Translate this page into:
Malnutrition in tribal people living with tuberculosis in India: A systematic review & meta-analysis
For correspondence: Dr Saravanan Natarajan, Department of Biochemistry, ICMR – National Institute for Research in Tuberculosis, Chennai 600 031, Tamil Nadu, India e-mail: natrajan.s@icmr.gov.in
-
Received: ,
Abstract
Background & objectives
Tuberculosis (TB) remains a persistent public health challenge in India. The country also has high proportions of malnutrition in different areas, making the population susceptible to TB. Among vulnerable populations, such as tribal communities, TB and malnutrition pose significant threats. Tribal populations exhibit disproportionately higher TB prevalence rates compared to non-tribal groups. Also, malnutrition prevalence among tribal communities far exceeds national averages in India. Amidst fragmented data, a systematic review of nutritional status among tribal populations with TB in India is imperative to inform comprehensive intervention strategies.
Methods
Cross-sectional, case-control, cohort and interventional studies reporting the nutritional status of active TB affected individuals among tribal populations in India were specifically included if terms such as “malnutrition” or “low BMI” were used. This systematic review followed PRISMA guidelines and was registered with PROSPERO (CRD42020168328). The data was assessed using a random-effects model and standardized mean with 95% confidence interval (CI). The I2 statistics indicated heterogeneity. Publication bias was evaluated using funnel plots.
Results
Out of 124 studies, 20 were selected for initial screening, 15 were excluded due to a lack of appropriate data, and five were included for the final analysis. The pooled prevalence estimates of malnutrition among Indian tribes living with TB was 514 per 1000 people, with 95% CI: 232-791. The sensitivity analysis showed that no individual study influenced the estimation of pooled prevalence.
Interpretation & conclusions
In the background of India, contributing considerably to the burden of TB-related morbidity and mortality alongside undernutrition, reviews have underscored undernutrition as the predominant risk factor for TB, affecting over 50 per cent of the population in some States. This situation is exacerbated among the tribal communities in India due to the dual burdens of undernutrition and TB being more pronounced. Our systematic review consolidates evidence from five studies, revealing the prevalence of malnutrition among tribal TB patients. Conducting well-planned implementation research to address this dual burden among the underprivileged population would help achieve the ambitious goal of a TB-free India 2025.
Keywords
Malnutrition
Indian tribes
tuberculosis
body mass index
meta-analysis
Tuberculosis (TB) remains a major public health problem in India and across the globe. According to the Global Tuberculosis Report, in 2023, the World Health Organization (WHO) areas of South-East Asia accounted for 46 per cent of TB cases in 2022. Of these, India accounted for 27 per cent, which is the highest in the region1. According to the report on the National TB Prevalence Survey (2019–2021), the prevalence of TB among the adult population is 316 per 100,0002. In many parts of India, individuals with active TB, especially those with pulmonary TB, have coexisting undernutrition, which can be severe and life-threatening. Moreover, undernutrition is considered to be one of the risk factors for TB infection or the progression of latent TB into active TB. Malnutrition is also associated with unfavourable treatment outcomes. As evidenced by the data, the population-attributable fraction of TB due to malnutrition in India is as high as 61.5 per cent in women and 57.4 per cent in men3. A report4 on Indian pulmonary TB patients showed that an increase in body mass index (BMI) lowered the odds of death during treatment [Odds ratio (OR), 0.78 (95% CI: 0.68–0.9) for each unit increase in BMI] after adjustment for age, sex, treatment category, sputum smear and human immunodeficiency virus infection status4. A recent modelling study projected that modest reductions in undernutrition could reduce TB incidences by ∼4.8 (95% uncertainty range, 0.5 million – 17.1 million) over 20 yr in India5.
In India, about 104 million tribal people live in different geographical locations (8.6% of the total population) and are distributed among 705 tribes across the nation6. A common feature among the tribals in India is that they have poor health indicators, a greater burden of morbidity and mortality, and limited access to health care. The tribals are vulnerable to both TB and undernutrition. A systematic review and meta-analysis on pulmonary TB among tribal in India has shown that the pooled estimate of TB prevalence was 703 per 100,000 population6.
