Translate this page into:
Infrared thermography: An investigative tool for detection of subclinical bleed in hemophilia on prophylaxis
For correspondence: Dr Maitreyee Bhattacharyya, Institute of Haematology and Transfusion Medicine, Kolkata 700 073, West Bengal, India e-mail: mbhattyacharyya@yahoo.co.in
-
Received: ,
Accepted: ,
Abstract
Background & objectives
Subclinical joint bleed is a matter of concern in individuals with hemophilia on prophylaxis. Ultrasonography (USG) is mostly used for the screening of subclinical bleeds in such individuals but it has its own limitations. Thus a more comprehensive technology is required for the detection of the same. This study undertook to evaluate the efficacy of infrared thermography (IRT) for detection of subclinical joint bleeds and its comparison with ultrasonography and MRI (Magnetic Resonance Imaging), considering MRI as the gold standard.
Methods
Forty eight asymptomatic individuals with hemophiliacs on prophylaxis and 15 healthy males as controls were recruited. IRT, USG and MRI were done in all participants included in the study. FLIR camera systems were used for the capture of thermograms of the joints in both the study groups.
Results
The mean of maximum temperature difference>0.5K (ΔT max >0.5K) as compared to a healthy joint was considered as significant. Subclinical bleeds were detected in 23.9, 7.29 and 27.08 per cent participants by IRT, USG and MRI respectively. Sensitivity and specificity of IRT and USG was detected to be 88.4 and 97.67 per cent, and 26.9 and 99 per cent, respectively.
Interpretation & conclusions
The findings of this study suggest that IRT is an effective tool for detection of subclinical joint bleeds in individuals with hemophilia and can be used for the monitoring of the joints in such individuals.
Keywords
Hemophilia
infrared thermography
MRI
prophylaxis
subclinical bleed
ultrasonography
Hemophilia is an X-linked disorder which occurs due to factor VIII or IX deficiency1 Recurrent bleeding in the joints is a major concern leading to hemophilic arthropathy and ultimate disability2 Hemophilia prophylaxis comprises administration of factors VIII or IX in small doses at regular intervals to convert a severe hemophilia to moderate hemophilia and avoid spontaneous bleeding3. The main aim of hemophilia prophylaxis is to alter the course of the disease by maintaining natural homeostasis and reducing the number of joint bleeds4. In many individuals on prophylaxis, the annual bleeding rates (ABR) gradually decrease, thereby preventing major deformities in the joint5. As a convention, efficacy of prophylaxis is judged by the annual bleeding rate which is solely based on clinical assessment. However, there may be subclinical bleedings which remain undetected and ultimately lead to joint damage.
Musculoskeletal imaging is used nowadays for detection of subclinical bleeding in persons with hemophilia (PwH) on prophylaxis. Ultrasound is the most commonly used modality for this purpose6. Infrared thermal imaging (IRTI) is a simple non-invasive tool in which heat distribution index is calculated and further mapped into thermal images. Like ultrasonography (USG) and Magnetic resonance imaging (MRI), Infrared Thermography (IRT) may also be applicable for musculoskeletal abnormality. Over three decades, IRTI with advance machine learning technology was developed for the early detection of breast cancer7-10. Lasenen et al11 established the ability of IRT to detect inflammation of joints in juvenile rheumatoid arthritis cases which further improved the treatment and patient care11. Later, this technology was extrapolated for the detection of muscular sport injuries by Siliero Quitianna et al12. As muscular injuries trigger inflammatory processes causing hyperthermia, these could be detected by IRT. This information helped doctors to detect sports injuries faster13.
Individuals with hemophilia suffer from inflammation as a result of joint bleeds. Bleeding in the joints causes inflammation and significant rise in temperature (>0.5K) in the joints13 which could be easily detected by IRT. According to Selfe et al14, it was observed that skin temperature asymmetry >0.5K is not normal and indicates abnormal physiology. So far, there are only two studies on the IRT imaging-based detection of musculoskeletal abnormality in hemophilia cases15,16. Of these one study was undertaken on hemophilia children on prophylaxis. Here, silent joints or asymptomatic bleed was determined by IRT and compared with clinical examination score15. In the present study, we aimed to detect subclinical joint bleeding by IRT in asymptomatic individuals with hemophilia on prophylaxis and to assess its efficacy with MRI as the gold standard17. So far as our knowledge goes, this is the first study on efficacy of IRT on detection of subclinical bleeds in individuals with hemophilia on prophylaxis.
