Translate this page into:
Pooled prevalence of hypothyroidism among Indian females with infertility: A systematic review & meta-analysis
For correspondence: Dr Pushpanjali R. Ojha, Department of Pathology, Trauma and Central Emergency Laboratory, Rajendra Institute of Medical Sciences, Ranchi, Jharkhand 834 009, India e-mail: drprojha@gmail.com
-
Received: ,
Abstract
Background & objectives
Studies suggest hypothyroidism is responsible for female infertility. This review aimed to determine the pooled prevalence of hypothyroidism in Indian infertile women so that hypothyroidism screening can be initiated, and policies are designed for prevalence reduction.
Methods
Electronic databases including PubMed, Google Scholar and Cochrane library were searched to obtain the relevant articles. Studies that reported the proportion of hypothyroidism in Indian infertile women were selected. Systematic procedures for study selection and data extraction were followed. Each study was evaluated for quality using the Joanna Briggs institute (JBI) critical appraisal checklist. To pool the effect sizes, a random effects model was utilized. Funnel plot and Egger’s test were used to assess publication bias. To quantify heterogeneity among studies, I2 statistics were utilized. Subgroup and meta-regression analyses were used to further investigate the heterogeneity of pooled estimates. The sensitivity analysis done whereby each study was excluded in order to examine the influence of that study in the pooled estimate. A P-value of 0.05 or less was considered statistically significant.
Results
Out of 198 articles, a total of 20 studies involving 2396 cases met the inclusion criteria. The pooled prevalence of hypothyroidism in women with infertility was 28 per cent [95% confidence interval (CI): 20% to 36%] which was highest in Telangana at 62 per cent (n=1; 95% CI 48% to 74%) and lowest in Karnataka at 14 per cent (n=2; 95% CI: 10% to 18%).
Interpretation & conclusions
Infertile women have high proportion of hypothyroidism, suggesting that screening programmes during diagnostic workup for infertility may provide optimal care. The result of this meta-analysis will help design guidelines and earmark highest prevalence regions to initiate preventive and diagnostic measures for prevalence reduction in future.
Keywords
Hypothyroidism
infertility
Indian female
meta-analysis
pooled prevalence
systematic review
Women of the reproductive age group are more likely to have thyroid problems. Reportedly, about 11 per cent of women had thyroid autoimmunity, 2-3 per cent had hypothyroidism, and 1-2 per cent had hyperthyroidism in the United States as of the early 90’s1. Furthermore, around 27.5 million couples attempting to conceive were reportedly affected by infertility1. According to the Indian consensus (1981, 1991, 2001), the infertility trend among Indian women has increased with every passing decade and affects between 10 and 14 per cent of the Indian population2. Women who have Graves’ and Hashimoto’s disease have difficulty to conceive and infertility reportedly affects about 50 per cent of them. For years, the dropping fertility rate has been a source of concern, and numerous treatment methods have been implemented to address the possible causes. Whereas infertility associated with hypothyroidism can be managed easily, untreated thyroid disorders may increase the risk for sub-fertility and infertility. A study on 438 infertile women demonstrated that a significantly higher proportion of thyroid peroxidase antibody (TPO-ab) positivity in infertile women compared to healthy fertile women3.
The increased release of thyroid stimulating hormone (TSH) and prolactin (PRL) is one of the elements considered to be significant in limiting the development of pregnancy. PRL overproduction has a dramatic effect because it impairs gonadotrophin activity at the ovarian level and gonadal steroid secretion, altering positive feedback effects at the hypothalamus and pituitary levels. This results in an inability to produce gonadotrophins resulting in infertility.
In addition to this, hypothyroidism affects the menstrual cycle and inhibits ovulation. Numerous researches conducted in India have already established a link between hyperprolactinemia and hypothyroidism with infertility. To have data on proportion of hypothyroidism in women with infertility in India will add substantial information in the literature; therefore, the objective of current meta-analysis is to determine the pooled proportion of hypothyroidism in women with infertility in Indian population.
