Translate this page into:
Factors influencing delayed cancer health seeking in Meghalaya, Northeast India: A qualitative study
For correspondence: Dr Melari Shisha Nongrum, Indian Institute for Public Health Shillong 793 001, Meghalaya, India e-mail: melari.nongrum@iiphs.ac.in
-
Received: ,
Accepted: ,
Abstract
Background & objectives
India accounts for about seven per cent of the global cancer burden with the highest cancer incidence reported from the North-Eastern Region (NER), including Meghalaya. Despite this, there is paucity of published studies on health seeking behaviour for cancer in the NER. To address this gap, this study used a qualitative approach to document patient, caregiver and provider perspectives to understand the factors influencing healthcare seeking for cancers in Meghalaya.
Methods
In-depth interviews were undertaken with 37 individuals diagnosed with one of the top five cancers in Meghalaya, namely, oesophageal, breast, oral, cervical and lung cancer. They were identified from the State referral cancer hospital. Twelve caregivers and five healthcare providers were also interviewed. All interviews were conducted in the local language using semi-structured interview guides. Transcripts were translated to English, coded, categorized and analyzed using thematic framework content analysis approach.
Results
A key factor influencing delayed cancer treatment in Meghalaya included misconceptions regarding the causes of cancer and cultural concepts such as bih and skai (Khasi language), i.e. notions of a figurative ‘poison’ or ill intent that makes one susceptible to illness. A general reluctance to discuss cancer diagnoses, perceived stigma, apprehension of treatment methods influenced their decision. Other factors included negligence and misinterpretation of early symptoms of cancer, self-management, preference for traditional medicines, financial constraints and health system-related factors.
Interpretation & conclusions
This study underscores the importance of addressing barriers to cancer diagnosis and treatment in indigenous populations in northeast India, advocating for culturally appropriate messaging, capacity building for healthcare workers, integration of traditional healers, and community involvement to enhance early healthcare seeking and improve outcomes.
Keywords
Cancer health-seeking behaviour
cultural concepts
indigenous world views
northeast India
stigma
traditional medicine
Cancer is a globally leading cause of death, accounting for around 10 million deaths in 20201. By 2040 the cancer cases are projected to increase by 47 per cent (an estimated 28.4 million cancer cases)2. The estimated incident number of cancer cases in India for the year 2022 was 14,61,427 with one in nine people with the likelihood of developing cancer in his/her lifetime3.
The States in the North Eastern Region (NER) of India have the highest cancer incidence and are predominantly inhabited by tribal communities, each with unique socio-cultural, behavioural and lifestyle factors4. NER’s cancer profile includes high incidence of cancers of the upper digestive tract such as stomach, oesophagus, and hypopharynx5. There is high consumption of tobacco, alcohol, betelnut and other food products such as chilli peppers, smoked meat and fish in the NER, which are known risk factors for cancers5,6. This is further exacerbated by the low levels of cancer screening7. Moreover, studies have reported low awareness regarding the signs, symptoms and risk-factors of cancers in the NER8, as well as lower adoption of methods for early cancer detection, such as self-breast examination9, potentially contributing to delays in diagnosis and poor survival.
The tribal population’s perspectives of health and disease (owing to their varied beliefs) may also play an important role in the health seeking behaviour of individuals affected with cancer in the NER. Earlier studies conducted to understand the cancer screening uptake in other parts of India reported poor knowledge, economic constraints, distance to the health centre, fear of diagnosis and lack of support from husband as the commonest barriers10. However, there is a paucity of published studies on health seeking behaviour for cancer in the NER. Hence, this qualitative study was conducted to investigate the barriers for healthcare seeking in cancer from patients, caregivers and healthcare providers (HCP).