Material & Methods
The study was conducted between September 2022 to February 2023 at the Institute of Haematology and Transfusion Medicine, Medical College and Hospital, Kolkata. The study was conducted according to Helsinki declaration and duly approved by the Institutional Ethics Committee. Informed consent was taken from each participant/parents prior to the recruitment.
Study population
The study included both individuals with Hemophilia A and B receiving prophylaxis from the institute and age-matched healthy males with no history of joint injury or pain were recruited as control. The age range was 3-34 yr for both the groups. Individuals without any prior joint diseases, arthropathy, arthritis in any form were included as controls. These individuals with Hemophilia were suspected of having subclinical bleed in the joints.
Study protocol
Detailed clinical history was taken from each patient/parents, annual bleeding rate (ABR) was noted from patient’s records, thorough examination was done and joint score was calculated by using Hemophilia Joint Health Score (HJHS). All the study participants were on prophylaxis with intermediate dose of 20 IU/kg body weight twice weekly dose as per the departmental protocol. IRT imaging of bilateral knee, ankle and elbow joints were done for all participants under patient and control groups. USG and MRI of the same joints were done from the department of Radiodiagnosis, Medical College Kolkata for each participant on the same day.
Magnetic resonance imaging
A 3-Tesla MRI scanner (Siemens MagnetomVerio TIM 3T MRI scanner) was used to assess the bleeding in respective joints. It was a non-contrast MRI. The International Prophylaxis Study Group (IPSG) MRI scale was used for detection of the bleeding17.
Ultrasonography
Ultrasonography assessment was done using Hemophilia Early Arthropathy Detection with Ultrasound (HEAD-US) protocol18. MRI was done by the technician and reported by the radiologist, while USG was done by the radiologist. Both the imaging was done on the same day, and the method was blinded19-22. Later, correlation with USG and MRI was done.
Infrared thermography
An infrared thermal camera (FLIR SC 305, FLIR Systems, AB, Sweden) was used to capture thermal images of the study participants of both the patient and control groups. FLIR camera has a thermal sensitivity of less than 0.05°C at +30°C; spectral sensitivity ranging from 7.5-13 µm and geometric resolution of 1.36 mrad (320x240 pixels focal plane array and field of view 25x18.8 and minimum focus distance of 40 cm); image resolution is nine frames per second. Participants were acclimated with the prevailing room temperature for 10 minutes prior to capture of images and video recording23.
Infrared thermography (IRT) of the study participants (both hemophilia and healthy group) was done following the protocol as described by Sueser et al15. IRT imaging of both hemophilia and control group was done in a closed dark room under ambient temperature. The room temperature was controlled at 298 K (25°C) and humidity was maintained at 45±5 per cent. The distance between the camera and participant was 90 cm for close view and 200 cm for distance imaging. Participants were advised not to involve in any hard physical activity two days prior to IRT. Thermographic images of the three bilateral joints knee, elbow, ankle were obtained for the controls and patients. The region of interest (ROI) was marked, heat distribution index (HDI) was calculated and maximum temperature of ROI is obtained. Mean T-max of each joint was compared between the hemophilia and healthy groups.
Statistical analysis
IR thermograms were analyzed using the FLIR software programme ( https://www.flir.in/browse/rampd-and-science/rampd-software/). Thermograms data was analyzed in MS excel and Graphpad Prism free software was used ( https://www.graphpad.com/features) for the calculation of probability and other statistically relevant indices like sensitivity and specificity. MATLAB programme (https://in.mathworks.com/products/matlab/programming-with-matlab.html) was used for the computation of Receiver Operating Characteristic (ROC) curve.