Material & Methods
Search strategy
The PRISMA guidelines 2020 were used to conduct this systematic literature review (PRISMA checklist attached as Supplementary material). An electronic search was conducted using the databases PubMed, Cochrane Library, and Google Scholar. English language and human subjects were used as search filters. The following free text words and medical subject heading (MeSH) terms were used (“TSH” [All Fields] OR (“hypothyroidal” [All Fields] OR “hypothyroidic” [All Fields] OR “hypothyroidism” [MeSH Terms] OR “hypothyroidism” [All Fields] OR “hypothyroid” [All Fields] OR “hypothyroidisms” [All Fields] OR “hypothyroids” [All Fields])) AND (“infertiles” [All Fields] OR “infertilities” [All Fields] OR “infertility” [MeSH Terms] OR “infertility” [All Fields] OR “infertile” [All Fields] OR “infertility s” [All Fields]) AND (“India” [MeSH Terms] OR “India” [All Fields] OR “India s” [All Fields] OR “indias” [All Fields]) (Fig. 1).
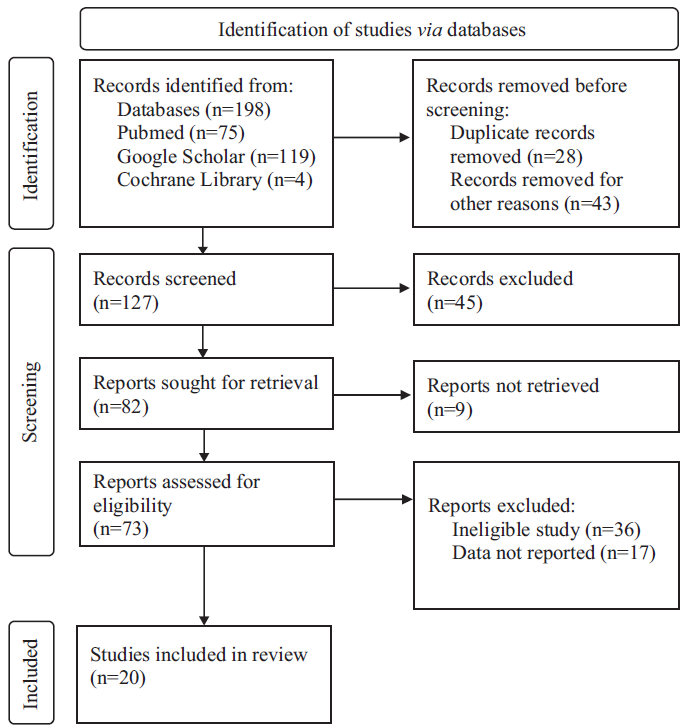
- Study flow diagram.
Selection criteria
Studies reporting the prevalence of hypothyroidism among infertile Indian women were included in the review. The following were the inclusion criteria: (i) community or hospital-based studies conducted in patients with primary or secondary infertility; (ii) studies determining the prevalence of hypothyroidism (subclinical, overt, or unspecified); (iii) research undertaken in India; (iv) cross-sectional, cohort-based and case control study designs; (v) TSH level was used for diagnosis of hypothyroidism.
Exclusion criteria included the following: (i) studies undertaken in the specialized field, such as mothers who have diabetes or mothers who are pregnant with history of miscarriages, etc.; (ii) studies which do not define infertility (primary or secondary) and (iii) studies not reporting TSH data and data required for the pooled analysis.
Data extraction
After identifying suitable studies, two authors extracted the required data for proportional meta-analysis separately. The following data were extracted: author(s) name, publication year, location of study, mean age in the study population, site of study (hospital- or community- or data-based), type of study, sample size and prevalence of hypothyroidism. Any discrepancies in data were resolved through consensus. In the event of a disagreement between two reviewers, the third reviewer arbitrated.
Statistical analysis
A logistic normal random effect model after the inverse of Freeman-Tukey double arcsine transformation was used to calculate the pooled prevalence of hypothyroidism with 95% confidence interval (CI). Since the proportion data need not follow normal distribution, the prevalence estimates were converted with the Freeman-Tukey double arcsine transformation prior to pooling in order to achieve a closer approximation to the normal distribution (Fig. 2). Publication bias was assessed using Funnel plot and Egger’s test. Meta-regression analysis was conducted to explore the source of heterogeneity and to determine the moderator effects of potential variables. Methodological quality of the studies was assessed using the Joanna Briggs Institute (JBI) tool (Fig. 3). We used the statistical analysis software STATA (Version 18, SE-Standard Edition, StataCorp LLC, TX, USA). A P value of 0.05 or less was considered as significant.