Methods
Study setting
This qualitative study was conducted among the individuals affected with cancer seeking treatment at the Civil Hospital Shillong, the primary State run referral hospital for cancer care in Meghalaya, their caregivers and cancer HCP. Being the main referral hospital, Civil Hospital Shillong serves affected individuals from multiple districts both urban and rural areas, and from different tribes and socio-economic backgrounds. Between 2017 and 2022, the Oncology Department of this hospital treated a total of 22,007 patients (15,233 in-patients and 6,774 out-patients). The study was undertaken between July and October 2021 after obtaining clearance from Institutional Ethics Committee of the Indian Institute of Public Health Shillong. All participants provided informed consent after having understood the aim of the study and their rights as participants as outlined in the participant information sheet.
Meghalaya a predominantly tribal State in the NER of India, with the Khasi (Khynriam, Pnar, Bhoi War, Maram, Lyngngam sub groups within Khasi tribe) and Garo tribes comprising of 86 per cent of its 3.27 million population11. It is characterized by its hilly terrain, and is prone to natural disasters like heavy rainfall and earthquakes throughout the year. Limited facilities for cancer care in the region, coupled with the difficult terrain, often poses a major barrier to access appropriate health care in this region12. Cancer is among the top five leading causes of death in Meghalaya. Infact, cancer of the oesophagus is the leading site of cancer in both genders, followed by cancer of hypopharynx in males and oral cancer in females13.
Study design and data collection
The study adopted a qualitative descriptive methodology, grounded in the general principles of naturalistic inquiry aimed at fully describing the participants’ experiences without extensive theorization or abstraction. The entire research process was conducted following consolidated criteria for reporting qualitative research (COREQ). Purposive sampling technique was used to select the participants, so that the top five cancers in Meghalaya, namely oesophageal, breast, oral, cervical and lung cancer, were represented. Individuals with cancer, who were seeking treatment in the Shillong Civil Hospital during the study period, were included in this study. Selection of participants was conducted with the assistance of the lead oncologist of the hospital and also through snowball sampling of patients in the wider community. Additionally, caregivers who were family members of those patients and had knowledge of the illness and treatment seeking behaviour of the patients were included to document the caregiver-perspectives. To understand the HCPs’ perspectives on the factors responsible for delayed cancer health seeking behaviour, oncologists and nurses from the Radiation Oncology department of the hospital were also included in the study.
Face-to-face in depth interviews (IDIs) were conducted with all participants between July and October, 2021, were undertaken by a team of three bilingual indigenous female researcher officers. These researchers possessed prior experience in collecting and analyzing qualitative data and were fluent in both Khasi (local language) and English. Two of the researchers were public health postgraduates and one researcher was a social work postgraduate. Before data collection, the interviewers underwent comprehensive training on the research purpose, objectives, and ethical considerations. They also participated in refresher training sessions focused on qualitative research methods and research ethics. The researchers had no pre-existing relationships with the participants before the commencement of the study.
In-depth interviews
There were 54 IDIs conducted, of which, 30 patients and six caregivers were interviewed at the hospital outpatient department (OPD), and seven patients and six caregivers interviewed at their homes. The IDIs with the five HCPs were conducted at the Radiation Oncology department. Each interview lasted for about 35 to 40 min. Not formal sample-size calculation was conducted; recruitment of participants continued till data saturation was achieved.
The interviewers used a topic guide, which was iteratively adapted for patients, caregivers and healthcare providers. The probes in the interview topic guide for patients and caregivers included the experience of patients during the onset of symptoms, health seeking behaviour, their pathway to health seeking, and reasons influencing their health seeking decision. For HCPs, the interview topic guide was adapted to document the provider perspectives on treatment and health seeking behaviour of cancer patients, the reasons they believed there was any delayed access to healthcare, and the challenges faced by the healthcare professionals in providing cancer care. The interviewers made field notes, and also made audio-recordings of all IDIs.
Data analysis
Data were analyzed using a thematic content analysis approach. The recordings were first transcribed in Khasi and, thereafter, translated to English. Khasi language experts were consulted when faced with words and phrases that were not easily translatable into English. Inductive analysis was adopted during the coding process. The transcripts were read many times by investigators independently and the emerging themes and sub-themes were identified and coded. The results were compared and any disagreements in context to the interview were identified and resolved following discussion within the team. In the event that the researchers could not arrive at a concensus, discussion with supervisor was conducted. A codebook was developed in Microsoft Excel workbook (version 16.6), using a framework matrix. NVivo-12 software was also used to organize and analyze the data.