Malnutrition among tribal people in India, indicated by Chronic energy deficiency (CED), is 60 per cent7, while it is about 30 per cent among the general adult population in India8. Since malnutrition is a major risk factor for TB, strategies on nutritional intervention will be helpful in the efficient control of TB among this underprivileged population. Currently, available data is scattered and misrepresentative. Hence, a systematic review of nutritional status among the tribal population in India is essential to plan a comprehensive intervention strategy. The End TB strategy9 of WHO aims to decrease TB incidences by 90 per cent and deaths due to TB by 95 per cent by 2035, which is unlikely to succeed without targeting undernutrition. Therefore, the present systematic review is planned to generate the required information.
Material & Methods
This systematic review was carried out following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (registered with PROSPERO (CRD42020168328). No ethical approval was sought as this analysis is undertaken from previously published data.
Identification and eligibility of studies
We reviewed community-based studies that targeted the tribal population and included people aged ≥15 yr in order to ascertain the prevalence of malnutrition among the tribal population living with TB in India. Studies describing malnutrition were specifically included if the terms such as ‘malnutrition’ or ‘low BMI’ were used. As our inclusion criteria were restricted to studies that reported malnutrition or low BMI, it was crucial to consider additional aspects when evaluating the quality and dependability of the investigations. These considerations included study design, sample size and data collection methods.
Selection criteria
The search strategy was formulated according to the CoCoPop (condition, context and population) framework, which is recommended for systematic reviews of prevalence studies (Table I). We included the following studies for the analysis: cross-sectional, case-control, cohort study design and interventional study design reporting the baseline nutritional status of those with active TB. The main outcome considered was the prevalence of malnutrition in a tribal population living with TB in India. A low BMI was an indication of malnutrition. BMI was calculated by dividing a person’s weight in kilograms by the square of their height in meters. Only studies on people living with TB from Indian tribal communities were included.
| Component | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Condition | Malnourished or those with low BMI | Malnourished or low BMI is not quantified |
| Context |
Indian tribal people diagnosed with TB No time/period restrictions |
TB is not a primary variable |
| Population | Tribal people living in India |
Non-tribal populations in India Article not published in English |
TB, tuberculosis; BMI, body mass index
Search criteria
For meta-analysis, we included all population-based cross-sectional and cohort studies. A literature search was conducted in PubMed, Cochrane Library and Google Scholar using the following combination of keywords: ‘pulmonary tuberculosis’, ‘tribals’, ‘nutrition’, ‘India’ and ‘prevalence’. Only published articles in the language ‘English’ were included in this meta-analysis. The references cited in the retrieved articles were also reviewed, and those found relevant were selected. Two independent reviewers screened the title/abstract and full text using Rayyan QCRI10.
Critical appraisal
Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement was used to evaluate the quality of reporting11. Two reviewers worked on it. Discussion among the reviewers was used to settle disagreements, and when that was not feasible, a third reviewer took over.
Statistical analysis plan
A summary of reports on the prevalence of malnutrition among the tribal people living with TB was done using R software (Version. 4.4.1 for Windows) 12. Meta-analysis of prevalence data was analyzed, pooled and estimated with a 95 per cent confidence interval (CI) using the ‘metafor’ package of R software13. Forest plots displayed prevalence with corresponding 95 per cent CIs for each study. The overall random-effects pooled estimate with its CI is reported in this paper. Due to the nature of the studies, substantial heterogeneity was expected. Hence, a random-effects meta-analysis was done with the estimate of heterogeneity being taken from an inverse-variance model14. Publication bias was assessed using Egger’s test, as well as a visual inspection of the funnel plot. Between-study heterogeneity was evaluated using Higgin’s I2 and Cochran’s Q method; I2 values of 25, 50 and 75 per cent were considered low, moderate and high heterogeneity, respectively15. A χ2 for Q determined the significance of heterogeneity, and a P<0.05 was considered significant. The impact of any single study on the overall results was assessed using a leave-one-out sensitivity analysis, in which each study was iteratively removed, and the findings were compared to the overall meta-analysis.