Results
The study population consisted of 48 asymptomatic individuals with hemophilia on prophylaxis. Fifteen healthy males of similar age groups were included as controls. Forty six (95.8%) were hemophilia A and two (4.2%) were hemophilia B. The age range was 3 - 34 yr. The mean age was 10.96 yr. Out of 48,45 (93.75%) were severe hemophilia and 3 had (6.5%) moderate hemophilia. The three moderate hemophilia patients received prophylaxis as two of them had evidence of intracranial bleed and one severe psoas haematoma. All of them received intermediate dose of prophylaxis at 20 U/Kg thrice weekly for hemophilia A and 30 U/Kg twice weekly for hemophilia B as per the hospital protocol. The duration of prophylaxis ranged from 14 months to seven yr. The mean duration of prophylaxis was 35.5 months. Out of the study population, 6 (12.5%) received primary prophylaxis, 36 (75%) received secondary prophylaxis and another 6 (12.5%) tertiary prophylaxis. The most commonly involved joint was the left knee (43.75%). Single joint involvement was found in majority 33 (68.75%) of the patients, 6 (12.5%) patients had two joints involvement whereas more than two joints were involved in 9 (18.75%) participants. The ABR ranged from 1-4. The mean ABR was 1.3. The joint scores were calculated for each joint with the hemophilia joint health scoring system (HJHS)24. The score ranged from 0-6. The mean HJHS score was 0.56. The details of the clinical characteristics are given in Supplementary Table. Thermographic images (Thermogram) for the different joints (knee, elbow, ankle) were captured for both the hemophilia as well as the control group (Fig. 1). The mean T-max of the knee joint of the hemophila group was significantly high as compared to that of controls. The participant shown in Figure 1A had haemorrhage in both of his knee joints with right knee more affected than the left, however, he was asymptomatic at the time testing.
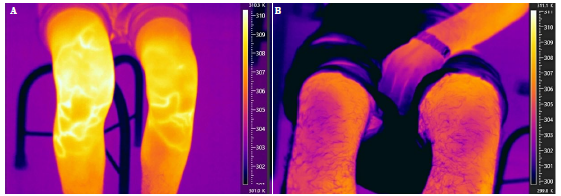
- Infrared thermograph image of a participant with (A) hemophilia and (B) healthy control. Temperature scale is shown on the right side in each panel.
IR thermogram of bilateral knee, ankle and elbow joints of each control subject was done and temperature recorded. Mean of maximum recorded temperatures of each joint was taken as standard normal temperature of that joint. This was 306.28 and 306.17 for right and left knee joints, respectively. Mean elbow temperature was slightly higher 306.53 for right and 306.43 for left elbow joint. For ankle joint standard temperature was 306.48 for right and 306.4 for left ankle (Fig. 1B).
Comparison of IR-thermogram
All three joints (knee, ankle and elbow) of the 48 hemophilia group were screened by IRT. Mean temperature of this group for each of these joints were significantly higher (P<0.05) than the control group at the susceptible bleeding points (Fig. 2). Temperature difference of >0.5 K above average of the recorded temperature (T max) of the hemophilia group for that particular joint was considered significant as bleeding joints13.
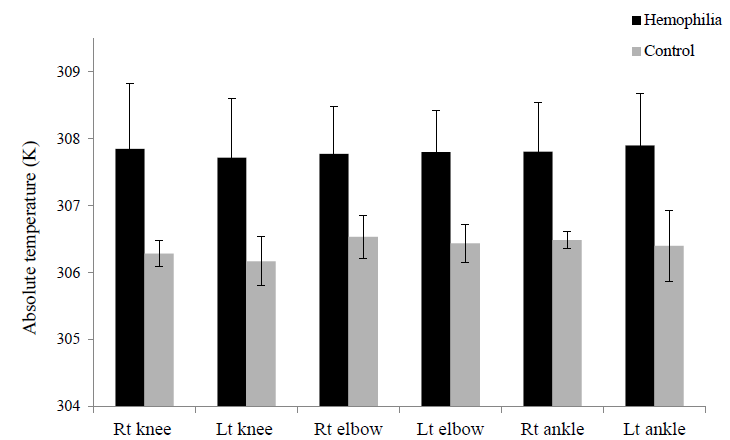
- Baseline comparison of avg. Tmax between haemophila affected individuals and controls. The bar-graph compares the avg. Tmax. for the bilateral joints in both the groups. Joints in haemophila affected individuals show significantly (P<0.05) high temperature in all the three types of joints as compared to controls. Rt, right; Lt, left.
IRT findings in the hemophilia group
In the hemophila group, temperature differences (ΔT max) ≥0.5 K were found in 69 (23.9%) affected joints. Temperature differences of >0.5 K above the average T-max of the joint in the hemophilia group was considered clinically significant. Joints with temperature difference <0.5 K were considered as in a quiescent state, hence 76.05 per cent of the joints were found to be at quiescent state in the haemophila group
USG and MRI findings
Ultrasonography of the participants showed that among the 288 joints screened; 21 (7.29%) had subclinical bleeding (Fig. 3). USG failed to detect bleed in 16.61 per cent joints; however, 2.08 per cent of joint bleed detected by USG were missed by IRT. MRI of the hemophilia group showed that among the 288 joints screened; 78 (27.08%) had subclinical bleeding and 199 (69.09%) joints were found to be normal. Results of IRT, USG and MRI were depicted in a composite bar-graph (Fig. 3).