Results
Demographic profile of participants
A total of 37 cancer patients were interviewed, representing five out of the 12 districts in Meghalaya: East Khasi Hills, West Khasi Hills, East Jaiñtia Hills, West Jaiñtia Hills and Ri Bhoi. Demographic characteristics of the 37 respondents interviewed are shown in Table. There were also 12 caregivers who participated in the study, all, but one, were female. The mean (SD) age of the caregivers was 43.3 (15.8) yr. The HCPs included two male and one female oncologist and two female nurses.
| Male (n=17) | Female (n=20) | Total | |
|---|---|---|---|
| Age in yr; mean (±SD) | 56.2 (±10.2) | 51 (±10.3) | |
| Types of cancer | |||
| Oesophageal | 8 | 1 | 9 |
| Oral | 4 | 3 | 7 |
| Lung | 5 | 1 | 6 |
| Breast | 0 | 8 | 8 |
| Cervical | NA | 7 | 7 |
| Disease stage known | 5 | 9 | 14 |
| Stage I and II | 4 | 2 | 6 |
| Stage III and IV | 1 | 7 | 8 |
| Time to diagnosis known | 10 | 12 | 22 |
| >3 months | 5 | 9 | 14 |
| <3 months | 5 | 3 | 8 |
| First point of consultation | 17 | 20 | |
| Western medicine | 10 | 17 | 27 |
| Traditional medicine | 7 | 3 | 10 |
SD, standard deviation
Factors affecting health seeking behaviour for cancer
The findings from the three participant groups on factors contributing to the delay in seeking cancer health are presented under nine themes (Figure), which are described below. An anonymized unique identifier of each participant where ‘P’stands for cancer patient, ‘CG’ for caregiver and ‘HCP’for health care providers was given.
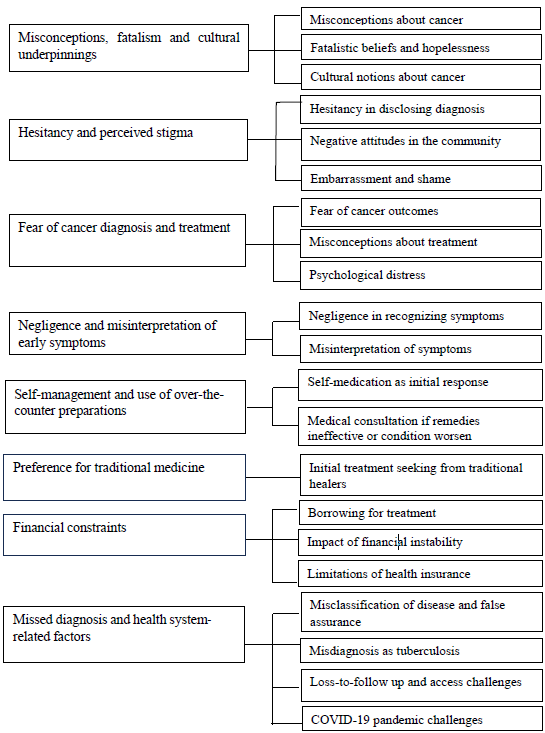
- Coding tree depicting key factors affecting health-seeking behaviour for cancer in Meghalaya.
Misconceptions, fatalism and cultural underpinnings
Misconceptions among 15 cancer respondents about the causes of cancer emerged as one of the major barriers to timely health seeking, both for males and females. Although 12 acknowledged and attributed their disease to habits such as alcohol consumption, smoking and betelnut chewing, a small proportion of the respondents (7/37) indulging in such habits did not believe that tobacco and betelnut chewing were risk-factors that potentially contributed to their disease. This risk-denial among these individuals was, according to them, based on their observation that not all tobacco smokers and betelnut consumers get cancer.