Results
We collected 124 articles as per the search criteria. They were all screened based on title and abstract, from which 20 articles were shortlisted for review. Three studies were excluded upon preliminary scrutiny as they did not fulfil the inclusion criteria. Eight articles provided secondary data related to the study’s objective; nevertheless, a detailed review showed that the information provided in those articles was irrelevant and, hence, excluded. Another four articles were not included since they did not carry information on malnutrition among tribal people living with TB (Fig. 1). Assessment specifics of studies is shown in Table II16-20.
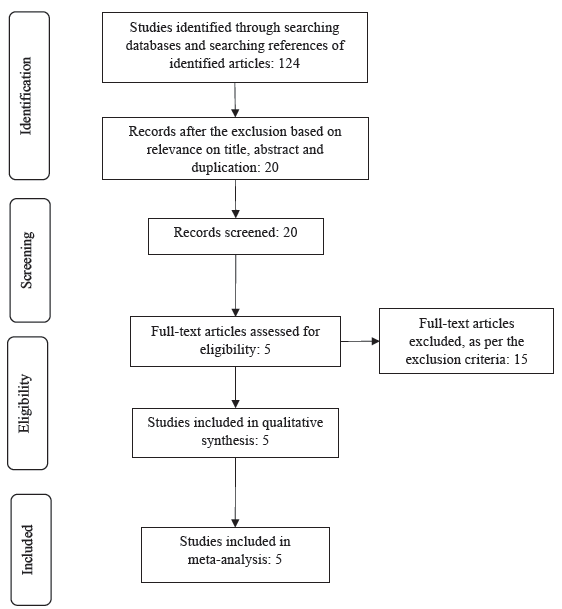
- PRISMA flow diagram showing the process of study selection.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bhat et al16 (2017) | |||||||||||||||||||||
| √ | √ | √ | √ | √ | √ | √ | √ | * | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | |
| Tungdim et al19 (2008) | |||||||||||||||||||||
| √ | √ | √ | √ | √ | √ | √ | √ | * | √ | √ | √ | √ | √ | √ | √ | √ | * | √ | √ | √ | |
| Tungdim et al20 (2010) | |||||||||||||||||||||
| √ | √ | √ | √ | √ | √ | √ | √ | * | √ | √ | √ | √ | √ | √ | √ | √ | * | √ | √ | √ | |
| Bapat et al18 (2015) | |||||||||||||||||||||
| √ | √ | √ | √ | √ | √ | √ | √ | * | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | |
| Rao et al17 (2018) | |||||||||||||||||||||
| √ | √ | √ | √ | √ | √ | √ | √ | * | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | |
Note: 1. Title & abstract; 2. Introduction/background; 3. Objectives; 4. Study design; 5. Setting; 6. Participants; 7. Variables; 8. Data; 9. Bias; 10. Study size; 11. Quantitative variables; 12. Statistical methods; 13. Descriptive data; 14. Outcome data; 15. Main results; 16. Other analyses; 17. Key results; 18. Limitations; 19. Interpretation; 20. Funding
√, Good description; %, Partial description; *, No description
Included studies
Five publications fulfilling the study’s requirements were considered for analysis since they reported on two necessary factors: malnutrition and TB among Indigenous people. The majority of studies used bacteriological tests such as sputum smear and culture examination as confirmatory procedures for TB. The details of people living with TB were acquired from both survey data in the tribal areas and TB treatment facilities. Anthropometric data were used to determine malnutrition in all five articles. Their characteristics are briefed in Table III.