- Study Forest plot.

- Subgroup analysis based on the methodological quality of studies.
Result
Study characteristics
Our search term obtained 198 articles from India out of which a total of 20 studies involving 2396 cases met the inclusion criteria. Characteristics of included studies are shown in Table I. Four studies were reported from Uttar Pradesh4-7, three from Delhi8-10 and Maharashtra11-13 each, two from Karnataka14,15 and one each from Rajasthan16, Meghalaya17, Telangana18, Punjab19, Jharkhand20, Bihar21, West Bengal22, Andhra Pradesh23. Mean ages of participants across the chosen studies ranged from ranged from 26 to 35 yr.
| Author | Year | States | Study design | Study period | Cases (TSH) | Cases (PRL) | Total sample | median age in years/mean/range |
|---|---|---|---|---|---|---|---|---|
| Agarwal A et al 4 | 2019 | Uttar Pradesh | Prospective | Sep 2016 to Dec 2018 | 15 | 37 | 80 | 18-40 |
| Biradar SM et al 14 | 2012 | Karnataka | Case control study | 1 yr | 8 | NA | 50 | 20-35 |
| Fupare S et al 11 | 2015 | Maharashtra | Case control study | 2010-2012 | 22 | 54 | 120 | 19-45 |
| Goswami B et al 8 | 2009 | Delhi | case control study | 6 months | 13 | 66 | 160 | 20-40 |
| Hivre MD et al 12 | 2013 | Maharashtra | Cross sectional study | Aug 2012 to Aug 2013 | 10 | NA | 50 | 20-40 |
| Mehra D et al 5 | 2018 | Uttar Pradesh | Prospective | 2016 to 2017 | 22 | 26 | 100 | 20-40 |
| Nath C et al 17 | 2016 | Meghalaya | Case control study | NA | 13 | NA | 53 | 20-40 |
| Gupta MK et al 6 | 2016 | Uttar Pradesh | case control study | 2015 | 15 | NA | 30 | 22.52 ± 2 |
| Pallavi S et al 18 | 2020 | Telangana | case control study | Jun 2018 to May 2019 | 37 | 15 | 60 | 22.5 ± 33 |
| Sinha S et al 15 | 2020 | Karnataka | Cross sectional study | Jan to Aug 2012 | 30 | 221 | 16-43 | |
| Yadav A et al 9 | 2014 | Delhi | case control study | NA | 151 | NA | 206 | 20-35 |
| Nemade ST et al 13 | 2012 | Maharashtra | case control study | NA | 9 | NA | 50 | 20-40 |
| Seth B et al 10 | 2013 | Delhi | Cross sectional study | NA | 32 | 22 | 113 | 20-35 |
| Verma I et al 19 | 2012 | Punjab | Cross sectional study | Feb 2007 to Mar 2010 | 94 | 73 | 394 | 20-40 |
| Priya DM et al 7 | 2015 | Uttar Pradesh | Prospective | Mar 2013 to Aug 2014 | 51 | NA | 95 | NA |
| Aziz T et al 20 | 2020 | Jharkhand | Case control study | NA | 9 | NA | 50 | 23.5±2.48 |
| Lal Rz et al 16 | 2016 | Rajasthan | Case control study | NA | 18 | NA | 100 | 20-45 |
| Shirazee HH et al 22 | 2021 | West Bengal | Prospective observational study | Jan 2017 to Jul 2018 | 69 | NA | 314 | 20-40 |
| Kameswaramma K et al 23 | 2016 | Andhra Pradesh | Case control study | 1 yr | 9 | NA | 50 | 19-40 |
| Sushilendu V et al 21 | 2020 | Bihar | Cross sectional | Aug 2017 to Jul 2018 | 52 | 20 | 100 | 20-40 |
TSH, thyroid stimulating hormone; PRL, prolactin; NA, not available
The highest prevalence of hypothyroidism in infertile women was observed in Telangana, from a single reported study (n=1; proportion 62%; 95% CI: 48-74%) followed by Bihar (n=1; proportion 52%, 95% CI: 42-62%), Uttar Pradesh (n=4; pooled proportion 35%; 95% CI: 17-54%), Delhi (n=3; pooled proportion 34%; 95% CI: 3-78%), Meghalaya (n=1; proportion 25%; 95% CI: 14-38%), Punjab (n=1; proportion 24%, 95% CI: 20-28%) and West Bengal (n=1; proportion 22%, 95% CI: 18-27%). Prevalence in Maharashtra (n=3; pooled proportion 19%, 95% CI: 14-24%), Jharkhand (n=1; proportion 18%, 95% CI: 9-31%), Rajasthan (n=1; proportion 18%, 95% CI: 11% to 27%), Andhra Pradesh (n=1; proportion 18%, 95% CI: 9-31%) and Karnataka (n=2; pooled proportion 14%, 95% CI: 10-18%). Methodological quality of studies included in the current meta-analysis is shown in Table II. The pooled prevalence of hypothyroidism in women with infertility was 28% (95% CI: 20-36%) in this study.