Beliefs related to the causes of cancer were often attributed to fate or bad luck. Fatalistic beliefs about cancer outcomes were narrated by some of the patients (10/37) as a result of which there was a sense of hopelessness and doubts regarding cancer treatment. Caregivers also mentioned that they had observed this fatalistic attitude in patients they cared for.
‘I really don’t know much about that, Kong [adult woman]. Perhaps it’s my fate that it has been written that I should suffer from this disease, so that is all. If any man is destined to suffer from this disease, there is no escape and it is not because of any other reason.’ (P-19, 65 yr, male)
HCPs and caregivers also highlighted prevalent cultural concepts in the community regarding the cause of cancers, such as the concept of bih (Khasi word). Bih is not an easily translatable word; its literal translation could be ‘poison’, but here, it does not really represent poison in the literal sense; rather it represents a concept in Khasi which embodies a situation associated with an illness acquired after a person has come in contact with or eaten food with/of a person with bad intent. Likewise, participants used words that represent an insect or germ within, but not necessarily as it is understood in a biomedical sense. Another term used was the word skai, likely equivalent to the evil eye in English, which is believed among Khasis to render one vulnerable to illness.
This ‘skai’ is fairly prevalent; individuals will give you this ‘skai’ just by looking at you. I’m not sure how to explain it, but that ‘skai’ is really common here, and we believe in it. For example, once a woman gives birth, they advise her not to display her baby to others since she would receive ‘skai’ from others. We heard/learnt of this from our elders’ (HCP-004)
Hesitancy and perceived stigma
While a cancer diagnosis was often disclosed to family members by the patient, there was hesitancy in disclosing the diagnosis among a few other participants (6/37), as they were ‘uncomfortable’ to talk about their diagnosis with friends and neighbours. Some caregivers also believed that disclosure could bring bad luck; hence they were hesitant.
‘Besides our own close relatives, I personally never tell. Because why would I tell right? Considering that, if I myself tell them, then its just like, it will bring bad luck. That is why I never want to tell others’(CG, 56 yr, female)
Some caregivers reported that negative attitudes within the community exacerbated the burden on the affected families. The concept of ‘kren jemdaw,’ referring to speaking negatively about a person, is believed to render them susceptible to illness or misfortune.
‘He used to share it with his own friends too. But he felt angry because there are other people who would be kren jemdaw. He would get angry with such people’ (CG, 29 yr, female)
Embarrassment and a sense of shame contributed to perceived stigma, depending on the body parts affected.. For example, female patients suffering from breast and cervical cancers expressed these feelings. This was corroborated by caregivers and HCPs.
‘Long time back… when the surgery was done, since her whole breast had been cut, she was embarrassed that people would notice’ (CG, 52 yr, male)
‘In case of breast and cervical cancer many patients feel shy to come seek help as they think it is shameful to tell others that they have problems in those areas. So, for so many years they try to self-manage and when the condition advances, they have no other way out than to show the doctors’(HCP-002)
Fear of cancer diagnosis and treatment
Fear surrounding cancer diagnosis and treatment among patients was predominantly expressed by the HCPs, who noted that many patients viewed cancer as incurable and synonymous with the end of life.
Misconceptions about cancer treatment, such as radiation and surgery, were also identified as the underlying cause of fear associated with seeking cancer treatment.
‘Patients think that radiation means they will be roasted (syang) in that machine or that they have to burn themselves in that machine but it is not like that. Radiation is also just like any other test like x-ray and all’ (HCP-003)
Such fear was commonly seen among the cervical and breast cancer patient respondents, who often harboured fearful and fatalistic beliefs. The fear of cancer diagnosis and treatment were also cited as reasons for incomplete therapy and loss to follow up by the HCPs. Cancer-induced psychological distress, caused by concern over the fate of dependent family members (especially children), family responsibilities, and inability to meet treatment costs, was also expressed by the patient respondents (11/37).
Negligence and misinterpretation of early symptoms
Sixteen patient respondents attributed the delay in treatment seeking to their own negligence, not recognizing their early symptoms as serious. They interpreted their symptoms as harmless and mild, often equating them to ailments such as cold, gastritis, ulcers, etc. Oral cancer patient respondents often attributed their mouth ulcers to common cold or transient mouth ulcers which they perceived to be caused by unwashed betel leaves.