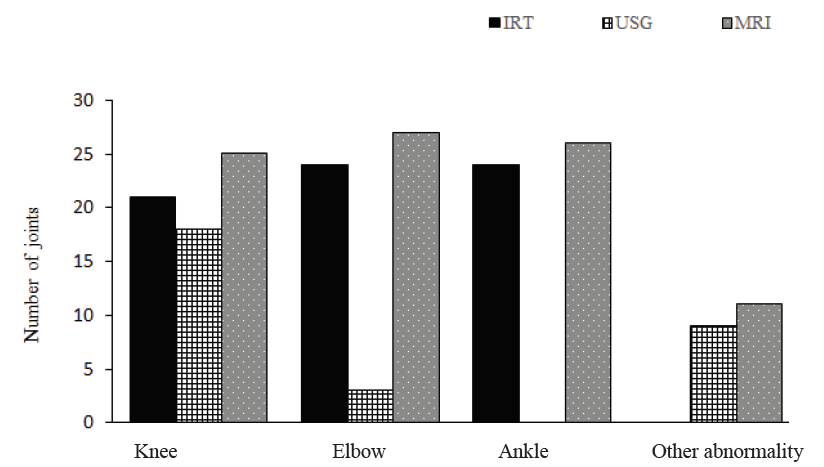
- Joint bleeding detected by IRT, USG and MRI. Results of IRT, USG and MRI is shown as composite bar-diagram. IRT of 69 joints had ΔTmax >0.5K, USG detected bleeding in 21 joints whereas MRI detected 78 joints with bleeding in total 288 joints screened. IRT, infrared thermography; USG, ultrasonography; MRI, magnetic resonance imaging.
Comparison of IR-thermogram with USG and MRI findings
Correlation of the thermographic findings with the USG of the joints for the particular individuals with hemophilia were done (Fig. 4). USG detected bleeding in knee joint and left elbow joint but failed to detect bleeding in ankle joints and right elbow joints. Comparison of thermographic findings with MRI was done. The results are shown in Figure 4. MRI could detect bleeding in 78 cases, whereas IRT could detect in 69 cases.
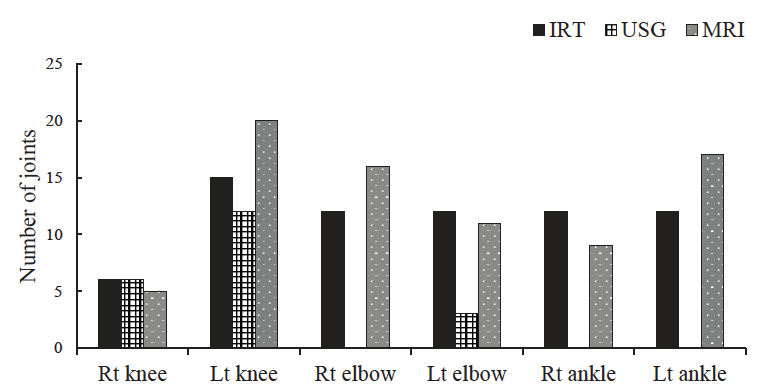
- Comparison of IRT with USG and MRI findings. Results of three modalities were compared and depicted as composite bar-diagram. Results of all the three bilateral joints investigated by IRT, USG and MRI were compared. USG failed to detect bleeding in right elbow and ankle joints. No., number.
Discussion
Prophylaxis in hemophilia has been shown to be effective both in children and adolescents. It also decreases the ABR25,26. Although prophylaxis reduces bleeding significantly, it does not eliminate bleeding events in all patients25. Often there is asymptomatic bleeding, which needs to be picked up for evaluation of prophylaxis protocol, and necessary modifications need to be done.
The presence of subclinical bleeding is difficult to study and quantify. However, its presence is usually supported by the observation that joint damage was seen on MRI despite a lack of clinically evident bleeding27. Clinical evaluation with the help of HJHS score of all the patients in the present study was done (average score) but could not be differentiated from that of control group as was found in previous studies21,28,29.
