.9 | 0.9 | 2.9 | 1.6 | 3.8 | -1.2 |
| Arunachal Pradesh | 17 | 31.2 | 18.2 | 21.9 | 25.3 | 5.4 | 9.4 | 15.3 | 26.1 | 26.7 | -10.3 |
| Assam | 10.2 | 13.9 | 9.3 | 10.5 | 16 | 6.1 | 9.3 | 17.4 | 11.4 | 19.6 | -8.6 |
| Manipur | 4.2 | 24.1 | 3 | 2.4 | 3.7 | 1.8 | 0.4 | -1 | 2.5 | 3 | -2.4 |
| Meghalaya | 3.4 | 5.7 | -0.8 | -1.1 | -0.4 | -2.1 | -3.1 | -2.4 | 0.7 | 2.6 | -2.2 |
| Mizoram | 8.1 | 17.6 | 10 | 12.5 | 19 | 5.4 | 8 | 14.4 | 19.7 | 22 | -8.5 |
| Nagaland | 17.4 | 13.6 | 16.4 | 19.2 | 20.1 | 9.7 | 11.4 | 13.3 | 23.9 | 22.5 | -11.9 |
| Sikkim | -2.3 | -2.6 | -3.8 | -2.4 | 0.3 | -5.7 | -1.7 | 1.3 | -2.8 | -0.5 | 2 |
| Tripura | 12.3 | 20.6 | 14.2 | 13 | 14.8 | 2.5 | 3.6 | 3.3 | 16.6 | 15 | -11 |
| Dadra and Nagar Haveli & Daman and Diu | 13.8 | 12.3 | 19.9 | 20.9 | 23.2 | 13.7 | 16.8 | 21.7 | 17.1 | 28.6 | -15 |
| Goa | -2.1 | -5.6 | 2 | 1.7 | -3.4 | -2.1 | -0.8 | -4.6 | -3.6 | -6.5 | 2.1 |
| Gujarat | 6.8 | 8.2 | 7.3 | 8.5 | 13.5 | 5.1 | 4.5 | 17.3 | 11.8 | 26 | -4.3 |
| Maharashtra | 3.8 | 3.5 | 6.6 | 8.3 | 8.8 | 3 | 2.7 | 12 | 2.2 | 17.4 | -3 |
| Andaman and Nicobar Islands | 10.8 | 7 | 10.4 | 10.1 | 9.3 | 8.7 | 2.1 | -2.9 | 7.6 | 6.7 | -10.8 |
| Andhra Pradesh | -2.6 | -1.3 | -3.5 | -2.1 | -0.5 | -3.7 | -1.9 | 2.7 | -2.3 | 8 | 2.4 |
| Karnataka | 4.6 | 5.7 | 5.6 | 8.4 | 14.4 | 3.7 | 5 | 12.9 | 9 | 21.7 | -3.7 |
| Kerala | -0.5 | -2.6 | 0.4 | -1.6 | -4.5 | -1.5 | -4.5 | -4.4 | -0.5 | -3.7 | 0.1 |
| Lakshadweep | -5.8 | -4.2 | -5.8 | -5.8 | -4.1 | -7.5 | -10 | -6 | -2.7 | -2.9 | 5.8 |
| Puducherry | -3.5 | 2.5 | -0.1 | 0.8 | -3.7 | -2 | -1.7 | -8.1 | 0.2 | -8.9 | 0 |
| Tamil Nadu | 2.7 | 4 | 5.1 | 7.8 | 10.4 | 1.7 | 3.4 | 9.2 | 10.7 | 19.7 | -1.9 |
| Telangana | -3.9 | -7.2 | -3.1 | -2.4 | 1.4 | -5.4 | -3.8 | 6.4 | 0.5 | 11.6 | 4.3 |
OPV (B), oral polio vaccine (birth); MR, measles rubella; FV, full vaccination; NV, no vaccination
A gradual rise in the percentage of vaccination among male (36.7-76.9%) and female children (34.1-76%) was found with a reduction in gap (2.6-0.9%) between males and females from NFHS-1 to NFHS-5 (Fig. 1). Similarly, the urban (50.7-75.5%) and rural (30.9-76.8%) population also presented with gradual rise in percentage of vaccination from NFHS-1 to NFHS-5 with a rise in rural vaccination (0.7%) in NFHS-5 as compared to previous rounds as presented in figure 2. As the birth order increased, the percentage of vaccination decreased proportionately from NFHS-1 to NFHS-5 (Fig. 3).