|
Study ID |
Author | Year | State |
Tribe name |
Study design |
Study start |
Study end |
Sample size |
Tribal population |
Mean age (yr) |
TB cases |
Malnourished with TB |
Nutritional status assessment method |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Bhat et al16 | 2017 | Madhya Pradesh | Saharia | Case-control | March 13 | Nov 13 | 12123 | 10259 | 39.4 | 267 | 228 | BMI |
| 2 | Bapat et al18 | 2015 | Maharashtra | Korku | Prospective cohort | May 9 | Jun 11 | 419 | N/A | N/A | 252 | 32 | BMI |
| 3 | Tungdim et al19 | 2008 | Manipur | Mongoloid | Cross-sectional | N/A | N/A | 247 | N/A | N/A | 167 | 88 | BMI |
| 4 | Tungdim et al20 | 2010 | Manipur | Mongoloid | Prospective case-control | Aug-00 | July 1 | 228 | N/A | N/A | 108 | 46 | BMI |
| 5 | Rao et al17 | 2018 | Madhya Pradesh | Saharia | Cross-sectional | Nov 13 | Oct 14 | 10300 | 9964 | 39.7 | 220 | 141 | BMI |
N/A, not available
A case-control study conducted in Gwalior, India (March-November 2013) on the Saharia community (n=10259) revealed 267 TB cases, with 228 being underweight. This underscores targeted advocacy needs for nutritional interventions among tribal TB patients16. In a 2013–2014 cross-sectional study17 in Shivpuri, Madhya Pradesh, 220 pulmonary TB cases and 660 controls were analyzed. The findings highlighted substantial correlations in Saharias between pulmonary TB risk and undernutrition17.
A study18 conducted in Maharashtra, India (May 2009-June 2011) focused on Melghat tribal community members with TB, where morbidity and mortality are primarily due to TB and malnutrition. Out of 275 individuals, 91.6 per cent were underweight (BMI < 18.5), with 70.2 per cent showing low diet intake and 33.7 per cent were severely malnourished. Among malnourished individuals, 32 exhibited Mycobacterium TB (M. tb) positivity18.
In Manipur, northeastern India, two studies on tribal individuals with TB included a cross-sectional and a case-control study at four TB facilities involving 247 adult males. Participants, categorized by treatment stage, exhibited improved post-therapy nutritional status, evidenced by decreased percentages of low BMI (<18.5 kg/m2) in affected individuals before starting treatment (64.5%), those who had completed two months of treatment (49%), and after completing treatment (34%) groups, compared to controls (6.3%). The study underscores enhanced nutritional outcomes following TB treatment, as demonstrated by various anthropometric indices19.
A case-control study20 conducted in Manipur, India (August 2000-July 2001) focused on adult TB affected individuals (20-40 yr). Of 108 cases with standard treatment, 46 were underweight. Anthropometric measurements revealed higher CED (42%) and undernourishment (64.8%) among TB affected individuals compared to controls, indicating compromised nutritional status with pulmonary tuberculosis onset involving muscle and fat loss20.
Meta-analysis
A random-effects meta-analysis was conducted because of expected variations between the studies. The meta-analysis indicated that variability between studies was high (T2 = 0.11; heterogeneity I2 = 99% with heterogeneity chi-square = 358.92, degrees of freedom (DF) = 4 and P<0.01). Our calculations indicated that 99 per cent of the variation observed in the pooled estimate was due to heterogeneity among the studies. Individual study prevalence estimates of malnutrition ranged from 8.6 to 89.6 per cent. Each study was given approximately equal weightage, ranging from 19.8 to 20.1 per cent, due to high heterogeneity between studies. Based on the random effects model, the pooled estimate of the prevalence of malnutrition was 514 per 1000 people infected with TB in the tribal population with a 95 per cent CI: 232–791. The P<0.01 indicates that the heterogeneity of the pooled results was significant. A forest plot with the pooled estimate (marked as a diamond with a vertical dotted line) with a 95 per cent CI, as obtained from the random effects model, is displayed in Figure 2. Also depicted are the estimates of the prevalence of malnutrition among the TB positives from the individual studies (marked as circles), along with their 95 per cent CIs.