Female cervical cancer patients aged over 40 yr often interpreted their symptoms as post-menopausal changes. There appeared to be a phase when they were constantly engaging in an internal debate on the seriousness of the issue and whether or not they needed to seek care. This ‘internal dialogue’ phase emerged as a key barrier to taking the first step in the health-seeking trajectory.
‘As days passed the flow was increasing, so later the flow stopped and the white discharges started. So, I thought to myself that since I have crossed 50 yr, it may be normal. So, it continued like that…’ (P-17, 54 yr, female)
Self-management and use of over-the-counter preparations
Self-medication was the primary response for managing the first symptoms in many patients (11/37), particularly among females (9/11). Medical consultation was sought only if self-remedies proved ineffective or if the condition worsened.
‘I applied ointment that I obtained from the pharmacy because I assumed it was an ulcer, and I never expected to acquire this kind of condition; yes, I went to the pharmacy and bought mouth ulcer medication’ (P-18, 42 yr female)
The tendency of self-medication among the patient respondents was also observed among the caregiver respondents (3/12), as they were also under the assumption that the early symptoms experienced by the patients were due to common ailments.
‘From the beginning we have been taking medicines from the pharmacy because we thought it was just a headache and that he would recover in only two or three days. He wasn’t very sick because he was just sneezing like that’ (CG,26 yr, female)
The above observations were further corroborated by HCPs, who mentioned that self-management of symptoms, by taking painkillers for pain, was common among cancer patients who neglected their health condition for a long time especially when there was symptomatic relief with over-the-counter preparations.
Preference for traditional medicine
Close to one-third (10/37) of the patient respondents first sought treatment from traditional healers. This preference for traditional medicine was more prevalent among males than in females. Traditional medicine was preferred as it was affordable, and accessible and widely used for various ailments.
‘I didn’t really pay much attention to it, so I went for traditional medicine since I have been used to taking such medicines’ (P, 38 yr, female)
Moreover, patients frequently reported positive experiences with traditional medicine for past illnesses; HCPs echoed similar observations. Additionally, recommendations from friends and neighbours also influenced patients to seek traditional medicine.
‘Yes, for cough and all I used to take that traditional medicine and it is very good for cough’ (P-03, 38 yr, female)
Preference for traditional healers as the first point of contact was also reported by some of the caregivers (3/12). A couple of patients (2/12) reported taking treatment from a traditional healer along with their modern medicine (biomedicine) provided from hospitals.
Financial constraints
Financial constraints affected the decision to seek treatment among one fourth (10/37) of the patient respondents. Patients had to borrow from friends and neighbours to cover the costs of treatment.
‘As the doctor advised, they sent me here at the appropriate time; however, I had to wait for a while because I didn’t have enough money to pay for the treatment. I had to arrange for the money and waited until I received it from my friends’ (P-019, 54 yr, male)
Some patients who initially could afford treatment at private hospitals, found themselves financially constrained, leading them to opt for subsidized cancer chemotherapy available at the government hospitals. Financial instability also compelled several patients to compromise on treatment decisions. The caregivers also highlighted that financial instability limited the patient’s choice to more affordable/subsidized services, offered by the government hospitals.
The HCP pointed out that financial constraints often led the patients to discontinue treatment.
‘Socio-economic constraint is a big reason that most of the people are unable to seek treatment. There are many who stop treatment because of lack of money. Patients in the far away rural areas need to pay a lot for their travel and food; therefore follow ups and many visits for treatment is not affordable to them’ (HCP-002)
Financial support through the Meghalaya Health Insurance Scheme (MHIS), which is a government-sponsored universal health insurance scheme for the residents of Meghalaya, was availed by nine patients. Patient respondents, however, expressed that MHIS was of little assistance, as it did not cover all the treatment costs. Among the caregivers, only five of 12 participants reported that the patients they cared for availed the MHIS, which helped cover small medical expenses (such as buying medicines), but was of little relief to their overall financial distress.