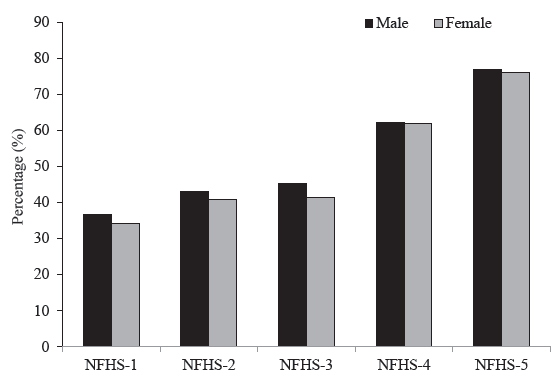
- Gender-wise change in fully vaccinated children in India between NFHS-1 to NFHS-5. NFHS, National Family Health Survey.
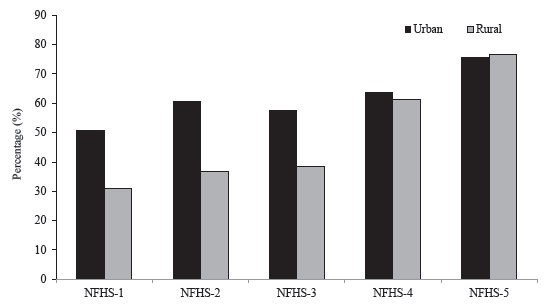
- Residence-wise change in fully vaccinated children in India between NFHS-1 to NFHS-5.
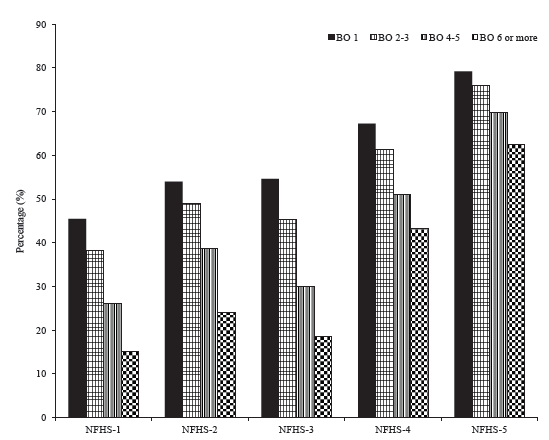
- Birth-order (BO) wise change in fully vaccinated children in India between NFHS-1 to NFHS-5.
Discussion
The current study analyzed State-wise and demography wise distribution of trends of immunization from NFHS-1 to NFHS-5. The study also assessed the State-wise distribution of vaccination gap in NFHS-5 and State-wise distribution of change in vaccination coverage between NFHS-4 and 5. The introduction of Expanded Programme on Immunization (EPI) in 1978 which was later renamed as Universal Immunization Programme (UIP) in 1985, expanded the UIP by introducing more vaccines such as hepatitis B and pneumococcal vaccine in 2007 and 2017. Furthermore, introducing new policies from time to time like mission Indradhanush to increase immunization coverage to make it more acceptable and effective for public is an evidence to the efforts done by the government of India to strengthen the immunization programme4,20,21.
In case of NFHS-5 the maximum gap was found to exist between BCG and hepatitis B vaccine (27.8%) which has to be given at birth. This gap was maximal in northeastern States like Manipur (47.3%) and Nagaland (44.7%). Similarly, the gap between birth dose of BCG and OPV was maximum in Manipur (32.8%) and Meghalaya (30.5%). The gap between the first and third dose of polio vaccine was 11.9 per cent followed by BCG and OPV zero dose (9.7%) at national level. The gap in vaccination was observed most in northeastern States as compared to other areas of India. This may be attributed to the fact that these are difficult terrain areas having tribal populations who may lack the access to health facilities and the knowledge regarding the importance of vaccination. As the risk of acquiring chronic hepatitis B virus infection is highest among the newborns and young children, addressing the vaccine coverage gap will be pivotal in reducing/elimination of chronic HBV cases.
Missed child vaccination in India contributes a lot to the preventable morbidity and mortality among children because of vaccine preventable diseases. An increase in the BCG, OPV, pentavalent, polio and MR coverage from NFHS-4 to NFHS-5 reflects the Government’s intention in achieving 100 per cent immunization coverage. From NFHS-4 and NFHS-5, the current study found an overall increase in ‘fully vaccinated’ coverage and decrease in the percentage of ‘non-vaccinated’. However, few States were found to have a downside in the vaccination coverage. The States of Telangana, Lakshadweep, Puducherry, Punjab, Goa, Sikkim were found to have decreased coverage of fully vaccinated children and increased prevalence of non-vaccinated children. These States were also found to have other decreased vaccination for other vaccine preventable disease.