| Author | q1 | q2 | q3 | q4 | q5 | q6 | q7 | q8 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Agarwal A | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 5 |
| Biradar SM | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 6 |
| Fupare S | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 5 |
| Goswami B | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 6 |
| Hivre MD | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 4 |
| Mehra D | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 5 |
| Nath C | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| Gupta MK | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 2 |
| Pallavi S | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 4 |
| Sinha S | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 4 |
| Yadav A | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 4 |
| Nemade ST | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 5 |
| Seth B | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 7 |
| Verma I | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 4 |
| Priya MD | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 4 |
| Aziz T | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 5 |
| Lal Rz | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 5 |
| Shirazee HH | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 6 |
| Sushilendu V | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 4 |
| Kameswaramma K | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 5 |
q1: Were the criteria for inclusion in the sample clearly defined?
q2: Were the study subjects and the setting described in detail?
q3: Was the exposure measured in a valid and reliable way?
q4: Were objective, standard criteria used for measurement of the condition?
q5: Were confounding factors identified?
q6: Were strategies to deal with confounding factors stated?
q7: Were the outcomes measured in a valid and reliable way?
q8: Was appropriate statistical analysis used?
JBI, Joanna Briggs Institute
Publication bias
We did not observe the significant publication bias in the included studies evident by funnel plot and Egger test (P value=0.820) (Fig. 4).

- Funnel plot with pseudo 95% confidence limit (P=0.82). ES, effect size.
Meta-regression analysis
Our meta-regression analysis showed an increasing trend of hypothyroidism with the year of conduct/publication of the selected studies, however, this was not statistically significant (P-value= 0.540) (Fig. 5). The meta-regression analysis did not observe any significant influence of mean age on the pooled proportion of hypothyroidism in infertile women in India (P value=0.160) (Fig. 6). The sensitivity analysis was done whereby each study was excluded in turn to examine the influence of each study in the pooled estimate. The sensitivity analysis did not observe the highly influential effect of any single study in the pooled proportion (Fig. 7).

- Bubble plot for determining variation in the proportion of infertility considering year of publication as moderator variables (P=0.54).

- Bubble plot for determining variation in the proportion of infertility considering mean age as moderator variables (P=0.16).

- The sensitivity analysis. X-axis denotes the distribution of estimates across numerical cut off value (y-axis) of the lower and upper confidence interval limits from left to right for the studies included in the meta-analysis.
Methodological quality of studies
Out of the 20 selected studies, 11 had total quality score of >5 and 9 studies had total quality score of <5. According to high and low methodological quality, our analysis suggests that prevalence was higher in the low methodological quality studies (pooled proportion 37%, 95% CI: 21-54%) than good quality studies (pooled proportion 21%; 95% CI: 15-28%).
Discussion
This study included publications that were reported from India to generalize the findings for proportion of hypothyroidism among Indian infertile women. Hypothyroidism was present in a significant proportion of infertile Indian women with pooled proportion of 28% (95% CI: 20-36%) in present study. The State wise prevalence estimates show highest prevalence in Telangana followed by Bihar, Uttar Pradesh and Delhi4-10,18,21. Other States show relatively lower prevalence (25 to 14%) of hypothyroidism among infertile Indian women11-17,19,20,22,23. None of the studies reported prevalence less than 14 per cent among studies reported from India. The variation in the prevalence of hypothyroidism across different States can also be explained by several reasons like cultural and dietary differences, life style, substance abuse, stress, genetic factors etc24.