Missed diagnosis and health system-related factors
Some patient respondents (8/37) identified health system-related factors as the causes of delay in their cancer health seeking path. These included misclassifications of the disease as common ailments (such as gastritis) and false assurance from the treating physician/s that their signs and symptoms were harmless. A breast cancer patient explained that she left the swelling untreated based on the physician’s assurance that it was nothing of concern, only to be diagnosed with stage III cancer months later. Another patient said,
‘I don’t know sister, whether I sought treatment on time or have delayed. I can’t explain anymore, because from my side I went for treatment at the earliest, but the doctors themselves said it was gastritis, what else could I do?’ (P-022, 49 yr, female)
Misdiagnosis of the disease as tuberculosis and the prolonged antitubercular treatment thereof were also attributed as a factor responsible for the delay in treatment initiation among the lung cancer patients (2/6).
‘At first, the doctors said that it was TB so they took care of it. I took TB medications, an enormous amount of them I took every day for 4-5 months’ (P, 56 yr, female).
Loss-to-follow up of suspected cases referred from the peripheral health centres was common. As patients coming to the Civil Hospital Shillong hail from remote villages, the access to this hospital, or even the district hospitals, is challenging due to the geographical terrain and poor road conditions leading to increased transportation costs which, in turn, result in patients not visiting hospitals for follow up.
‘For suspected cases, we will make sure that they are referred. But whether they go or not, we cannot say anything. Because some of the patients, once they know about their suspected diagnosis, they give up as it is quite a distance to go to the city …’ (HCP-005, HCP)
Besides transportation difficulties, the HCPs stated long waiting hours, unavailability of physicians and delay in reporting as some of the other perceived reasons for the delay in initiating treatment.
Among the health system-related factors, the lack of cancer diagnosis and treatment facilities often compelled HCPs to refer patients to hospitals outside the state for treatment, which may be unaffordable. Absence of a professional counsellor in the hospital to address the psychological needs of the cancer patients, was also identified it as a gap in healthcare provision.
Several patients explained that the COVID-19 pandemic was one of the causes for delay in seeking healthcare, as they encountered difficulty in reaching the hospitals due to the travel restrictions imposed during the lockdown. Inadequate manpower during the pandemic also posed major challenges for the HCPs at the hospitals. A drastic decline in cancer patients visiting the hospital for follow up, during the pandemic, was highlighted by the HCPs.
Support and coping mechanisms
Despite enduring considerable uncertainty and challenges during their cancer treatment, patients and their families relied on various support and coping mechanisms. Religious faith emerged as the predominant facilitator in cancer health seeking among half of patient respondents (18/37) and their caregivers.
‘At first, we told at home, then to the other faithful; we prayed together. After the prayer we felt good and believed that God will show wonders in our lives’ (CG, 53 yr, female)
Almost all patients received emotional support from their families during their cancer treatment, fostering hope. Family support was cited as crucial to the health-seeking behaviour of seven patients, influencing their decision to seek medical consultation for symptoms and adhere to medical treatment.
Discussion
This study highlights the factors responsible for delayed cancer health-seeking behaviour in the tribal community of Meghalaya. The lack of correct knowledge about cancer and its treatment coupled with cultural beliefs among patients was also observed in another study conducted in three States of the NER14, and from studies conducted in Nigeria and Ethiopia15,16. With cancer-specific health education, misconceptions of cancer and delays in treatment seeking can be reduced17, but taking into consideration the underpinning cultural and contextual factors will likely improve acceptance.
Socio-demographic variables such as age and sex have often been implicated as determinants of delayed health-seeking behaviour among cancer patients18,19. Similarly, a higher proportion of women participants in this study with breast and cervical cancers were detected at stages III and IV. Breast and cervical cancer affects sexual reproductive organs of women and in the Khasi community generally, there is silence around sexuality, reproductive health or sexual and reproductive organs in homes or public spaces20. As a result, women tend to keep silent till they are unable to manage their illness. This problem is compounded with the low level of awareness about breast and cervical cancers among women in Meghalaya14.