An increase in the percentage of fully vaccinated children by 41.2 per cent and decrease in percentage of non-vaccinated children by 26.4 per cent was observed from NFHS-1 to NFHS-5. Overall, the northeastern States showed maximum improvement in percentage of fully vaccinated and non-vaccinated prevalence but still away from national percentages. The State-wise variation in immunization was evident in Lakshadweep, Telangana and Andhra Pradesh which had a maximum rise in the number of non-vaccinated children from NFHS-4 to NFHS-5. Few States which were found to have recorded less change in percentage of fully vaccinated and non-vaccinated children were already having comparatively higher percentages of these indicators. The hard to reach areas of northeastern States, low socio-economic status, and low education status of people may be attributed to slower immunization coverage22. The States of Arunachal Pradesh, Assam, Bihar, Meghalaya and West Bengal were found to be the only States where there was a uniform trend of increase in prevalence of fully vaccinated children and decline in prevalence of non-vaccinated children from NFHS-1 to NFHS-5. Past studies have shown that the distance from the health facility, availability of health care workers, and infrastructure of health centres are associated with the vaccine coverage23-27. The role of sociodemography is also important here as it has been revealed that maternal education, household wealth, child size at birth and maternal health services are significant predictors of a child’s full immunization. Other factors which have significant bearing on full vaccination coverage of children were maternal age, sex of head of the household, social category, religion and place of residence10.
A steady rise in percentage of immunized children was found over the period of time among both males and females with reduction of gap between males and females (2.6-0.9%) from NFHS-1 to NFHS-5. Various programmes focusing on gender equality in India and within States may be associated with improvement in immunization28. Awareness among people and increased literacy rate among people can also be attributed to increased immunization29-31.
The vaccination coverage has increased in both urban (50.7-75.5%) and rural (30.9-76.8%) population but the rise is higher in rural area than urban. The percentage rise in rural vaccination from NFHS 1 to 5 was 0.7 per cent. The various national health programme such as National Rural Health Mission (now renamed as National Health Mission) have targeted to cover the rural population, the increase is much higher there32. Despite these efforts, there remain some underserved pockets, especially the urban slums. Such pockets should be identified, and an intensified approach should target to cover all the children and to reduce drop outs.
As the birth order increased, the percentage of vaccination decreased proportionately. A study by Chowdhury et al33. found higher odds of vaccination in children whose birth order was <2. Mothers being the care givers of the children must be educated about the importance of vaccination. This will help increasing the vaccine coverage in India.
The improvement in the overall immunization status was quite evident from the existing data, however the goal of achieving 100 per cent immunization is still a far-fetched idea. In addition to the efforts put in by the government, the stakeholders need the same level of motivation regarding vaccination. Besides this, understanding the root causes of immunization inequalities in States will help policy makers and programme managers develop strategies to increase health service coverage and eliminate barriers for underserved populations.
The present study had some limitations. Firstly, as this was an analysis of aggregated data, there could be a role of ecological fallacy with respect to various factors such as gender, place of residence, birth order, etc. Hence, the results are to be read with caution as the data is sourced from published reports and not raw data. Detailed analysis from the raw data is required to be complemented with trend analysis to gain a better picture, ruling out differences and accounting for uncertainty estimates. Thirdly, the data from reports is cross-sectional in nature which implies no causal inference. Fourth, the change in age of respondents from households (married females/unmarried women) in different NFHS surveys may have mis-estimated the immunization coverage as the lower limit of age was 13 yr (NFHS-1) which increased to 15 yr subsequently (NFHS-2 onwards).
To achieve 100 per cent immunization coverage, each State has to improve their immunization coverage individually owing to differences in the socio-demographic and operational factors responsible for immunization. Strict guidelines should be put in place to overcome the difference in the vaccines given at the same time/visit which is of grave concern. Differences in the immunization coverage of different States needs in depth analysis at an individual level and at national level to overcome the barriers of immunization. The better performing States in terms of immunization coverage may act as a mentor for other States. Implementation of user-friendly information technology services can also boost the under-coverage of immunization.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Why vaccines matter: understanding the broader health, economic, and child development benefits of routine vaccination. Hum Vaccines Immunother. 2020;16:1900-4.
- [CrossRef] [Google Scholar]
- A brief history of vaccines & vaccination in India. Indian J Med Res. 2014;139:491-511.
- [PubMed] [PubMed Central] [Google Scholar]
- Eradicating poliomyelitis: India’s journey from hyperendemic to polio-free status. Indian J Med Res. 2013;137:881-94.
- [PubMed] [PubMed Central] [Google Scholar]
- Universal Immunization Programme (UIP). Available from: https://main.mohfw.gov.in/Major-Programmes/universal-immunization-programme-uip, accessed on August 7, 2023.
- Improving vaccination coverage in India: lessons from Intensified Mission Indradhanush, a cross-sectoral systems strengthening strategy. BMJ. 2018;363:k4782.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mission Indradhanush. Available from: https://www.nhp.gov.in/mission-indradhanush1_pg, accessed on April 9, 2023.