Thyroid gland disorders result in reduced level of peripheral thyroid hormone – triiodothyronine (T3) and tetraiodothyronine (T4). This signals the hypothalamus to release thyroid releasing hormone (TRH) which stimulates the production of TSH and PRL from the pituitary gland. The follicular and granulosa cells of ovaries express thyroid receptors that are sensitive to the thyroid hormone levels thus vulnerable to be affected in hypothyroidism19,25. The abnormal production of the thyroid hormone results in menstrual abnormalities, anovulatory cycles and infertility26. Prolactin may also impair ovarian function by altering gonadotropin releasing hormone (GnRH) pulsatility thereby reducing the reproductive potential27. Mehra et al5 stated that thyroid dysfunction and hyperprolactinemia are one of the major causes of infertility5. The American Thyroid Association (ATA) provided clinical practice guidelines for management of hypothyroidism28. It has been suggested that in the context of elevated TSH values, the primary goal of treatment should be to rectify hypothyroidism before considering additional causes of hyperprolactinemia5. In established hypothyroidism, hormone therapy with thyroxin is the preferred therapeutic regime that normalizes menstruation28. Thus, with six wk to one year of uncomplicated oral treatment for hypothyroidism, 76.6 per cent of infertile women had attained conceivement19. Infertile women with subclinical hypothyroidism (SCH) are justified in initiating thyroid replacement medication at an early stage. The infertile women may benefit significantly from a proper diagnosis and treatment of hypothyroidism rather than undergoing an unnecessary battery of radiological and biochemical investigations including costly invasive procedures.
Thyroid problem has been linked to infertility, presumably as a result of abnormal menstrual cycles. ATA recommends testing TSH for all women considering infertility therapy, with levothyroxine prescribed for overt hypothyroidism28. The task force also suggested that there is insufficient evidence to determine whether levothyroxine can improve fertility in subclinical hypothyroidism. However, states that treatment with a low dose of levothyroxine may be considered in this setting given its ability to prevent progression to more significant hypothyroidism once pregnancy is achieved5,6,8.
This study also observed a non-significant increase in the frequency of hypothyroidism with advancing publication year of articles. This finding may not be excluded from type II error due to insufficient number of studies. Due to change in lifestyle and socioeconomic factors there is a possibility of increase in the prevalence of hypothyroidism in women with infertility. The high proportion of hypothyroidism in the Indian population demands the rigorous screening of TSH levels in infertile women. The findings of the present study will also help policy makers for considering TSH screening for all the Indian women with infertility including primary, secondary and tertiary care hospitals.
This review was not without some limitations. The included studies have used the variable cut-off values for thyroid profile parameters. Additionally, pre-analytical factors such as type and duration of infertility, thyroid antibody status, iodine status, different states and timing of TSH sample collection could have altered the results. Different immunoassays used across the selected studies could have produced variable TSH readings, casting doubt on the reproducibility and repeatability of tests. Most of the studies did not mentione that technicians who conducted the TSH test were blinded to the diagnosis of patients or not. Findings of the meta-analysis were limited by the availability of single studies from many States like Meghalaya, Telangana, West Bengal, Andhra Pradesh, Bihar, Jharkhand, Punjab and Rajasthan, which could have limited the reliability and precision estimates of the prevalence of hypothyroidism in women with infertility from different States. Therefore, there is a clear need to conduct more studies for generalizability of these findings of across different States of India. The finding of the current meta-analysis could also have been limited by methodological flaws in the included studies.
Overall, we observed that the studies from India reported significant proportion of hypothyroidism in women with infertility. More studies from different States of India are needed but based on rigorous methodological quality to generalize the finding in the entire population. TSH test may be considered in the screening test of women visiting a health care facilities for infertility treatment.
Financial support & sponsorship
None.
Conflicts of Interest
None.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
References
- Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III) J Clin Endocrinol Metab. 2002;87:489-99.
- [Google Scholar]
- Childlessness in time, space and social groups and its linkages with fertility in India. In: European Population Conference. 2006.
- [Google Scholar]
- Thyroid dysfunction and autoimmunity in infertile women. Thyroid. 2002;12:997-1001.