Preference for traditional medicine in the treatment of cancer, as observed in this study, is due to the socio-cultural practices, affordability and acceptability of traditional medicine in the community21. One underlying reason for the preference of Khasis for traditional medicine involves their belief that certain ‘illnesses’ can be cured only by traditional medicine22. However, relying on alternative medicine, lacking empirical evidence of efficacy, may lead to squandered resources and time. While some research indicates that cancer patients using complementary alternative medicine tend to delay seeking conventional medical care23, this study did not ascertain comparable findings due to the unrecorded disease stage among participants opting for traditional medicine.
This study highlights various cultural underpinnings that influence health-seeking behaviour. Concepts such as ‘bih’ and ‘skai’ are culturally embedded notions in the Khasi community that are believed to be curable only by nongai dawai or Khasi traditional medicine. Albert et al22, noted a reference to ka bih and tuberculosis, where the traditional healer suggests that his therapies ameliorate the enervating effects of biomedical remedies that might only achieve a partial cure, because ‘the roots of the disease persisted, from poison or toxin (ka bih) remaining in the body,’ which otherwise remains unaffected by biomedical therapies.
Individuals with cancer from low socioeconomic background have been reported to have more advanced disease at diagnosis, to receive less aggressive treatment, and also to have a higher risk of mortality in the five yr following their cancer diagnosis24,25. Moreover, most health systems in LMICs are ill-equipped to manage the growing cancer burden, thus severely diminishing the survival rates among cancer patients26. Meghalaya including other States in NER has gaps in health infrastructure, qualified workforce, and related resources. These deficiencies in the health system further add to the burden of the impoverished population. Lack of easy access to healthcare centres due to the difficult hilly terrain and remote tribal areas, distance, multiple visits required for referrals and treatment, and inadequate coverage of the existing health insurance scheme in Meghalaya (MHIS), add an extra financial burden to rural dwellers of the region, resulting in delayed diagnosis and treatment12,27.
A limitation of this study is the potential lack of generalizability, as most of the participants were enrolled from a single government hospital, albeit a main referral centre with diverse patient background. Additionally, only individuals with specific cancer types were included, potentially limiting diversity of opinion. Most patient perspectives were also collected during the COVID-19 pandemic, potentially influencing their views on cancer care due to repurposed health workers and prioritized COVID-19 control, which may also limit the generalizability of findings beyond the pandemic context, necessitating further research on its specific impact on cancer health-seeking behaviour.
Nevertheless, this study highlights the barriers for cancer diagnosis and treatment in an indigenous or tribal population in Northeast India. Our findings underscore the need to address such misconceptions through culturally appropriate messaging via locally suited channels of communication, while addressing the health system-related barriers such as improving the capacity building of healthcare workers in cancer diagnosis and treatment. Integration of local tradition healers for early diagnosis and referral of cancer patients should help improve survival rates. Involving the local non-governmental organizations and self-help groups and village health committees28, in sensitization activities may increase community awareness, thereby leading to early healthcare seeking and better outcomes.
Financial support & sponsorship
This study was funded by the grant received from Indian Council for Medical Research – National Centre for Disease Informatics and Research, Bengaluru (NCDIR/CaRes-NER/8/2020/7501).
Conflict of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Latest global cancer data: Cancer burden rises to 19.3 million new cases and 10.0 million cancer deaths in 2020. Available from: https://www.iarc.who.int/wp-content/uploads/2020/12/pr292_E.pdf, accessed on October 8, 2023.
- Global cancer statistics 2020: GLOBOCAN Estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209-49.
- [Google Scholar]
- Cancer incidence estimates for 2022 & projection for 2025: Result from National Cancer Registry Programme, India. Indian J Med Res. 2022;156:598-607.
- [Google Scholar]
- Profile of Cancer and related health indicators in the North east region of India - 2021. Available from: https://ncdirindia.org/All_Reports/NorthEast2021/resources/NEComplete.pdf, accessed on November 16, 2023.
- Cancer scenario in North-East India & need for an appropriate research agenda. Indian J Med Res. 2021;154:27-35.