USG has been used as an established modality in detection of subclinical bleeds in hemophilia. Hortensia et al30 detected in their series, that 14 per cent of the study participants exhibited HEAD-US signs of incipient arthropathy in joints with no history of bleeding2. In spite of adequate prophylaxis, there is possibility of withdrawal bleeding2. A previous study from our institute detected subclinical bleeding in 11.1 per cent cases of hemophilia6. But the issue with USG is that only one joint can be screened at a time and there is a lot of subjective variability. Sensitivity of USG in detecting subclinical bleeds in this study was found to be 26.9 per cent but specificity of 99 per cent with respect to MRI. Doria et al28 too reported variable sensitivity of USG (sensitivity range of 12-100% for knees and 86-100% for ankles) in evaluating joint damage.
A comprehensive review of the studies on the utility of IRT in different pathological conditions has shown that hyperthermia correlates with inflammation or bleeding points31. In the present study, IRT were assessed on asymptomatic hemophilia patients and compared with the control group. There was a significant difference in T-max (P<0.05) in the hemophiliacs at joints of susceptible bleeds.
Seuser et al13 studied the musculoskeletal differences in hemophilia children using IRT in a case control study. They detected early inflammation depending on temperature difference between the two sides of the same joint (such as left knee and right knee) taking clinical examination as reference, and found a significantly high number of affected joints in hemophiliacs as compared to healthy boys and reported sensitivity of 84 per cent and specificity of 73 per cent, but only 33 per cent of positive predictive value. In this study, IRT was found to have a high sensitivity (88.4%), specificity (97.67%), positive predictive value (PPV) (93.2%), and negative predictive value (NPV) (97.67%) taking MRI data of joints as standard. ROC curve further validates the efficacy of the IRT method (Fig. 5). Similar findings were reported by Xuan et al32. that detected arthrorrhagia in hemophilia patients using IRT and found high sensitivity (89.3%) and specificity (84.3%) of IRT16. Both USG and IRT findings of the joints were compared with MRI (gold standard) which showed high sensitivity and specificity of IRT. Though we considered knee, ankle and elbow joints only, many other joints showed a rise in temperature. This suggests that IRT can be used for screening of all joints simultaneously which is not possible with USG. However, screening all the joints by USG is time-consuming and costly. IRT setup is less sophisticated and requires minimal training. Hence, IRT may serve as an important reliable point-of-care tool for early detection of subclinical bleeds. It is an easy, low cost modality, point of care testing which can be used for early interpretation of inflammatory changes. The success of prophylactic treatment may also be assessed by this test by serial monitoring of joint bleeds. In a resource poor country like India, factor availability is a major concern. Hence economic and optimum use of factors is necessary. However, this needs further validation with a large study population.
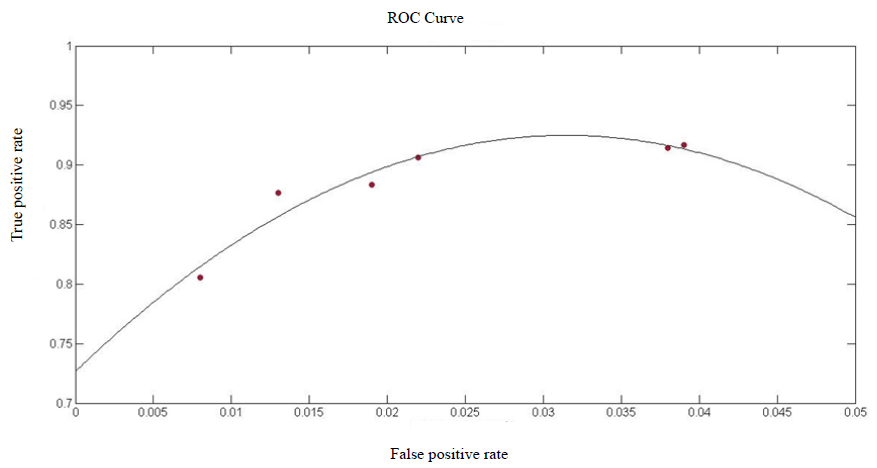
- Receiver operating characteristic (ROC) curve. The ROC graph shows the correlation between the TPR (true positive rate) and FPR (false positive rate) of the IRT data with reference to MRI data. Curve fitting was done in MATLAB programme.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Asymptomatic joint bleeding and joint health in hemophilia: a review of variables, methods, and biomarkers. J Blood Med. 2021;1:209-20.
- [Google Scholar]
- Factor VIII/factor IX prophylaxis for severe hemophilia. Semin Hematol. 2016;53:3-9.
- [Google Scholar]
- Blanchette vs. prophylaxis in the hemophilia population. Hemophilia. 2010;16:181-8.