- [Google Scholar]
- Correlative study of prolactin level and hypothyroidism in both primary and secondary infertility in females of Uttar Pradesh. Indian J Public Health Res Dev. 2019;10:138-41.
- [Google Scholar]
- Evaluation of thyroid and prolactin levels and its correlation in patients with infertility. Int J Med Health Res. 2018;4:126-8.
- [Google Scholar]
- Study on thyroid hormone, FSH, LH and prolactin levels in patients with primary infertility: A Hospital based study. J Med Sci Clinical Res. 2016;4:11435-8.
- [Google Scholar]
- Prevalence of hypothyroidism in infertile women and evaluation of response of treatment for hypothyroidism on infertility. Indian J Endocrinol Metab. 2015;19:504-6.
- [Google Scholar]
- Correlation of prolactin and thyroid hormone concentration with menstrual patterns in infertile women. J Reprod Infertil. 2009;10:207-12.
- [Google Scholar]
- Serum gonadotropin and prolactin levels in females with primary infertility and thyroid dysfunction in North Indian population. J Infertility Reprod Bio. 2014;2:88-91.
- [Google Scholar]
- Association of obesity with hormonal imbalance in infertility: A cross-sectional study in North Indian women. Indian J Clin Biochem. 2013;28:342-7.
- [Google Scholar]
- Correlation of thyroid hormones with FSH, LH and prolactin in infertility in the reproductive age group women. Int J Clin Biochem Res. 2015;2:216-22.
- [Google Scholar]
- Study of serum TSH and prolactin levels in patients of female infertility. Int J Recent Trends Sci Technol. 2013;9:144-45.
- [Google Scholar]
- The association of thyroid profile with primary infertility in females. Int J Health Sci Res. 2012;1:90-4.
- [Google Scholar]
- Correlation of thyroid-stimulating hormone and prolactin levels in non-pregnant female. Asian J Pharm Clin Res. 2020;13:147-8.
- [Google Scholar]
- Correlation of thyroid hormones with FSH, LHlh and prolactin in infertility in the reproductive age group women. IAIM. 2016;3:146-50.
- [Google Scholar]
- Association of thyroid disorders in females with primary infertility attending a tertiary-care hospital in northeast India. Int J Med Sci Public Health. 2016;5:1724-26.
- [Google Scholar]
- Female infertility risk assessment in relation to serum thyroid hormone levels and serum prolactin levels. J Cont Med A Dent. 2020;8:52-6.
- [Google Scholar]
- Prevalence of hypothyroidism in infertile women and evaluation of response of treatment for hypothyroidism on infertility. Int J Appl Basic Med Res. 2012;2:17-9.
- [Google Scholar]
- Study of thyroid hormones with LH, FSH and prolactin in tribal infertile women of reproductive age group at RIMS, Ranchi, Jharkhand. IOSR J Dental Med Sci. 2020;19:20-3.
- [Google Scholar]
- Evaluation of serum prolactin, FSH and LH in infertile females with thyroid disorders. JIGIMS. 2020;6:18-20.
- [Google Scholar]
- Prevalence of hypothyroidism in infertile women attending a tertiary care centre in West Bengal, India - a prospective observational study. J Evid Based Med Healthc. 2021;8:556-61.
- [Google Scholar]
- Study of correlation of thyroid profile and clinical parameters in patients with infertility. Int J Reprod Contracept Obstet Gynecol. 2016;5:1410-13.
- [Google Scholar]
- Association between lifestyle and thyroid dysfunction: A cross-sectional epidemiologic study in the She ethnic minority group of Fujian Province in China. BMC Endocr Disord. 2019;19:83.
- [Google Scholar]
- Study of thyroid profile and prolactin levels in female infertility patients: An Institutional Analysis. J Scientific Soc. 2021;48:13-6.
- [Google Scholar]
- Thyroid disease and reproductive dysfunction: A review. Obstet Gynecol. 1987;70:789-98.
- [Google Scholar]
- GnRH pulsatility, the pituitary response and reproductive dysfunction. Endocr J. 2009;56:729-37.
- [Google Scholar]
- Clinical practice guidelines for hypothyroidism in adults: Cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract. 2012;18:988-1028.
- [Google Scholar]