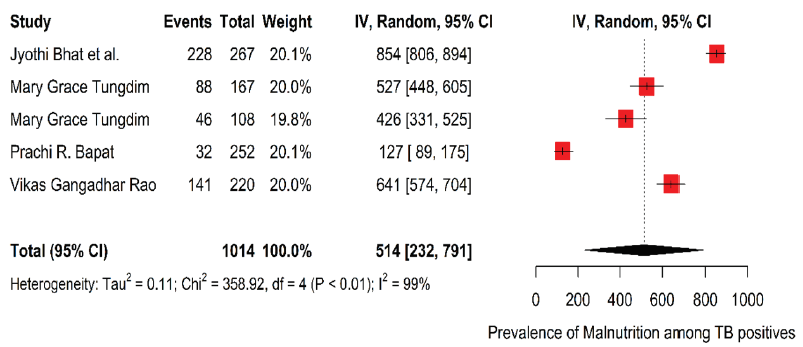
- The forest plot visualization of malnutrition prevalence among TB affected individuals with 95% CI per 1000 population. Weight refers to the weightage given to each study for statistical analysis. IV, random 95% CI refers to an inverse-variance random-effects model with a 95% CI. CI, confidence interval.
Publication bias
An attempt was made to assess the publication bias using a funnel plot and Begg’s and Egger’s test. However, the funnel plot method and other tests were underpowered due to a small number of studies. However, the result of effect estimates against its standard error was plotted and Egger’s test showed that it did not indicate the presence of funnel plot asymmetry with a P value of 0.834 (Fig. 3).
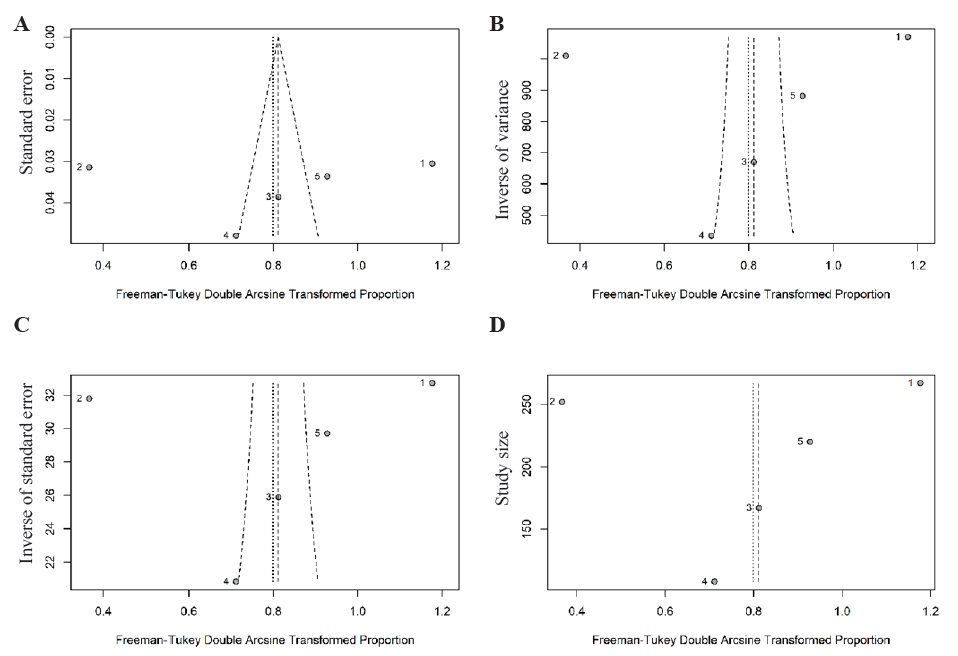
- Funnel plot to show asymmetry of logit transformed prevalence against (A) standard error, (B) inverse of variance, (C) inverse of standard error and (D) study size. Egger’s test does not indicate the presence of funnel plot asymmetry (P = 0.834).