- [Google Scholar]
- Prophylaxis usage, bleeding rates, and joint outcomes of hemophilia, 1999 to 2010: a surveillance project. Blood. 2017;129:2368-74.
- [Google Scholar]
- Ultrasonography of knee joint in hemophilia A: What the eyes cannot see. Indian J Hematol Blood Transfus. 2019;35:149-54.
- [Google Scholar]
- Effectiveness of a noninvasive digital infrared thermal imaging system in the detection of breast cancer. Am J Surg. 2008;196:523-6.
- [Google Scholar]
- Breast cancer detection using infrared thermal imaging and a deep learning model. Sensors. 2018;18:2799.
- [Google Scholar]
- A hybrid methodology for breast screening and cancer diagnosis using thermography. Comput Biol Med. 2021;135:104553.
- [Google Scholar]
- Thermal imaging in screening of joint inflammation and rheumatoid arthritis in children. Physiol Meas. 2015;36:273.
- [Google Scholar]
- Infrared thermography as a means of monitoring and preventing sports injuries. In: Research anthology on business strategies, health factors, and ethical implications in sports and eSports. Pennsylvania, United States: IGI Global; 2021. p. :832-65.
- [Google Scholar]
- Orthopaedic issues in sports for persons with hemophilia. Hemophilia. 2007;13:47-52.
- [Google Scholar]
- A narrative literature review identifying the minimum clinically important difference for skin temperature asymmetry at the knee. Thermol Int. 2008;18:41-4.
- [Google Scholar]
- Infrared thermography as a non-invasive tool to explore differences in the musculoskeletal system of children with hemophilia compared to an age-matched healthy group. Sensors. 2018;18:518.
- [Google Scholar]
- Infrared thermal imaging maybe an available tool to detect arthrorrhagia in patients with hemophilia. Blood. 2017;130:4887.
- [Google Scholar]
- WFH guidelines for the management of Hemophilia, 3rd edition. Hemophilia. 2020;26:1-158.
- [Google Scholar]
- An MRI scale for assessment of haemophilic arthropathy from the International Prophylaxis Study Group. Hemophilia. 2012;18:962-70.
- [Google Scholar]
- Magnetic resonance imaging evidence for subclinical joint bleeding in a Dutch population of people with severe hemophilia on prophylaxis. J Thromb Haemost. 2023;21:1156-63.
- [Google Scholar]
- Patient-reported outcomes and joint status across subgroups of US adults with hemophilia with varying characteristics: Results from the Pain, Functional Impairment, and Quality of Life (P-FiQ) study. Eur J Hematol. 2018;100:14-24.
- [Google Scholar]
- Evaluating outcome of prophylaxis in hemophilia: objective and self-reported instruments should be combined. Hemophilia. 2016;22:e80-6.
- [Google Scholar]
- HJHS 2.1 and HEAD-US assessment in the hemophilic joints: How do their findings compare? Blood Coagul Fibrinolysis. 2020;31:387-92.
- [Google Scholar]
- Thermal fluctuation based study of aqueous deficient dry eyes by non-invasive thermal imaging. Exp Eye Res. 2014;120:97-102.
- [Google Scholar]
- WFH Guidelines for the management of hemophilia. In: Haemophilia Vol 27. (3rd edition). 2021. p. :699.
- [Google Scholar]
- Prophylaxis versus episodic treatment to prevent joint disease in boys with severe hemophilia. N Engl J Med. 2007;357:535-44.
- [Google Scholar]
- Should prophylaxis be used in adolescent and adult patients with severe hemophilia? An European survey of practice and outcome data. Hemophilia. 2007;13:473-9.
- [Google Scholar]
- Diagnostic accuracy of ultrasound for assessment of hemophilic arthropathy: MRI correlation. AJR Am J Roentgenol. 2015;204:W336-47.
- [Google Scholar]
- Validation of a new pediatric joint scoring system from the International Hemophilia Prophylaxis Study Group: validity of the hemophilia joint health score. Arthritis Care Res. 2011;63:223-30.
- [Google Scholar]
- The value of HEAD-US system in detecting subclinical abnormalities in joints of patients with hemophilia. Expert Rev Hematol. 2018;11:253-61.
- [Google Scholar]
- Applications of thermal imaging with infrared thermography in orthopaedics. J Clin Orthop Trauma. 2022;24:101722.
- [Google Scholar]
- Infrared thermal imaging maybe an available tool to detect arthrorrhagia in patients with hemophilia. Blood 2017:4887.
- [Google Scholar]