- Vaccination coverage and the factors influencing routine childhood vaccination uptake among communities experiencing disadvantage in Vellore, southern India: a mixed-methods study. BMC Public Health. 2021;21:1807.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mother and child protection card as a resource tool for health care providers on VHND sessions: Providers’ views in rural area of Valsad district in south Gujarat, India. J Fam Med Prim Care. 2022;11:3104-8.
- [Google Scholar]
- Electronic Vaccine Intelligence Network (eVIN). Available from: https://www.nhp.gov.in/electronic-vaccine-intelligence-network(evin)_pg, accessed on April 9, 2023.
- Explaining socioeconomic inequalities in immunisation coverage in India: new insights from the fourth National Family Health Survey (2015-16) BMC Pediatr. 2020;20:295.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Vaccination inequality in India, 2002-2013. Am J Prev Med. 2021;60:S65-76.
- [CrossRef] [PubMed] [Google Scholar]
- Measles elimination in India—shifting goal post. Indian J Pediatr. 2023;90:420.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Vaccine hesitancy as a challenge or vaccine confidence as an opportunity for childhood immunisation in India. Infect Dis Ther. 2020;9:421-32.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- National family health survey (NFHS-1), 1992-1993. India. Available from: https://dhsprogram.com/pubs/pdf/SR162/SR162.pdf, accessed on March 7, 2024.
- National family health survey (NFHS-2), 1998-1999. India. Available from: https://www.dhsprogram.com/pubs/pdf/FRIND2/FRIND2.pdf, accessed on March 7, 2024.
- National family health survey (NFHS-3), 2005-2006. Available from: https://dhsprogram.com/pubs/pdf/frind3/frind3-vol1andvol2.pdf, accessed on March 7, 2024.
- National family health survey (NFHS-4), 2015-2016. Available from: https://dhsprogram.com/pubs/pdf/fr339/fr339.pdf, accessed on March 7, 2024.
- National family health survey (NFHS-5), 2019-2021. Available from: https://www.iipsindia.ac.in/content/nfhs-project, accessed on March 7, 2024.
- Goal 3: Targets and Indicators. Available from: https://sdgs.un.org/goals/goal3#targets_and_indicators, accessed on October 22, 2024.
- National Operational Guidelines-Introduction of Pneumococcal Conjugate Vaccine (PCV). Available from: https://mohfw.gov.in/sites/default/files/PCV_Operational%20Guidelines_Jan%20%202021.pdf, accessed on March 7, 2024.
- Mission Indradhanush Operational Guidelines 2016. Available from: https://mohfw.gov.in/sites/default/files/ 216846291201489665182.pdf, accessed on March 7, 2024.
- Explaining socioeconomic inequalities in immunisation coverage in India: New insights from the fourth National Family Health Survey (2015-16) BMC Pediatr. 2020;20:1-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Determinants of childhood immunisation coverage in urban poor settlements of Delhi, India: A cross-sectional study. BMJ Open. 2016;6:1-12.
- [CrossRef] [Google Scholar]
- Influence of socio-demographic factors on coverage of full vaccination among children aged 12-23 months: a study in Indian context (2015-2016) Hum Vaccin Immunother. 2021;17:5226-34.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Migration and child health: Understanding the coverage of child immunization among migrants across different socio-economic groups in India. Child Youth Serv Rev. 2020;119:105684.
- [CrossRef] [Google Scholar]
- Vaccination coverage and the factors influencing routine childhood vaccination uptake among communities experiencing disadvantage in Vellore, southern India: a mixed-methods study. BMC Public Health. 2021;21:1807.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Public health facility quality and child immunization outcomes in rural India: A decomposition analysis. Vaccine. 2022;40:2388-98.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Initiatives by Government for reducing gender gap in all aspects of social, economic and political life. Available from: https://pib.gov.in/PressReleasePage.aspx?PRID=1707475, accessed on March 7, 2024.
- The association of health literacy with intention to vaccinate and vaccination status: A systematic review. Vaccines. 2022;10:1832.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association between maternal health literacy and child vaccination in India: A cross-sectional study. J Epidemiol Community Health. 2015;69:849-57.
- [PubMed] [Google Scholar]
- Determinants of immunization coverage in Lucknow district. North Am J Med Sci. 2015;7:36.
- [CrossRef] [Google Scholar]
- National Health Mission. Available from: https://nhm.gov.in/index1.php?lang=1&level =1&sublinkid=969&lid=49, accessed on July 31, 2024.
- Universal health coverage - There is more to it than meets the eye. J Fam Med Prim Care. 2017;6:169-70.
- [Google Scholar]