Sensitivity analysis
A sensitivity analysis was performed, which indicated that there was no influence of an individual study on the estimation of pooled prevalence. The resulting pooled estimate still fell within the 95 per cent CI of the original pooled estimate, even after the removal of any specific study at a time. This indicated the stability of our results. Heterogeneity among studies persisted. The sensitivity analysis is graphically depicted in Figure 4, where the vertical dotted line is the actual pooled estimate, we calculated using the random effects model along with its 95 per cent CI.
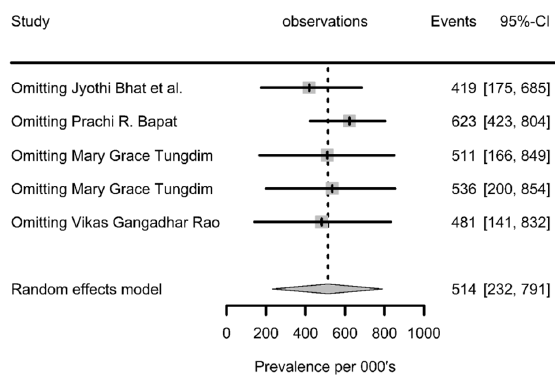
- A sensitivity analysis plot of malnutrition prevalence estimates with 95% CI per 1000 tuberculosis positive population (after omitting studies one after another).
Discussion
TB is not only a public health crisis but also a socioeconomic catastrophe. India has the largest global burden of TB-related morbidity and mortality, as well as undernutrition. This situation has compounded the effect of TB as indicated by a recent review, which showed that the most significant risk factor for TB in India is undernutrition, which affects more than 50 per cent of the population in most States21.
The current systematic review has summarized the results from five different studies on TB and malnutrition in the tribal population. The meta-analysis showed that the overall prevalence of malnutrition among those with TB in the tribal population is 514 per 1000 (95 per cent CI: 232,791). High heterogeneity between the studies was observed with heterogeneity l2 =99 per cent and heterogeneity chi-square=358.92.
In conclusion, our work adequately established the high prevalence of undernutrition among the TB patients of the tribal populations in India. There is a need for implementation research among the tribal population in terms of prevention, diagnosis and treatment. A recent cluster randomized trial in Jharkhand, India, which consisted of two thirds tribal population, showed that the effect of nutritional support on TB incidence in household contacts was associated with a substantial (39-48%) reduction in TB incidence in the household during the two yr of follow up. Such biosocial interventions will accelerate TB control in communities with TB and undernutrition22.
The Ministry of Health and Family Welfare and the Ministry of Tribal Affairs announced the Tribal TB Initiative23 on 26 March 2021 to address TB in India’s tribal populations, which are known to have a higher prevalence of the disease than the general population24. The Government of India’s Nikshay Poshan Yojana (NPY) is a Direct Benefit Transfer scheme under the National Tuberculosis Elimination Programme (NTEP), which offers INR 500 monthly to all notified patients with TB for nutritional support during the period of anti-TB treatment. A study has shown that the coverage of NPY among patients with TB had increased and the time to receipt of benefit had halved in the past five yr25. However, the policy implications should go beyond endorsing nutrition supplementation alone and promote ongoing initiatives to tackle issues such as hunger, poverty, unemployment, inequality and systemic disadvantage.
The strength of this systematic review is that the included studies were selected after a thorough quality assessment. However, this systematic review has some limitations. First, there is a limited number of articles, making the data insufficient to draw a strong conclusion. Second, the study population was only from three States in India, which may not be representative of the diverse tribe population and age groups across the country, and also required inputs using different screening platforms. Therefore, the results may be over- or underestimated among the included studies. Finally, the funnel plot suggests the existence of publication bias, so our results must be interpreted with caution. Despite the limitations of our review, it summarises the prevalence of undernutrition among tribal communities living with TB and could be used as a reference for future studies.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Global tuberculosis report 2023. Available from: https://iris.who.int/bitstream/handle/10665/373828/9789240083851-eng.pdf?sequence=, accessed on October 23, 2023.