- [Google Scholar]
- Prevalence of use of tobacco, alcohol consumption and physical activity in the North east region of India. J Cancer Policy. 2021;27:100270.
- [Google Scholar]
- National Family Health Survey (NFHS-5) 2019-21 - State fact sheet Meghalaya. Available from: https://dhsprogram.com/pubs/pdf/FR374/FR374_Meghalaya.pdf, accessed on November 11,2023.
- Assessing the awareness level of breast and cervical cancer: A cross-sectional study in northeast India. Int J Med Sci Public Health. 2016;5:1987.
- [Google Scholar]
- Impact of educational level and family income on breast cancer awareness among college-going girls in Shillong (Meghalaya), India. Asian Pac J Cancer Prev. 2020;21:3639-46.
- [Google Scholar]
- Barriers to timely diagnosis and management of breast cancer: Observations from a tertiary referral center in resource poor setting. Indian J Surg Oncol. 2020;11:287-93.
- [Google Scholar]
- Meghalaya Population Census 2011. Available from: https://www.censusindia.co.in/states/meghalaya, accessed on March 8, 2024.
- The healthcare services delivery and medical supply management: The case of cancer management in North-east India. PBME. 2020;3:89-101.
- [Google Scholar]
- Profile of cancer and related health indicators in the North east region of India. Meghalaya. Available from: https://ncdirindia.org/All_Reports/NorthEast2021/resources/NE_chapter5.pdf, accessed on March 8, 2024.
- Assessment of knowledge and screening in oral, breast, and cervical cancer in the population of the Northeast region of India. JCO Glob Oncol 2020:601-9.
- [Google Scholar]
- Delayed treatment of symptomatic breast cancer: The experience from Kaduna, Nigeria. S Afr J Surg. 2008;46:106-11.
- [Google Scholar]
- A mixed-method assessment of beliefs and practice around breast cancer in Ethiopia: Implications for public health programming and cancer control. Glob Public Health. 2011;6:719-31.
- [Google Scholar]
- The impact of a breast cancer educational intervention in Ghanaian high schools. BMC Cancer. 2022;22:893.
- [Google Scholar]
- Treatment delay in oral and oropharyngeal cancer in our population: The role of socio-economic factors and health-seeking behaviour. Indian J Otolaryngol Head Neck Surg. 2011;63:145-50.
- [Google Scholar]
- Educational levels and delays in start of treatment for head and neck cancers in North-east India. Asian Pac J Cancer Prev. 2014;15:10867-9.
- [Google Scholar]
- Sexuality and ‘silence’ among Khasi youth of Meghalaya, Northeast India. Cult Health Sex. 2013;15:S351-64.
- [Google Scholar]
- Is ‘mainstreaming AYUSH ‘ the right policy for Meghalaya, Northeast India? BMC Complement Altern Med. 2015;15:288.
- [Google Scholar]
- Doktor Kot, Doktor Sla–book doctors, plant doctors and the segmentation of the medical market place in Meghalaya, Northeast India. Anthropol Med. 2019;26:159-76.
- [Google Scholar]
- Indian cancer patients’ use of Traditional, Complementary and Alternative Medicine (TCAM) and delays in presentation to hospital. Oman Med J. 2009;24:99-102.
- [Google Scholar]
- Low socioeconomic status increases risk of death after cancer diagnosis. Available from: https://www.sciencedaily.com/releases/2008/06/080623092544.htm, accessed on March 8, 2024.
- Impact of socioeconomic status on cancer incidence and stage and end results: National Longitudinal Mortality Study. Cancer Causes Control. 2009;20:417-35.
- [Google Scholar]
- Cancer control in low- and middle-income countries: Is it time to consider screening? J Glob Oncol 2019:1-8.
- [Google Scholar]
- cancer control in India: Current status, and control in India limiting factors. Paripex Indian J Res 2019:454-5.
- [Google Scholar]
- Village health sanitation and nutrition committees: Reflections on strengthening community health governance at scale in India. BMJ Glob Health. 2018;3:1-4.
- [Google Scholar]