- National TB Prevalence Survey in India 2019 – 2021. Available from: https://tbcindia.mohfw.gov.in/wp-content/uploads/2023/05/25032022161020NATBPSReport.pdf, accessed on October 23, 2023.
- Comorbidities in pulmonary tuberculosis cases in Puducherry and Tamil Nadu, India: opportunities for intervention. PLoS One. 2017;12:e0183195.
- [CrossRef] [PubMed] [Google Scholar]
- Nutritional status of adult patients with pulmonary tuberculosis in rural central India and its association with mortality. PloS One. 2013;8:e77979.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Estimating the impact of reducing under-nutrition on the tuberculosis epidemic in the central eastern States of India: a dynamic modeling study. PloS One. 2015;10:e0128187.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pulmonary tuberculosis among tribals in India: A systematic review & meta-analysis. Indian J Med Res. 2015;141:614-23.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tribal Health in India - Bridging the gap and a roadmap for the future. Available from: https://nhm.gov.in/nhm_components/tribal_report/Executive_Summary.pdf, accessed on October 23, 2023.
- National Family Health Survey (NFHS-5) 2019-21. Compendium of fact sheets, Key indicators India and 14 States/UTs (Phase II). Available from: https://mohfw.gov.in/sites/default/files/NFHS-5_Phase-II_0.pdf, accessed on October 23, 2023.
- Undernutrition and tuberculosis: public health implications. J Infect Dis. 2019;219:1356-63.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1-34.
- [CrossRef] [PubMed] [Google Scholar]
- Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- R Version 4.4.1 for Windows: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria 2016. Available from: https://cran.r-project.org/bin/windows/base/, accessed on August 29, 2024
- Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1-48.
- [Google Scholar]
- Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177-88.
- [CrossRef] [PubMed] [Google Scholar]
- Investigation of the risk factors for pulmonary tuberculosis: a case–control study among Saharia tribe in Gwalior district, Madhya Pradesh, India. Indian J Med Res. 2017;146:97-104.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A comparative study of the socio-economic risk factors for pulmonary tuberculosis in the Saharia tribe of Madhya Pradesh, India. Trans RSoc Trop Med Hyg. 2018;112:272-8.
- [CrossRef] [Google Scholar]
- Differential levels of alpha-2-macroglobulin, haptoglobin and sero-transferrin as adjunct markers for TB diagnosis and disease progression in the malnourished tribal population of Melghat, India. PLoS One. 2015;10:e0133928.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tuberculosis treatment and nutritional status among the tribals of Northeast India. Acta Biol Szeged. 2008;52:323-7.
- [Google Scholar]
- Nutritional status and chronic disease among the adult tribal population of Northeast India. Open Anthropol J. 2010;3:188-91.
- [CrossRef] [Google Scholar]
- Undernutrition & tuberculosis in India: Situation analysis & the way forward. Indian J Med Res. 2016;144:11-20.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Nutritional supplementation to prevent tuberculosis incidence in household contacts of patients with pulmonary tuberculosis in India (RATIONS): A field-based, open-label, cluster-randomised, controlled trial. Lancet. 2023;402:627-40.
- [CrossRef] [PubMed] [Google Scholar]
- Available from: https://swasthya.tribal.gov.in/, accessed on September 16, 2022.
- Nutrition profile of certain Indian Tribes. In: Samal PK, ed. Proceedings of a National seminar on Tribal Development options. Almora, India: GB Pant Institute of Himalayan Environment & Development; 1996.
- [Google Scholar]
- Direct benefit transfer for nutritional support of patients with TB in India-analysis of national TB program data of 3.7 million patients, 2018-2022. BMC Public Health. 2024;24:299.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






